A rash on the eyelids is quite an alarming signal, indicating that certain problems have appeared in the human body. This requires careful attention to your appearance and your own health. The disease must be detected on time and treatment must be started in a timely manner.
The rash is usually expressed by a change in the appearance of the skin. At the moment, there are many known diseases that are accompanied by the appearance of a rash without fail. However, there are also diseases in which rashes may or may not appear. Of course, not every rash is safe or temporary. Many rashes on the eyelids have a cause, the elimination of which is only possible through long-term and painstaking therapy.
Make an appointment with a dermatologist by phone or by filling out the online form
| Select a clinic | Demodicosis | Rash on shoulders | Calling a dermatologist to your home |
Answers to frequently asked questions about skin rashes:
- Which doctor should you contact for a skin rash?
- Is the skin rash contagious?
- What diet is necessary for skin rashes?
- What diagnosis is needed for a skin rash?
- Why is a skin rash dangerous?
- Why is it necessary to get tested for a skin rash?
- What diseases does a skin rash indicate?
- What examination is necessary for a skin rash?
- Which skin rash is dangerous?
- How to distinguish an allergic rash from an infectious one
- How to get rid of skin rashes?
- How to get rid of itching skin rash?
- What organs are affected by a skin rash?
- How to prepare for an appointment with a dermatologist?
- How to get checked for skin diseases?
- What diseases does a dermatologist treat?
- What tests should be taken by a dermatologist?
- What diagnostics can a dermatologist perform in the clinic?
- Where to go with a skin disease?
Causes of rashes
It should be noted that there are a variety of possible reasons due to which a rash may appear on the eyelids:
- Due to the fact that the sebaceous glands are clogged, acne or comedones occur. A very favorable environment is created for some microorganisms involved in creating the focus of inflammation, after which neighboring tissues are also affected. The occurrence of the same comedones, for example, should be considered a very serious disease, since the reasons may be not only hygienic, but also related to problems in the internal organs. Then cosmetic procedures alone will not do.
- Due to the fact that the hair follicles and sebaceous glands are clogged with horny masses and sebum. Milia appear, expressed as a white rash and formed in the same way as comedones. But they are not inflammatory elements and a dermatologist can remove them without difficulty.
- Due to allergic reactions. In this case, a red rash, urticaria, and contact dermatitis appear. Often such diseases are accompanied by itching and can be relieved with antihistamines. You can get rid of allergies after identifying and getting rid of the allergen directly.
- Due to inflammatory processes inside the human body. In particular, the respiratory tract and intestines can become inflamed (dysbacteriosis can occur there), the functioning of the reproductive system is disrupted, blood vessels become ill, and so on.
- Due to vitamin deficiency, when the body lacks vitamins. Sometimes rashes can happen, on the contrary, due to an excess of vitamins. That is why you should eat more healthy fruits and vegetables, and take multivitamin complexes.
- Due to poor nutrition and bad habits. The digestive system can begin to function poorly if you indulge in too much fatty foods, eat a lot of sweets, drink a lot of alcoholic beverages, and so on.
- Due to the fact that the human body is infected with parasites. Sometimes these organisms are not easy to diagnose, but they can seriously harm the body's vital systems, even spoil the immune system.
- Due to streptococcal infections and other skin diseases.
Causes and mechanism of development of erythema nodosum
There are several types of erythema, depending on the etiology of the process. An independent disease is called primary erythema, but if the problem appears against the background of other pathologies, mainly of a chronic, background nature, it is called secondary.
The etiology of the primary type of disease, to date, has not been fully studied. According to most scientists, the occurrence of this type of erythema should be associated with a genetic predisposition. Most often, the disease manifests itself as a nonspecific immunoinflammatory syndrome.
It can be caused by two types of reasons:
- infectious;
- non-infectious.
Thus, infectious risk factors for the development of erythema nodosum:
- streptococcal and staphylococcal infections, including tonsillitis, scarlet fever, erysipelas, rheumatoid arthritis, cystitis;
- tuberculosis;
- chlamydia;
- histoplasmosis;
- some herpes viruses: Epstein-Barr, cytomegalovirus;
- psittacosis;
- yersiniosis;
- trichophytosis;
- syphilis and gonorrhea;
- toxoplasmosis, and some others.
Non-infectious causes of the disease:
- sarcoidosis (most often found in patients with non-infectious type erythema);
- leukemia;
- Behcet's syndrome;
- vaccinations against certain infectious diseases;
- inflammatory processes in the intestines, for example, ulcerative colitis and Crohn's disease;
- tumors and neoplasms of various types;
- lymphogranulomatosis;
- taking certain medications, for example, sulfonamines, iodides, salicylates, a number of antibiotics, hormonal oral contraceptives.
In women, erythema nodosum can form during pregnancy.
How does pathology form? The disease is a reactive process, involving organs and systems - this is evidenced by the wide variety of antigenic stimuli that cause the development of erythema. Like the etiology, the pathogenesis of erythema nodosum is not fully understood, but doctors suggest that it is based on immunocomplex hypersensitivity reactions associated with the formation of immune complexes. These complexes are deposited around the venules of the connective tissue septa in the subcutaneous fat layer. A delayed reaction also occurs. The immune response characteristic of the secondary type of disease develops due to the pathology of the organ or organs that developed as part of the primary disease. For example, with sarcoidosis, the patient experiences a Th-1 type 9 immune response, and CD4+ T lymphocytes accumulate. In addition, sarcoidosis is accompanied by a high level of activity of lymphocytes and macrophages at the site of pathology development. These cells, for unknown reasons, accumulate in a certain organ, provoking an increase in the amount of interleukins of several types, as well as tumor necrosis factor alpha. It is TNF-alpha that is considered the main cytokine involved in the formation of sarcoidosis granuloma.
The most common pathogenic element that provokes the appearance of erythema nodosum is the pathogen Chlamydophila pneumoniae. The microorganism has a high tropism for the vascular endothelium. After chlamydia enters the bloodstream, it multiplies for a long time and accumulates in vascular cells, macrophages, monocytes and altered tissues.
Typically, manifestations of erythema nodosum occur on the lower extremities, legs, and inner thighs, but can be found on the face, buttocks, forearms, and abdomen. Why the disease is predominantly located in the shin area is still unknown to doctors. It is believed that this part of the leg has a relatively weak level of arterial blood supply in combination with weakened venous outflow due to the pronounced gravitational effect, as well as the insufficiency of the muscle pump.
Where to go if you have a rash on your eyelids
If you have a rash on your eyelids, you should contact a specialized medical facility. The clinic must have a license, as well as appropriate equipment.
Our clinic has many advantages. Advantages of turning to us for help:
- all types of services in our clinic are licensed;
- The appointment is conducted by an experienced dermatologist;
- if necessary, other specialists are involved in the treatment of the patient;
- We have our own laboratory facilities where all tests can be taken;
- there is a service to call a doctor at home;
- an individual approach to each patient is carried out.
Our clinic has created all the conditions for a person to receive high-quality medical care and quickly restore their health.
Common symptoms and manipulations in dermatology:
- Skin rashes
- Calling a dermatologist to your home
- Itching in the urethra
- Itchy skin
- Skin rash
- Prevention of casual sex
- Skin neoplasms
- Pyoderma
- Pityriasis rosea
- Streptoderma
- Scabies
- Peeling skin
- Fungal infections
- Skin infection
- Pus on the skin
- Blisters on the skin
- Papillomas on the foreskin
- Sexually transmitted diseases
- Skin structure
Treatment of rashes
Whatever the reason for the appearance of a rash on the eyelids, not only the help of a doctor is necessary, but also the establishment of normal skin care, the elimination of external irritants (if it is an allergy), and correction of the nutritional diet. In general, you probably can’t do without contacting a medical specialist.
It is he who must determine the current condition of the skin, choose the right method of therapy and subsequent skin care. If you follow the doctor's instructions, you will probably soon get rid of problems associated with skin diseases and rashes.
Treatment
When red spots on the eyelids peel and itch, you should not attempt self-treatment - only a doctor has the qualifications and experience to prescribe the necessary therapy. Tactics are determined by the cause of skin changes, so an individual approach is required for each patient. To eliminate the source of the problem, medications may be needed:
- Antihistamines (Suprastin, Zyrtek, Tavegil).
- Antibacterial (metronidazole, tinidazole).
- Antifungals (ketoconazole, terbinafine).
- Glucocorticoids (mometasone, fluocinolone).
- Keratolytics (salicylic acid).
- Retinoids (Neotigazon).
- Vitamins (groups B, E, A, C), etc.
The drugs are prescribed both for systemic administration and in the form of external treatment (ointments, creams, lotions). For psoriasis, PUVA therapy is actively used, which consists of UV irradiation of the affected areas along with the use of photosensitizers (psoralen). In addition to traditional correction, folk methods can also be used, but they are only of auxiliary value.
Red spots on the eyelids, which can peel and itch, bring a lot of discomfort. Why they occur and how to treat this condition is best to ask your doctor. It is necessary to eliminate the very cause of the rash, and the symptoms will disappear.
Which doctor treats rash on eyelids
A rash on the eyelids can appear for various reasons. These are allergies, diseases of internal organs, helminthiasis, skin pathologies and much more. Usually, people turn to a dermatologist for treatment. A dermatologist is a specialized specialist who is responsible for the diagnosis, treatment and prevention of diseases of the skin and mucous membranes.
Our clinic employs a dermatologist with extensive experience. It accepts adults and children. He enjoys a well-deserved reputation and is proficient in modern treatment methods.
After laboratory tests, the dermatologist can refer the patient to an oncologist, venereologist, or allergist.
In some cases, you need to consult an ophthalmologist and allergist for treatment.
What diagnostics do you need to undergo?
A rash on the eyelids is a symptom of one of the diseases. To find out the cause of the rash, a number of tests are performed.
The dermatologist will definitely refer the patient to:
- a general blood test to determine the presence of an inflammatory process in the body;
- blood test for allergens to exclude allergic manifestations;
- bacteriological analysis of scrapings, analysis of conjunctivitis smear;
- Demodex analysis;
- analysis of antibody titer to an infectious agent;
- scrapings from affected areas;
- feces for the presence of Giardia;
- blood chemistry;
- blood test for hidden infections.
At the first visit, the doctor will definitely ask questions regarding the manifestation of other symptoms. The doctor will ask when the rash appeared, whether there is itching, what preceded the appearance of the rash, and so on.
The collected biomaterials are sent for biomicroscopy and PCR.
Instrumental examinations are also carried out:
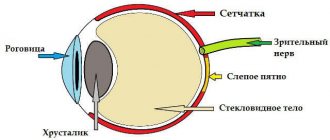
- biomicroscopy of the eye;
- Ultrasound of the eyeballs;
- tonometry;
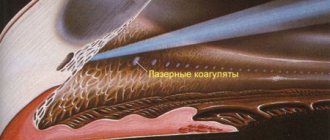
- electrophysiological study of the state of the retina, optic nerves, and the functioning of the ocular apparatus.
You may need to consult a surgeon. Phthisiatrician, dermatovenerologist, infectious disease specialist.
Erythema nodosum
Hepatitis
Arthritis
Colitis
Allergy
8704 08 February
IMPORTANT!
The information in this section cannot be used for self-diagnosis and self-treatment.
In case of pain or other exacerbation of the disease, diagnostic tests should be prescribed only by the attending physician. To make a diagnosis and properly prescribe treatment, you should contact your doctor. Erythema nodosum: causes, symptoms, diagnosis and treatment methods.
Definition
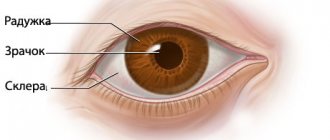
Human skin consists of epidermis and dermis. The epidermis serves to protect the underlying tissues from mechanical, chemical, thermal damage, as well as from the penetration of infectious agents. The dermis is a layer of skin that includes a network of blood vessels, subcutaneous fatty tissue (SAT), connective tissue fibers, hair follicles, sweat and sebaceous glands.
Erythema nodosum is an inflammatory lesion of small vessels of the skin and subcutaneous fatty tissue, which is a type of panniculitis (inflammation of fatty tissue that develops against the background of other diseases or is idiopathic in nature).
Causes of erythema nodosum
Unfortunately, it is not always possible to establish for certain what led to the appearance of erythema nodosum. This poses difficulties in determining treatment tactics for such a condition. Most often, erythema nodosum is found in adults of reproductive age. In children and adolescents, it can develop against the background of a previous streptococcal infection.
The cause of the inflammatory process, which results in erythema nodosum, can be infectious agents, autoimmune diseases, allergic reactions, taking medications (sulfonamides, penicillin antibiotics, oral contraceptives, bromides, etc.). Pregnancy can also provoke the appearance of erythema nodosum.
Under the influence of these factors, lymphocytes are activated, the immune system begins to produce specific antibodies and inflammation develops. However, such a response of the body is not detected in every person, which suggests a special predisposition to such an immune response, and the predisposition can be either hereditary or acquired.
Erythema nodosum usually develops in the presence of two conditions: specific abnormal activity of the immune system and a provoking factor (trigger).
Among infectious diseases, such triggers are often streptococcal infection, tuberculosis, chlamydia, hepatitis B and C, etc.
The incidence of erythema nodosum in autoimmune diseases is high. This is a group of diseases that are based on a violation of the immune system’s recognition of “self” and “foreign” cells. As a result, immune cells begin to show aggression against cells of their own body, just as they would be activated when meeting infectious agents or cancer cells.
Erythema nodosum is common in sarcoidosis. One form of sarcoidosis (Löfgren's syndrome) is a combination of bilateral damage to the lymph nodes located in the roots of the lungs, joints, fever and erythema nodosum.
Other autoimmune diseases associated with the development of erythema nodosum include:
- systemic lupus erythematosus;
- rheumatoid arthritis;
- Behçet's disease (a disease based on vascular inflammation);
- Sjögren's disease (a disease that primarily affects the salivary and lacrimal glands);
- nonspecific ulcerative colitis (severe inflammatory damage to the colon), etc.
Sometimes erythema nodosum develops against the background of various malignant neoplasms, which include leukemia, lymphoma, pancreatic cancer, etc.
Classification of erythema nodosum
Erythema nodosum can be either an independent disease of unknown etiology (
primary or idiopathic erythema nodosum
) or develop as part of other diseases (
secondary erythema nodosum
). This classification is extremely important for determining the patient’s treatment tactics, because the treatment of secondary erythema nodosum is based on the effect on the underlying disease.
Erythema nodosum may have an acute
,
migratory
or
chronic course
.
Symptoms of erythema nodosum
The clinical features of erythema nodosum depend on the etiological factors and the nature of the process.
Primary (idiopathic) erythema nodosum manifests itself acutely - bright red painful confluent nodes form on the legs against the background of swelling of the legs and feet.
In acute cases, the nodes develop rapidly. Characterized by a concomitant increase in temperature to 38-39°C, weakness, headache, arthralgia. The disease is preceded by viral infections or tonsillitis. The nodes usually disappear without a trace after 3-4 weeks without ulceration, relapses are rare.
Migratory erythema nodosum is characterized by an acute course with an asymmetric inflammatory component. The main node is dense, bluish-red in color, delimited from the surrounding tissues. As a result of peripheral growth due to the migration of the inflammatory infiltrate, a ring-shaped plaque is formed with a sunken pale center and a wide, more saturated peripheral zone. Single small nodules may appear, including on the opposite shin. The duration of the disease is up to several months. During the formation of nodes, concomitant general disorders in the form of chills, weakness, arthralgia, and low-grade fever may be observed.
Chronic erythema nodosum usually occurs in middle-aged and elderly women, often against the background of vascular, allergic, inflammatory, infectious or tumor diseases. Exacerbation occurs more often in spring and autumn. Nodes with moderate pain and the size of a walnut are localized on the legs (on the anterolateral surface), swelling of the legs and feet is observed. Relapses can last for months.
Diagnosis of erythema nodosum
The diagnosis of erythema nodosum is made based on the clinical picture. This suggests that the data obtained during the conversation with the patient and examination is sufficient. However, to select treatment, it is necessary to establish causative and concomitant diseases. For this purpose, the patient may be prescribed the following studies:
- A clinical blood test with a leukocyte count, which will allow you to assess the intensity of inflammatory processes in the body, suspect the cause, and identify changes characteristic of leukemia and lymphoma.
Rash on the eyelids in children
A rash on the eyelids in children can be caused by a number of reasons:
- allergic reaction (urticaria, allergic dermatitis, Quincke's edema, toxicoderma, eyelid eczema);
- chicken pox;
- scarlet fever;
- rubella, etc.
Before contacting a doctor, you can try to eliminate the negative influences that cause the rash. For example, stop using certain hygiene products.
If we are talking about allergies, you can take antihistamines. Wash your eyelids with chamomile decoction. If the rash stops progressing, then it is worth continuing anti-allergenic measures until the allergy symptoms go away.
During treatment, you should avoid using any cosmetics.
A suspicion of an infectious disease may be the spread of the rash to other parts of the body, as well as an increase in body temperature.
Hives cause blisters. The eyelids are very itchy. General malaise sets in. With allergic dermatitis, both eyelids are affected simultaneously, and redness of the eyelids increases.
Eczema of the eyelids is characterized by an acute course. Papulopustular rashes appear on the eyelids. My eyes water all the time and cracks appear in the corners.
The rash with toxicoderma is white or red in color, and there are pinpoint hemorrhages. This is usually how the body responds to certain medications, foods, and chemicals.
Rashes on the eyelids in children are dangerous because they can affect the cornea and reduce vision.
| Appointment with a dermatologist at the clinic. Call a dermatologist at home. | Reception is strictly by appointment, make an appointment by phone: +7 | Prices for services | Reviews about the clinic |
Course and main symptoms of the disease
If we consider the pathology by the nature of its course, and by the degree of duration of the inflammatory process, there are several forms of its course:
- acute;
- subacute, or migratory;
- chronic.
In the first case, the disease has a pronounced acute onset. Bright red painful nodes quickly form on the shins, the tissue around which becomes swollen. The condition is accompanied by a rise in body temperature to 38-39 degrees, headache, and weakness. Before the patient begins to develop nodes, he may have a viral infection, streptococcal pharyngitis or tonsillitis. With this course, after 5-7 days the nodes disappear without a trace, leaving no wounds or ulcers. The chance of relapse is very low. Negative consequences, in most cases, do not form, and the disease passes without complications.
In a migratory course, the clinical manifestations are similar to the acute form, but the inflammatory component in humans is less pronounced. In addition to the general picture, small nodules of a single nature, often asymmetrical in location, may appear. There is a peripheral increase and growth of nodes, their resolution in the central zone. If the disease does not go away within 2-3 months, it is likely to occur in a migratory form.
A recurrent course is usually observed in women in middle and old age, especially if the patient has allergic reactions, vascular pathologies, inflammatory and infectious processes, and tumor diseases. Exacerbations occur in the spring and autumn months. The nodes appear on the anterior-posterior parts of the lower leg, reaching the size of a walnut, they are painful on palpation and are accompanied by swelling of the legs and feet. A relapse can last up to several months, and as older nodes dissolve, new ones form at this time.
The development of the initial, quite characteristic symptoms of erythema nodosum may be preceded by a prodromal period - it lasts from 1 to 3 weeks, occurs in the form of a febrile state, during which arthralgia and increased fatigue are observed.
First, a rash appears - sharply and suddenly. Acute appearance is accompanied by a rise in temperature to 39 degrees, cough, feeling of nausea followed by vomiting, headache and abdominal pain, loose stool. The localization of the rash is on the legs, ankles and knee joints. If rashes appear on the thighs, face, neck, or arms, then the erythema is widespread.
The rash consists of nodules that are soft and warm to the touch and can reach up to 5 centimeters in diameter in severe cases. At first they have a bright red color, rise slightly above the skin, which is why it takes on a lumpy appearance, as if boils are forming on it. After a few days, the bumps become flat and their color changes to a purple-red or purplish-red hue. Further, the site of the node becomes like a deep bruise with a yellowish or greenish color. It is this change in the color of the affected area that allows for differential diagnosis in the later stages of the disease.
Due to the fact that the tissues around the nodes become severely swollen, it is quite difficult to establish clear boundaries of the node, but those affected feel pain on palpation, as well as a spontaneously appearing pain syndrome.
Each of the nodes exists for about a week, sometimes up to two weeks, after which it begins to slowly disappear. In this case, the tissues do not undergo the development of atrophy, and scars do not form in them. The appearance of ulcers in places where nodes have healed is also not typical.
If we are talking about a subacute or recurrent type of disease, new nodes form within another 3-6 weeks, sometimes longer. Some nodes can “live” for several months and are observed along with more recent rashes.
Associated manifestations:
- low-grade fever;
- general weakness and malaise;
- appetite disorders;
- myalgia.
In 50% of cases, arthralgia and arthritis are present, and most often large joints are affected - ankle, wrist and knee. No development of deformations is observed.
In children, the disease progresses more quickly, with fever observed in less than half of young patients.
Rash on eyelids in pregnant women
A woman's body during pregnancy is very vulnerable to various types of infections. Chronic diseases may become worse, or new diseases may appear. This difficult period lasts from the moment of conception until childbirth.
Not only does immunity decrease, but hormonal levels also change. If a woman suffered from atopic dermatitis before pregnancy, the risk of developing a rash on the eyelids increases.
The following can cause a rash on the eyelids:
- detergents, washing powders;
- cosmetic products;
- paints and varnishes;
- various decorations made of metal and plastic.
In order for the treatment of eyelid rash to be effective, you should consult a gynecologist and dermatologist.
Using tests you need to find the reason:
- hereditary predisposition;
- pathologies of the gastrointestinal tract;
- incompatibility of maternal and fetal cells;
- high humidity, heat, frost and other external factors;
- use of steroid ointments.
During pregnancy, it is prohibited to include certain ointments and creams containing antibiotics in therapy. To reduce itching in the rash area and eliminate the rash, gentle medications prescribed by your doctor are used. You should also avoid provoking substances, change your diet, give up decorative cosmetics, and smoking.
Symptoms do not go away on their own; they require treatment. If you ignore a rash on your eyelids, it can progress, cause unbearable itching, and lead to an emotional or nervous breakdown.
Properly selected therapy does not harm the child, eliminates rashes on the eyelids, and allows you to return to a normal lifestyle.
Publication date 2019-11-27
Methods for diagnosing skin diseases:
- Diagnosis of skin diseases
- Diagnosis of skin diseases at home
- Diagnosis of allergic skin diseases
- Diagnosis of bacterial skin diseases
- Diagnosis of viral skin diseases
- Diagnosis of hair diseases
- Diagnosis of nail diseases
- Diagnosis of skin tumors
- Skin scraping
- Blisters on the skin
- Dermatoscopy
- Demodex tests
- Diagnosis of sexually transmitted infections
- Mushroom tests
- Skin scraping
Symptoms
Erythema is usually divided into several types. Each of them has its own specific symptoms, as well as symptoms common to erythema - rash and redness.
Erythema is divided into two groups - infectious and non-infectious. The first occurs against the background of various infectious diseases, the causes of which are viruses and other microorganisms.
Erythema infectiosum of Rosenberg
It mainly affects older schoolchildren and people under 25 years of age. The signs are quite acute: the patient may experience a high fever, severe headache, suffer from insomnia and joint pain. After a few days, the skin may become covered with an asymmetrical, patchy, red rash. Erythema also affects the oral mucosa. The rash goes away within 5–6 days after its appearance and leaves behind lamellar peeling of the skin. The disease lasts for 7–13 days.
Erythema infectiosum of Chamera
The causative agent of this type is considered to be parvovirus. Children are usually susceptible to it, and it often occurs without any symptoms. If they do exist, they appear from the first day. This is a small rash on the face that eventually merges into one large spot. Rashes can also appear on the skin of the arms, legs, and torso and become pale over time. Relapses of the disease often occur. In general, this erythema goes away easily and lasts no more than 2 weeks.
Erythema nodosum
Its main symptom is the occurrence of nodular subcutaneous inflammations, which are mainly located on the anterior parts of the lower extremities, on the forearms and on the thighs. They are distinguished by their round shape and noticeable swelling, their structure is dense, and their sizes can range from 1–10 cm in diameter. These inflamed areas can be painful, especially in the case of mechanical impact (pressure, etc.). Other symptoms include joint pain and a feeling of fatigue.
Erythema nodosum can be a symptom of a more serious disease, such as rheumatism or tuberculosis, or be independent. In the latter case, the origin of the disease often remains unclear, although the cause is often streptococcal infection, mononuculosis, or the use of contraceptives and sulfa drugs. The disease can last for two weeks or one and a half months. Over time, redness and swelling will subside, and bruising may remain on the affected areas, which will go away on its own.
Multiforme or polyform exudative erythema
This form of the disease is manifested by fever, headache, joint pain and discomfort in the muscles. After a few days, the skin of the body and limbs may become covered with a severe rash, which can cause itching and burning. Erythema multiforme may be accompanied by the formation of blisters filled with exudate. After their rupture, painful erosion may remain.
Even more severe forms of the disease can manifest as the Stevens-Johnson symptom, which is characterized by the appearance of blisters on the mucous membranes of the mouth, eyes, throat, and genitals. Lyell's syndrome may also occur, which is accompanied by a skin rash that turns into large blisters with serous-hemorrhagic content. In half of the patients, the exact cause of the disease cannot be identified. In other situations, manifestations of this type of disease such as erythema exudative multiforme are provoked by infectious viral microorganisms - measles, herpes, scarlet fever, etc. or taking certain medications.
Sudden erythema
As the name suggests, this type of erythema develops quite quickly. Symptoms include a sharp increase in body temperature with enlarged lymph nodes under the jaw, headache, aching joints and general weakness. Within four days the temperature returns to normal, and after that the skin of the face, limbs and torso becomes covered with a spotty rash. Sometimes the spots can merge and turn into erythematous fields.
Erythema migrans
May be a sign of Lyme disease, which is predominantly transmitted by a tick bite, although the cause is often unclear. The incubation period lasts 1–3 weeks. A ring-shaped spot appears at the site of the bite. It grows quickly and reaches 30 cm in diameter. Then this ring may turn pale and disappear altogether. The illness can last from 2 weeks to a couple of months. Erythema annulare cannot be treated and goes away on its own over time. This species poses a particular danger to a pregnant woman and her baby.
If we talk about the second, non-infectious form of erythema, then this includes diseases that appear as a reaction to a certain irritant, or as a manifestation of an allergy. These include the following types of pathologies:
X-ray erythema
It is manifested by inflammation of the skin and is characterized by a rash in response to prolonged or repeated exposure to X-ray waves. This type of erythema manifests itself on the irradiated area of the skin as a pronounced red spot that appears approximately 7 days after irradiation. This stain lasts 10 days, after which it darkens and acquires a brownish tint. Peeling may also appear at the site of the lesion.
Infrared or heat erythema
It appears due to prolonged or regular exposure to heat, which is not enough for a full-fledged burn. It appears as a mesh or pigmented rash appearing on the skin.
Persistent elevated erythema
It is a sign of allergic vasculitis. The disease has two forms: symptomatic, which manifests itself as a side effect, that is, as an allergy to taking certain medications, or against the background of polyarthritis, and idiomatic, which is associated with hereditary etiology and manifests itself as a nodular rash of a purple tone.