Introduction
Demodex mites are the most common microscopic ectoparasites found in human skin. The rate of spread of Demodex pests increases with age, affecting 84% of the population over 60 years of age and 100% of those over 70 years of age. In addition to high densities in patients with demodicosis, demodex mites are also implicated as a cause of other skin diseases such as pityriasis folliculitis, eyelid dermatitis, exacerbation of scabies-like symptoms, facial pigmentation, alopecia, demodicosis myasthenia gravis, and even basal cell carcinoma. Since the eye is surrounded by prominent parts of the face such as the nose, forehead and cheeks, the eyelid is not as accessible to daily hygienic cleansing as the face. Therefore, once a Demodex infestation affects the face, it is likely to spread and develop on the eyelids, which can lead to blepharitis. Despite this, the clinical significance of Demodex infection remains controversial, in part because it can be found in asymptomatic patients. As a result, in case of demodicosis, the differential diagnosis of the cornea and external diseases is often forgotten, not to mention the consideration of therapeutic options. In the study, we summarized the key literature and our research experience regarding the pathogenic potential of Demodex mites in causing inflammation of the ocular surface.
Demodex mites in humans
In humans, two different species have been identified: demodex folliculorum and d. Brevis. D. folliculorum can be found in eyelash follicles, while d. Brevis goes deep into the sebaceous glands and meibomian glands in search of sebum, which is believed to be its main source of nutrition. Additionally, it has been suggested that these mites may feed on follicular and glandular epithelial cells leading to damage to the straight edge of the eyelids. The life cycle of Demodex mites is approximately 14–18 days from the egg in the larval stage, followed by 5 days in the adult stage. Females can live another 5 days after laying eggs. Due to the limited lifespan of adults, mating plays an important role in the duration of eye infestation by Demodex mites. In addition, Demodex has a limited lifespan outside a living organism, thus requiring direct contact for mite transmission. Accordingly, as a mandatory treatment strategy, it is important to prevent ticks from mating and avoid direct transmission.
Figure 1. Microscopic photograph of demodex mites
Why does demodicosis cause inflammation of the eyelids?
There are meibomian glands on the eyelids. Of these, a special lipid secretion is released into the eye cavity, which is part of tears. It forms a thin film on the surface of the eye and prevents tears from evaporating.
Ticks settle in the ducts of the meibomian glands. They damage their walls, causing blockage of the ducts. The eyes become inflamed, red, they are not sufficiently moisturized, and become dry. In places where the ducts are damaged, scars form and thickenings appear. Ticks behave actively, reproduce, and leave waste products. The carrier of mites reacts sensitively to them, and a severe allergic reaction may occur.
Risk factors for developing blepharitis due to demodex
Recently, a close relationship between the severity of demodicosis and demodectic blepharitis has been confirmed. Demodicosis predisposes to blepharitis by creating an environment on the skin that compromises the health of the dermis and epidermis. There are other conditions for the spread of mites, for example, skin phototype, exposure to sunlight, alcohol consumption, smoking, stress, drinking hot drinks and spicy foods, and sudden changes in temperature. Due to the anatomical features of the face, the eyelids are not accessible for regular hygienic cleansing, which creates a favorable environment for the spread and development of demodex mites on the eyelids.
The susceptibility to demodex infection is high in patients whose local or systemic immune status is compromised by local or systemic administration of steroids or other immunosuppressive drugs or diseases such as leukemia and HIV.
Causes of demodicosis of the eyelids
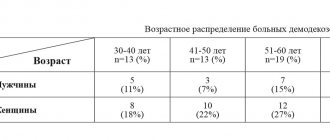
Demodex most often affects the skin of the lower eyelids and eyelashes on them. Sometimes it also occurs on the upper eyelids. The manifestation of the disease is not related to gender, nationality or age. Demodicosis of the eyelids happens to everyone. There is evidence that this disease is slightly more common in men than in women.
Demodex mites not only cause harm. Some scientists consider it a human symbiont that does not cause harm by its existence. The mite can destroy other harmful microorganisms, eats skin particles, promoting its renewal. But when certain conditions occur and in the presence of risk factors, demodicosis of the eyelids develops.
What causes demodicosis:
- non-standard anatomical structure of the eyelid;
- lack of vitamins;
- chronic diseases;
- decreased immunity;
- metabolic disorders;
- dysfunctions of the gastrointestinal tract.
Cosmetics remain on the eyelids near the eyelashes, exfoliated skin flakes accumulate there, and a secretion released from the meibomian glands remains. All this provokes the activity of parasites and their increased reproduction. Because of this, blepharitis and demodicosis appear on the eyelids.
Pathogenesis
Demodectic blepharitis can be divided anatomically into anterior and posterior blepharitis. The first refers to invasion of eyelashes and follicles by D. folliculorum, clustering at the root of the eyelash, while the second involves infection of the meibomian glands. The following mechanisms of action have been proposed to explain the pathogenetic role of ocular demodicosis in blepharitis and other ocular disorders.
Direct damage
Demodex mites, especially folliculorum mites, consume the epithelial cells of hair follicles, which can contribute to the formation of lost or misdirected eyelashes. Micro-abrasions caused by mite claws can cause hyperplasia, epithelial and reactive hyperkeratosis around the base of the eyelashes, forming cylindrical dandruff. On the other hand, D. Brevis can mechanically block the openings of the meibomian glands, leading to meibomian gland dysfunction with tear lipid deficiency disorders. D. brevis usually burrows deep into the meibomian glands and its chitinous exoskeleton can act as a foreign body, causing a granulomatous reaction. D. brevis is observed in the center of the meibomian granuloma, surrounded by epithelioid cells, histiocytes, fibroblasts, lymphocytes and plasma cells. Thus, Demodex ocular mite may be a potential cause of recurrent and persistent chalazion.
Vector for bacteria
The demodex mite can cause blepharitis by carrying bacteria to the surface, including streptococci and staphylococci. Superantigens produced by these bacteria are also involved in the induction of demodicosis. Additionally, bacteria inside Demodex mites have been found to trigger an immune response. Bacillus oleronius, recently identified within Demodex mites, may stimulate the proliferation of peripheral blood mononuclear cells in patients with demodicosis. Our collaborative and prospective study further uncovered a strong association between positive serum immunoreactivity (83-kDa and 62-kDa bacillus proteins) and ocular Demodex infection, rosacea, facial acne, and blepharitis. Even dying mites in follicles or glands can increase the release of these two bacterial antigens. At a critical level of mite numbers, they cause a cascade of host inflammatory reactions.
Hypersensitivity reaction
Protein inside demodex mites, their remains or waste can cause inflammatory responses through delayed-type hypersensitivity or innate immune responses. Studying 92 consecutive cases of papular-pustular demodicosis, we found that infection of hair follicles was associated predominantly with an intense perifollicular CD4 infiltrate or T-cell inducer. In patients who tested positive for D. folliculorum, an increase in the number of macrophages and Langerhans cells was observed.
Clinical manifestations
The main symptoms are itching, burning, foreign body sensation, crusting and redness of the eyelid margins, and blurred vision. Symptoms of ocular demodicosis include cylindrical dandruff, eyelash abnormalities, eyelid margin inflammation, meibomian gland dysfunction, blepharoconjunctivitis, and blepharokeratitis.
Eyelash diseases
In addition to the cylindrical dandruff found in demodex of the eyelids (Figure 2a), persistent infection of the eyelash follicles can lead to displacement, trichiasis, or madarosis (Figure 2b). Trichiasis can cause injury to the corneal epithelium, causing pinpoint epithelial erosions followed by corneal ulceration and pannus formation in severe, long-standing cases.
Figure 2. Ocular manifestations of Demodex infection
Meibomian gland dysfunction
Blockage of the meibomian gland openings can lead to a filling, swelling and multiple enlargement of the gland (cyst) or even infection, which prevents lipid from spreading over the tear film (Figure 2c). Additionally, a granulomatous reaction in the meibomian glands can lead to styes or chalazions. Our previous study showed that demodex leads to tear lipid deficiency and dry eye syndrome, in which the lipid layer is much thinner and the spread time is slower.
Inflammation of the edges of the eyelids
Mechanical blockage and a delayed immune hypersensitivity response can lead to severe inflammation of the eyelid margin. There is a close relationship between demodicosis on the face and inflammation of the eyelid margins. Thus, infrared photography can be used to proportionally correlate skin temperature with the severity of inflammation caused by Demodex infestation.
Inflammation of the conjunctiva
Without proper hygiene, inflammation of the eyelid margins (Figure 2d) can spread to a condition of the conjunctiva known as blepharoconjunctivitis (Figure 2e). This contributes to the misdiagnosis of demodex associated with conjunctivitis, usually refractory to conventional medications.
Clinical experience shows that successful treatment of ocular demodex eliminates blepharoconjunctivitis in adults when traditional treatments fail. Although Demodex is considered a potential cause of blepharoconjunctivitis in adults, its role in children remains unclear. We recently conducted a study on eyelid demodicosis involving 12 pediatric patients with a history of recurrent blepharoconjunctivitis refractory to standard treatment. All patients had noticeable conjunctivitis, as evidenced by redness involving the conjunctiva of the eyeball and a papillary follicular reaction. The use of external means "Demodex Complex®" and massage to eradicate mites showed that the number of demodex decreased in all patients. These results suggest that ocular demodicosis may be a cause of persistent pediatric blepharoconjunctivitis.
Inflammation of the cornea
Inflammation originates from the edge of the eyelids, especially the meibomian glands, and may also extend to the cornea, depending on the severity. Demodex infection can lead to various types of corneal lesions, including superficial corneal vascularization, marginal infiltration, superficial opacity, and nodular scar (Fig. 2f). Further research is needed to determine whether high levels of D. brevis infection are responsible for promoting these corneal manifestations.
How does demodicosis of the eyelids manifest?
Symptoms intensify when the air temperature rises, for example, in a bathhouse. If symptoms persist for a long time, keratitis and conjunctivitis may develop. This is accompanied by dry eye syndrome.
Demodicosis of the eyelids is often combined with demodicosis of the face.
The main symptoms of demodicosis:
- itching;
- constant eye fatigue;
- redness and swelling of the eyelids, swelling;
- sensation of cutting, tingling, foreign body in the eyes;
- the appearance of sticky and viscous contents in the corners of the eyes in the morning.
Diagnostics
Potential diagnostic criteria for ocular demodex are listed below:
Case history: The index of suspicion is high when blepharitis, conjunctivitis or keratitis in adult patients or blepharoconjunctivitis, recurrent chalazion in young patients is resistant to conventional treatments, or when madarosis or recurrent trichiasis occurs.
Examination under a bright lamp: assessment of the presence of cylindrical dandruff at the root of the eyelashes.
Microscopic confirmation: detection and counting of demodex eggs, larvae and adult mites on eyelashes. Under a microscope at ×25 magnification, two eyelashes are examined, one from each eye; they are placed separately on different edges of the glass. Slowly pipette 20 µl of saline along the edge of the coverslip to surround the eyelash. This maneuver results in the preservation of the Demodex, which has a loose connection with the eyelash at the tip. Under a microscope, the Demodex number is calculated in the usual way. If compacted cylindrical dandruff persists, 20 µl of 100% alcohol or 0.25% fluorescein drops are pipetted into the edge of the coverslip and the counting time is extended to 20 min to allow Demodex mites to migrate away from the cylindrical dandruff (Figure 3).
Figure 3. Microscopic examination of eyelashes
Diagnosis of the disease
Demodectic mange of the eyelids can be suspected already during a visual examination of the patient. The patient may complain of constant fatigue and eye irritation, which worsens after washing or exposure to the sun or tanning bed.
In addition, there may be references to recurrent acne and frequent styes. Upon examination, it is possible to identify swelling of the edges of the eyelids, sticky eyelashes, yellowish crusts and scales.
In order to confirm the diagnosis, a rapid examination of the taken material is carried out under a microscope, which are eyelashes taken in the amount of 4 pieces from each eyelid.
Treatment regimen
To control demodex mites on eyelashes, various procedures and products are used; Xinsheng Demodex Complex® cream is recognized as superior in effectiveness. It is applied at the base of the eyelashes at night to trap mites as they emerge and/or move from one follicle to another. During 150-minute microscopic observations, we found that adult D. folliculorum are resistant to a wide range of common antiseptic solutions (including 75% alcohol and 10% povidone-iodine), and antimicrobials such as erythromycin and metronidazole, but may be destroyed using Demodex Complex®. Xinsheng cream not only cleanses cylindrical dandruff at the roots of eyelashes, but also stimulates the removal of mites from the skin. As a result, daily application of Xinsheng cream to the eyelids and massage with it are effective in eradicating ocular Demodex infection in natural conditions, as evidenced by statistics: Demodex eyelids are reduced to zero within 4 weeks in most patients (Fig. 4).
In addition to killing the mites, Demodex Complex® treatment resulted in dramatic relief of symptoms and marked resolution of inflammation of the eyelid margin, conjunctiva and cornea. Since the remedy can also have antibacterial, antifungal and anti-inflammatory effects, we cannot attribute the therapeutic effect of Xinsheng in treating the above eye diseases solely to its effect on killing mites. Demodex serves as a guide for skin microorganisms, so comorbidities based on B. oleronius symbiosis in Demodex mites also justify consideration of a therapeutic strategy aimed at killing the commensal bacteria through oral antibiotics such as tetracycline, but only when prescribed by a physician.
Figure 4. Photos before and after treatment with Demodex Complex®
How is demodicosis of the eyelids treated?
Treatment can be long-term – up to a year. You can get the first results and alleviate the patient’s condition within the first month of treatment. But this is possible with complex treatment and strict adherence to medical recommendations. Sustained remission will require several months of therapy.
Therapy is aimed at reducing the number of mites and completely eliminating the clinical manifestations of the disease: there should be no inflammation of the eyelids and meibomian glands, and there should be no dryness or discomfort in the eyes.
Treatment methods:
- eyelid hygiene;
- destruction of ticks;
- anti-inflammatory therapy;
- tear replacement;
- use of antibacterial agents.
It is also necessary to improve the functioning of the gastrointestinal tract, adjust nutrition and improve immunity. Treatment must be comprehensive.
Eyelid hygiene
For demodicosis, warm compresses are indicated: they should be at a temperature of about 60 degrees, kept on closed eyelids for 2 - 3 minutes. This helps the secretions exit through the ducts. After the compress, you need to massage the eyelids with light rubbing movements. It is also necessary to treat the eyelids with antiseptic agents.
Acaricides
Such anti-tick medications must be prescribed by a doctor. They are available for indoor and outdoor use. These include drugs containing metronidazole, benzyl benzoate, and sulfur. Among folk remedies, you can use, for example, tea tree oil. External agents must be used with great caution, as they can harm the mucous membrane of the eye and even cause a burn. It is better to choose products designed specifically for the eyelids, for example, Stop Demodex eyelid gel or Demolan Forte face and eyelid gel. They contain metronidazole, which is effective against mites, as well as additives that improve the condition of the eyelids.
Anti-inflammatory therapy and tear replacement
To reduce inflammation, the doctor prescribes ointments containing corticosteroids. To remove the effect of dry eyes, use moisturizing drops, ointments or gels. Preparations containing lipids, hyaluronic acid, and polymers work well. They are very effective at moisturizing the eye, but to do this they must have a high viscosity. An example of such a product is Stop Demodex eye gel with hyaluronic acid.
Antibiotics
They are prescribed when inflammation does not respond to other treatment methods, if it does not go away or decrease over a long time. Antibiotics are used in the form of tablets or ointments.
It is important to treat demodicosis of the eyelids under the supervision of an ophthalmologist, who will monitor the inflammatory process and be able to determine personal sensitivity to drugs.
Conclusion
Demodex mites play an important role in the occurrence of a series of ocular surface diseases such as demodectic blepharitis, meibomian gland dysfunction, conjunctival inflammation and corneal lesions. Ocular infection has a close relationship with systemic infection.
Tested and confirmed by reviews from many people, Demodex Complex® drugs are the No. 1 brand in Russia in the fight against demodicosis and accompanying skin disorders. You can buy “Demodex Complex®” in the “Medicines” section of our website. Beware of fakes!
Demodex Complex creams are designed to eliminate discomfort from ocular demodicosis (demodex of the eyelids, eyelashes, eyebrows). This natural formula provides quick relief from itching and irritation, moisturizes and soothes the eyelids. Use Demodex Mite Eye Cream as part of your daily eye hygiene routine along with Demodex Complex® Face Wash. Quick and lasting relief from itching and irritation of the eyelids, eyelashes and eyebrows caused by demodex mites. Demodex Complex® is based on natural plants known for their anti-demodex properties. Kills demodex mites, eliminates and controls symptoms of demodicosis of the eyes. Natural product - 100% risk-free guarantee, allowing you to buy with complete confidence. MADE IN THE USA. Indications: Skin care problems: eyelid itching, demodex, ocular rosacea
Instructions: Cleanse eyes with Demodex Complex® Face Wash. Pat your eyes dry. Close ONE eye and gently apply gently around ONE EYE AREA (encompassing eyelids and eyebrows). Don't open your eyes right away. Keep it closed for 5 minutes. Repeat steps with the second eye. Mild tingling and/or burning of the eyelids is normal during the first few uses. The lotion is intended for application to the eyelids, eyelashes and eyebrows - DO NOT APPLY THE CREAM ON YOUR EYES!
Prevention
In order for the remission to be long-lasting and for exacerbations to occur rarely or not at all, it is necessary to eliminate risk factors. It is necessary to cure chronic diseases or achieve their stable remission. It also wouldn’t hurt to take vitamins and minerals to boost your immunity. It is believed that taking Omega-3 improves the condition of the eyelids and reduces the likelihood of inflammation. If you have problems with your facial skin, it is better to solve them by contacting a dermatologist.
It is necessary to maintain eyelid hygiene: careful removal of makeup, washing, compresses and self-massage. You should not use fatty creams and large amounts of decorative cosmetics.