Dark spots on the eyeball are not uncommon. Spots on the eyeball can be either congenital or acquired. Most often, pigmentation of the cornea of the eye appears if some changes occur in the body.
Finding a dark spot on the eyeball causes anxiety in any person, because dysfunction of the eye can lead not only to discomfort, but also to partial or complete loss of vision. If you notice a dark spot on your eye, you should not draw premature conclusions, go to the pharmacy and self-medicate, because the wrong medication can lead to complications, since we are talking about the eyes, and this, as everyone knows, is one of the most vulnerable human organs .
If you find dark growths on the eye, it is better to contact an experienced specialist, even if the dark spot on the eyeball does not cause you discomfort.
- Lycee V.Rohto eye brightening drops make your eyes expressive and radiant, like white pearls;
- Relieves redness, brightens the sclera;
- Vitamins B6 and B12 nourish the membrane of the eye;
- Restore cell metabolism.
Congenital dark spots on the eyeball
Congenital spots are called pigmented nevi. This is nothing more than a birthmark, only it is located on the eyeball. The pigmentation of such a spot can vary from light brown to almost black. They may be flat and slightly raised above the surface of the eye. They are characterized by the following signs:
- looks like a pigment spot;
- has an irregular shape;
- cystic spaces are observed on the nevus;
- The intensity of nevus pigmentation may change over time.
They arise due to excess melanin in the body. Most often, this type of pigmentation is harmless. As a rule, it does not bother a person and does not affect vision.
Treatment
To prescribe treatment, the doctor needs to determine why colored or black dots appeared near the pupil, on the sclera.
- For injuries, surgery is used. After this, healing drugs are prescribed - “Korneregel”, “Solcoseryl”.
- Infectious diseases are treated with drops or ointments. Antibacterial - “Normax”, “Uniflox”. Antiviral - “Ophthalmoferon”.
- In case of pigmented formations, pterygium, pinguecula, the issue of their removal is decided. To prevent relapses, vitamin preparations are prescribed - “Taufon”, “Pro-vizio”.
Children are first placed under observation. In most babies, the spots disappear on their own.
Self-treatment and the use of folk remedies are not recommended. Without consulting a doctor, you can miss a serious illness and permanently lose your vision.
Spots on the eyeball are a sign of a malfunction of the body. It is recommended to consult a doctor to identify the cause of the pathology. After this, appropriate treatment is prescribed.
Share the article on social networks, leave comments describing your experience. Be healthy.
Treatment of congenital dark spots on the eyeball
Usually the size of the nevus does not change throughout life, but sometimes this formation can degenerate into malignant. Progressive nevus is distinguished by the following symptoms:
- blurred vision;
- a sharp change in color intensity;
- spread of nevus to the cornea of the eye;
- increase in the size of the nevus.
If you notice such signs, then this is not a reason to think about cancer. The doctor will determine whether the growth is benign or melanoma. If you notice the growth of the spot, blurred vision, discomfort and the sensation of a foreign object in the eye, then you need to undergo an examination by a specialist, undergo treatment, and, if necessary, remove the nevus. Modern medicine uses gentle methods of treatment and removal for this. If the nevus progresses, electroexcision is used, and plastic surgery of the damaged tissue is performed. Laser coagulation is widely used. Thanks to modern equipment, it is safe for nearby tissues and achieves good cosmetic results.
We must not forget that timely treatment of this disease guarantees a favorable outcome.
Causes of white spots on the eyes
These are people with congenital eye diseases, personnel who, due to the nature of their work, experience increased visual stress (office employees, engineers, welders, etc.), people working with harmful production factors, exposed to gases, chemical reagents, etc. .
| The term “sore” is popularly used to describe a spot that forms on the eye. Since ancient times, all sorts of fables have been attributed to the disease and shrouded in mystical overtones, but in fact this disease leads to a decrease in visual function, in severe cases to complete loss. |
The places where white dots appear can be different; all internal components of the eye are susceptible to them: the vitreous body, cornea, pupils, etc. But there are not so many reasons for their occurrence. Considering the location of the eyes, most diseases directly arise from disruptions in the functioning of the nervous and vascular systems of the body, the brain, and cardiac activity.
Congenital spots
The inclusions are caused by pigment that manifests itself on the tissues of the eye. Such points are harmless and do not pose a threat to the quality of vision. If the problem is of concern only in aesthetic terms, consult an ophthalmologist, he will recommend removal methods.
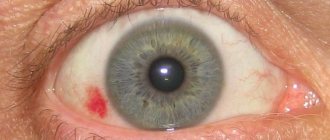
Red dots
The appearance is caused by sudden changes in blood pressure, leading to damage to the ocular blood vessels, and are nothing more than small hematomas. They do not require treatment and go away on their own.
The only thing recommended in this situation is to monitor your blood pressure level, regularly and preferably over time, and try to keep it within the limits inherent in the body.
The problem is also provoked by increased intraocular pressure, then it is necessary for a specialist to make a diagnosis and determine the necessary treatment.
Yellow and floating spots
Sometimes the patient may observe various objects in the form of blots or circles. They are barely noticeable, and sometimes quite bright, similar to flashes. In this case, it is very important to understand the nature of these manifestations: they occur irregularly, from time to time, or are present constantly.
Most often this is a single symptom. However, they can be combined with others:
- migraine;
- flashes of light;
- pain in the eyes.
Another formation that is worth mentioning is called a pinguecula, which is characterized by raised yellow spots on the mucous membrane of the eye. This disease is characteristic of older people, since it is formed largely due to the aging processes occurring in the conjunctiva. People who neglect to use sunglasses are also susceptible to this disease.
Floating spots on the integument of the eye are considered a more serious pathology. They usually occur when the pupil rotates. This defect is most likely associated with manifestations of retinal detachment. In most cases, patients feel uncomfortable and feel something like being hit by a speck. An ophthalmologist makes a diagnosis of a floating spot.
Return to contents
Floaters before eyes
The result of disturbances in the tissues of the vitreous body. When healthy, it is colorless and has a jelly-like consistency. Acts as an internal filler for the organ of vision and is designed to give it the necessary spherical shape and maintain the elasticity of the eye muscles. Most often, symptoms are associated with loss of transparency of the structure, due to the degeneration of the gel into connective tissue.
The reasons for this phenomenon are considered:
- excessive physical activity;
- salt deposits in the cervical region;
- instability of blood pressure;
- dystonia of vegetative-vascular nature;
- vitamin deficiency and atherosclerotic changes.
The appearance of floaters and white spots over the entire surface of the white membrane of the eye is influenced by bruises, retinal detachment, burns, hemorrhages and head injuries.
Belmo (leukoma)
A normal cornea is convex and completely transparent. Pathology provokes the degeneration of healthy tissue into connective tissue. The affected area does not work, and a scar forms in this place. A white spot on a person’s eye is a rich milky color, usually of an indefinite shape, located on its surface.
With changes of a pathological nature, it is prone to constant growth. The rate of decline in the ability to see is directly proportional to the distance between the spot and the pupil. The closer you get, the faster your ability to see deteriorates.
Clouding of the cornea occurs after injury or inflammation (trachoma, keratitis, etc.). As a result, transparency is lost, and the outer membrane in the iris area becomes white. Over time, the thorn becomes yellow due to the degeneration of fatty tissue or hyaline.
Types of leukoma
Depending on the factors that caused the change in the transparency of the cornea, the disease is classified into the following types:
- The congenital form is a fairly rare eye disease and, as a rule, provoked by a previous inflammatory process, less often manifests itself as a developmental defect inside the womb.
- Acquired leukoma.
Factors influencing its occurrence:
- consequences of previous keratitis (eye damage after infection with syphilis or tuberculosis). A massive scar and an extensive cataract appears;
- chemical eye burns. Alkaline solutions are considered especially dangerous, the effects of which can lead to complete blindness; the victim may retain the ability to distinguish between light and dark;
- traumatic eye injuries;
- unsuccessful surgery.
Black spots
Dark inclusions that are present in a person from birth are called nevi. In fact, this is an ordinary mole, but located in an unusual place. Colors can range from pale brown to black. The points are flat or have a slight convexity.
They are characterized by the following features:
- resemblance to a birthmark;
- irregular in shape;
- color may change over time;
- the appearance of cysts in the form of processes is not excluded.
The motivating factor is an excess of melanin. In most cases, nevi are not dangerous.
Changes in corneal structures
A slight decrease in the light transmission of the shell does not affect the patient's ability to see. Its healthy tissues degenerate into cloudy ones. The pathology process can be either local or widespread throughout the organ.
With pronounced opacity over the entire surface of the eye, after a short period of time a sharp decrease in vision is observed. Many prerequisites for inflammatory eye diseases can serve as an impetus for the development of leukemia, we will list just a few of them:
- infection with keratitis;
- tuberculosis infection;
- syphilis;
- other infections;
- conjunctivitis that has become chronic.
Return to contents
Transformations in the lens
The formation of white spots on the lens is often a sign of cataracts. The change in its transparency varies, depending on the stage of the disease, from pale milky to dark gray. The disease can be congenital or acquired, caused by processes of degeneration of the organ of vision.
The disease is more common in older people. Both classical and surgical treatment methods are used for it. In severe cases, the affected lens is amputated and an intraocular lens is implanted.
Retinal transformation
When there is insufficient blood supply to the retina, spots form on the tissues. In the language of doctors, this pathology is called angiopathy. The disease, as a rule, is caused by the presence of the following factors in the patient: hypertension, injuries to the organ of vision, regardless of the nature of their origin (chemical, mechanical, thermal), vascular atherosclerosis.
The disease in most cases is caused by diabetes mellitus, and is of a secondary nature, as a consequence of the underlying pathology. In addition to the appearance of white spots, patients experience uncomfortable sensations and note a decrease in the level of vision.
| Adherence to bad habits, especially smoking, only aggravates the picture, disrupting the blood supply to the retina. |
Acquired dark spot on the eyeball
If a pigment spot appears, it may indicate diseases such as destruction of the vitreous body and macular degeneration. As a rule, this disease is not dangerous. It can be caused by a number of reasons. Often these are age-related changes in the vitreous body, occurring in people aged 40 to 60 years.
Also, the appearance of such a spot can be caused by vascular disorders, such as dystrophic changes in blood vessels, arterial hypertension. Often the cause of the disease is metabolic and endocrine changes, for example, puberty.
Injuries to the head, eyes, and nose can lead to the appearance of dark spots.
In addition, there is a high probability of developing this disease in people who abuse alcohol, smoke, or eat large amounts of unhealthy food.
The process of retinal detachment that occurs with this disease is very dangerous.
If you do not contact a specialist in time, this can result in complete loss of vision.
Causes
The front part of our eye - the sclera - is white when healthy.
Its shade can vary from whitish-blue to whitish-pink, but it should be uniform. A noticeable change in the shade of the sclera and the appearance of yellow spots on it indicates the development of pathology. Moreover, this can be either a disorder of the eye itself or a systemic disease of the body. If yellow spots appear on the white of the eye, we advise you to contact an ophthalmology clinic.
Often, in addition to yellow spots on the eyes, the patient also notices other symptoms
:
- Itching and pain in the eye area
- Deterioration of vision
- Increased sensitivity to bright light
- The appearance of discharge from the eyes.
Yellow spots can signal various eye diseases. As a rule, these diseases are not very dangerous and cannot lead to complete loss of vision, but you should definitely not ignore their symptoms. Among the most common reasons are the following
:
- A conjunctival cyst is a formation with fluid inside, which may have a yellowish tint and appear as a small spot on the white of the eye.
- Pterygium is an eye disease in which the conjunctival tissue begins to grow from the nasal corner of the eye to the center of the cornea. The yellow spot on the squirrel has a triangular shape and sometimes changes color to scarlet or pink
- A pinguecula is a yellow spot that is a sign of aging of the conjunctiva or a lack of vitamin A. Most often, a pinguecula is localized on the inside of the eye near the bridge of the nose, so Patients do not immediately notice it
- Nevus is a kind of “mole” on the white, which signals serious pathologies of the eye
- Horner-Trantas spots are spots that occur as a result of an allergic reaction. They look like grains and are localized mainly around the cornea. The reason for the appearance of this type of spots is keratitis (inflammation of the cornea) or allergic conjunctivitis (allergic reaction of the conjunctiva).
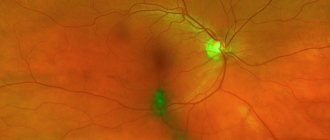
The process and features of the development of macular degeneration
With this disease, the blood circulation process is disrupted, and processes of destructuration begin. In the first stages of the disease, a person sees a black spot in the eye, which increases over time. There is deterioration in vision.
Instead of damaged nerves, new ones are formed, but they are no longer complete, so in a sick person you can see dark spots on the protein.
There are dry and wet types of the disease. The dry type of the disease is the most common. With dry macular degeneration, there is a slight decrease in vision, a lack of daylight, and the person feels periodic discomfort.
The wet type of the disease is much less common, and its consequences can be much more serious. With wet macular degeneration, irreversible processes occur in the retina of the eye. It is accompanied by a sharp loss of vision, pain, and the edges of objects seem wavy to the patient.
What to do if a dark spot appears on the eyeball?
As mentioned above, you should not self-medicate under any circumstances, especially if the appearance of a dark spot in your eye causes discomfort. You need to see an ophthalmologist.
To determine the diagnosis, doctors often use the so-called Amsler test. The patient is given a white checkered sheet of paper on which there is a point for concentration.
If, when you fix your gaze on this point, the edges of the cells become wavy, then there is cause for concern. In this case, the doctor will perform an angiography. During the study, the doctor introduces a composition with a dye into the vessel, with the help of which he determines how new defective capillaries are formed.
How is a dark spot on the eyeball treated?
To treat a dark spot, the ophthalmologist prescribes vasodilators and lyotropic drugs, biostimulants.
Older patients suffering from this disease have a similar set of complaints, so the doctor can easily identify the disease.
The diagnosis is confirmed using ophthalmoscopy and fundus photographs. When checking visual acuity, a disturbance in central vision is observed, and perimetry determines the preservation of the functions of the macula.
Today, treatment of the wet form of the disease with drugs such as Avastin and Lucentis is very effective. The introduction of these drugs intraocularly, it allows you to remove swelling from the retina and prevent the appearance of newly formed vessels. This improves the condition and preserves the patient's vision.
While taking these drugs, the metabolic process improves, and the retina of the eye is supplied with the substances it needs.
There are practically no effective methods for treating the dry form of the disease, so high-quality and timely prevention of the disease and strengthening the retina of the eye play a decisive role, especially for older people.
In order to improve the elasticity of blood vessels, drugs such as:
- No-shpa;
- Rutin;
- Papaverine;
- Angelin and others.
It must be remembered that all medications for treatment are prescribed exclusively by a doctor.
If the disease is in its early stages, the ophthalmologist may recommend vitamin and retinal strengthening medications.
The laser method is often used to treat this disease. It allows you to get rid of the disease and freeze the processes occurring in the eyeball.
It must be remembered that identifying the disease at an early stage and timely contacting a specialist will help to avoid complications and cure a dark spot on the eyeball.
General symptomatology of fundus changes (Part 2)
Description
3. Changes in the contents of blood vessels.
Abnormal pallor of the blood column with sufficient filling of the retinal vessels is observed in general anemia, chlorosis and leukemia. The unusually dark color of the blood column may depend both on the venous state of the blood, observed during fever, intoxication, heart defects, etc., and on the difficult outflow of blood from the neutral vein, due to: partial thrombosis, various types of compression, stagnation of blood in the jugular veins, etc.
Low blood pressure and circulatory arrest in the retinal vessels (embolism, thrombosis, spasm of the neutral artery) can also cause abnormally dark color of the blood in the vessels, while intermittent flow and segmentation of the blood column occurs in the veins.
4. Changes in circulatory phenomena
a) Arterial pulse.
Normally, the pulse wave is not noticeable on the retinal arteries. The arterial pulse is observed only under pathological conditions and is most clearly visible on the papilla, in those places where the vessel bends and emerges from the depths to the surface.
Arterial pulsation is caused by intermittent (synchronous with cardiac systole) blood flow into the retinal vessels, which may be due to the following reasons:
1) the blood flow entering the eye encounters an obstacle on its way and overcomes it only at the moment of systole (glaucoma, constriction art. ophthalmica, with tumors of the orbit and inflammation of the optic nerve); 2) blood circulation is so impaired and weakened that even a normal obstacle, in the form of intraocular pressure, is overcome only by a systolic wave (fainting, acute blood loss).
In some cases, pulsation of the retinal artery appears as a result of an unusually high pulse wave entering the eye, as, for example, with cardiac hypertrophy or aortic valve insufficiency. Graves' disease.
The locomotor pulsation of the S-shaped convoluted sections of the arteries, which is sometimes observed as a normal phenomenon, cannot be confused with the arterial pulse: however, expansion of the diameter of the vessels is not observed, but only periodic changes in the degrees of their bending are noticeable, occurring as a result of uneven longitudinal stretching of the walls of the vessels at the moment of systole. If locomotor pulsation is accompanied by an increase in the diameter of the artery, synchronous with the pulse, then this phenomenon is certainly pathological, since it contains an element of true pulsation.
Cessation of blood circulation (stasis) in the vessels of the retina, which occurs as a result of cessation of blood circulation in the central vascular system (cardiac arrest) or resulting from embolism of the central retinal artery, or rupture of the optic nerve, is characterized by the collapse of large trunks of blood vessels, while small branches on the periphery remain unchanged , while in the vessels there is a disintegration of the blood column into individual particles, like mercury in a broken thermometer. The central light strip disappears first on the empty trunks of the vessels, and then, due to the onset of clouding of the retina, also on the smaller branches containing blood.
b) Venous pulse.
The pulsation of the vein in the area of the optic nerve papilla, visible best at the place where it plunges into the tissue of the papilla or at the edge of the physiological ascavation, where the vein makes a bend, is common and is considered normal, while a spontaneous venous pulse extending far from the papilla - refers to pathological phenomena.
A normal venous pulse occurs due to the fact that in some eyes, during cardiac diastole, slight pressure in the veins is overcome by intraocular pressure and the vessel is temporarily compressed in places of sharp bends. Some authors believe that the cause of the venous pulse is pulsatory fluctuations in intraocular pressure.
A pathological venous pulse often occurs simultaneously with the arterial pulse in the above diseases, but can also be observed independently of the arterial pulse, for example, with pulsation of the jugular veins, due to venous stagnation in them, etc.
5. Inflammatory changes in blood vessels.
Perivasculitis, endarteritis or endophlebitis, as well as inflammation of all vessel membranes, are recognized ophthalmoscopically by the onset of clouding of the vessel wall; at the same time, the central light strip looks dim, and the white edges, on the contrary, seem clearer. Subsequently, a narrowing of the vessel appears over a greater or lesser extent, and the white edges become especially noticeable. Sometimes, with obliterating endarteritis or endophlebitis, the thickening of the wall can reach such a degree that obliteration of the vessel occurs and then the blood column naturally disappears in it.
In such cases, the two accompanying white stripes seem to merge into one and, as a result, the vessel looks like a bloodless white stripe (“white vessels”). Often, not the entire vessel is obliterated, but only some part of it or a branch, while the white stripes are a continuation of the red threads (vessels filled with blood) or, conversely, the red threads extend in the form of branches from the white trunk.
When examining directly in the center of such white stripes, it is often possible to notice the thinnest interrupted blood columns, which indicates the presence of still a lumen in the white vessel. The fact that blood circulation in the white vessel has not yet completely stopped is also indicated by the fact that the peripheral part of such a vessel passes into a vessel containing a clearly visible blood column.
If the white area is located in the peripheral part of the vessel trunk, then in this case it is necessary to pay attention to the contours of the vessel: the coincidence of the contours of the white area with the contours of the red part of the vessel indicates complete obliteration of the white area of the vessel, but if the contours of the white area are wider than the contours of the adjacent If there is a red area in it, then such a white vessel may still have a lumen, since the thickening of the stack of such a vessel could be due to perivasculitis (Table 28, Fig. b).
6. Symptom of vascular decussation (known in the literature as Hun’s or Salus sign).
At a young age, at the site of intersection of the artery with the underlying vein, no peculiarities from the intersecting vessels are noted. In some elderly people, due to thickening of the artery wall and, most often, with hypertension, the vein lying under the artery is compressed and ophthalmoscopically it seems as if it was interrupted, especially if the artery reflects more than usual.
Salus distinguishes three types of such changes:
a) Salus I. The vein at the intersection is not clearly contoured, there is a light reflex and has a thinning that occupies an extent equal to several diameters of the vessel (Table 17, Fig. 1);
b) Salus II. The vein in the area of the cross is not only thinned, but also bends in the form of an arc, in the middle of which lies the artery (Table 17, Fig. 2); c) Salus III. The vein curved into an arc at the intersection with the artery is visible so unclearly that it seems as if it was interrupted (Table 17, Fig. 3).
Sometimes partial venous thrombosis occurs at the site of crossing of vessels, accompanied by hemorrhages in the retina near the crossing vessels.
The symptom of vascular decussation is most often observed above the papilla on the temporal and nasal eyelids.
A symptom of vascular crossing is noted, mainly in espinal hypertension, as well as in other conditions associated with hypertension, for example, in acute glomerulonerritis, toxemia of pregnant women, and in some cranial injuries.
7. Thinning and atrophy of blood vessels
. The cause of thinning of the nipples may be hyaline degeneration of their wall. In some cases, the vessel wall ophthalmoscopically appears unchanged, in others, thinning and atrophy of the vessel is accompanied by thickening of its wall and a decrease in the irony of the vessel. But one way or another, atrophy of the vessels often leads to the fact that they are visible only in the posterior part of the fundus, and sometimes the retina generally looks like an avascular membrane.
Retinal vascular atrophy is the result of inflammatory degenerative processes in the retina during diseases of both the retina itself and the optic nerve.
8. Symptom of “copper and silver wire”.
Normally, a central light stripe is observed on the arteries, which is a light reflex that arises as a result of the collision of light with the cylindrical surface of the blood column moving in the vessels, has a light pink color, its width is approximately 1/4 of the diameter of the vessel (Table 28, Fig. 1) .
With severe sclerotic damage to the retinal arteries, accompanied by infiltration of their walls with a hyaline substance, which has a higher refractive index, the central light strip becomes brighter, wider and acquires a yellowish tint, which gives the vessel the appearance of a light copper wire (copper wire symptom) (Table 28, Fig. 5).
Subsequently, as a result of the onset of clouding of the vessel wall, the red color of the blood column is less prominent, and the light strip, on the contrary, becomes especially sharp and narrower, as a result of which the vessel takes on the appearance of a white silver string (a symptom of a silver wire) (Table 28, Fig. 4).
The symptom of copper and silver wires is most often observed with changes in the vessels of the retina due to arteriosclerosis and hypertension.
9. Diffuse (spread) retinal opacification
It can be expressed in varying degrees, from a subtle haze to a strong clouding, giving the retina a dull, gray appearance. Retinal clouding is often most noticeable near the optic papilla, since the retina is thicker here than in other parts of the eye. In order to make sure that the clouding really belongs to the retina, you need to keep the following in mind.
When retinal opacities are localized in those sections that directly border the papilla, first of all, blurred boundaries of the papilla are observed; in addition, the choroidal ring and scleral strip become invisible (if they were observed before the disease), since they are known to be located behind the retina. If this is also accompanied by hyperemia and clouding of the papilla, which often occurs, then the papilla completely loses its characteristic outline, but in any case its location is not difficult to determine along the course of the vessels.
When directly examined, one can notice that most opacities of the retina, due to the fact that they belong to its inner layers, are accompanied by radial striations, which coincide with. direction of the nerve fibers and is best seen around the papilla.
A reliable sign of retinal clouding is also the state of the central light strip on the vessels and other fundus reflexes. Reflexes in those places where the clouding is localized either weaken or disappear completely. With severe opacities of the retina on the vessels, not only does the central light strip disappear, but the vessel itself becomes poorly visible, since it turns out to be covered by a layer of opacified retina, and smaller vessels in certain areas are even completely lost in the opacified retina.
Diffuse opacification of the retina occurs in the following diseases: diffuse retinitis, neuroretinitis, retinopathy, commotio retinae, central artery embolism, retinal detachment. Naturally, these diseases can be accompanied not only by opacification, but also by other signs of retinal damage: hemorrhages, lesions, vascular changes, etc.
10. Limited white lesions (plaques).
Pathological changes in the retina are manifested not only by diffuse opacification, but can also have a nested, focal nature.
The shape and size of the lesions can be varied and to some extent depend on what layers of the retina they are located in: when the lesions are located in the inner layers, their shape is linear, striped; lesions localized in the outer layers of the retina usually appear as roundish spots. If the location of the lesion coincides with the retinal vessel, then this greatly facilitates the solution of the question in which layers it is localized; a lesion located in the anterior layers of the retina is often located above the vessel and covers it, while a lesion localized in the posterior layers of the retina does not cover the vessel. The color of the lesions is usually light white or light yellowish.
In the macula area, lesions are often arranged in such a way that a star-like figure is formed. This is explained by the fact that the nerve fibers around the macula run radially in relation to its center, and therefore the strips of exudate, located between the fibers, must take on radial etching.
The appearance of limited white lesions is associated with various changes, most often they are caused by the accumulation of fibrinous exudate or edematous fluid in certain layers of the retina.
White lesions are also caused by degenerative processes:
1) fatty degeneration of supporting tissue by the introduction of so-called fatty granular cells into the retina. 2) varicose hypertrophy of nerve fibers, which initially, due to edema, thicken, and then also undergo fatty degeneration.
Ophthalmoscopically, of course, it is impossible to establish these pathohistological details.
Clinical experience shows that focal changes in the retina cause a wide variety of diseases. First, a place among them should be given to chronic nephritis, accompanied by hypertension, followed by: blood diseases (especially leukemia), hypertension, arteriosclerosis, diabetes, sepsis, central vein thrombosis, poisoning with phosphorus, quinine, etc.
Peeudoalbuminuric retinitis with a typical star shape around the macula is observed after influenza, with chlorosis, tuberculous periphlebitis, cancer cachexia and even with brain tumors.
Consequently, it is not possible to make a final conclusion about the reason that caused focal changes in the retina only on the basis of ophthalmoscopic data, despite the fact that in some retinitis and retinopathy the ophthalmoscopic picture is very characteristic, but the identified foci, as well as many other pathological changes in the retina should always be considered as an alarming signal, which should prompt a deep, comprehensive study of the patient.
As for differential diagnosis, two questions may arise:
1) whether the detected lesions really belong to the retina and not the choroid and 2) whether these white spots are a consequence of damage to the retina, or a developmental anomaly - soft nerve fibers.
It is not always easy to distinguish fresh lesions of the retina from lesions of the choroid, simply because both the retina and the choroid are often simultaneously involved in the process, but if the lesion is localized primarily in the retina, then it is distinguished by its lighter color and more clearly defined outlines.
Old retinal lesions are easier to distinguish from choroidal lesions:
1) the foci of the choroid have a bright white color, since in the area of these foci the sclera is visible, due to atrophy of the chorion of the distant tissue and pigment epithelium: the foci of the retina are usually not distinguished by bright whiteness; 2) foci of the choroid are almost always surrounded by a more or less intense strip of pigment, while around the foci of the retina (if the pigment epithelium was not involved in the process) no accumulation of pigment is observed.
If unchanged retinal vessels still pass through the lesion, then after this there should be no doubt that the lesion belongs to the choroid.
It is relatively not difficult to distinguish retinal lesions from white bundles of pulpy fibers; Let us present some data characterizing the latter. The bundles of pulpy fibers are either directly adjacent to the optic nerve papilla, most often from below or above, or are located at some distance from the papilla. They have the appearance of shiny spots or stripes, on which radial striations are visible, especially at their outer edge, as a result of which they look r. in the form of a tongue of flame.
The retinal vessels are partly visible between the fibers, partly covered by them. This ophthalmoscopic picture remains unchanged during repeated examinations. If we add to this that, in addition to the indicated phenomena, no other pathological changes are detected in the fundus, and a general examination of the patient also excludes the disease, then the nature of this phenomenon becomes completely clear.
eleven). Pigment spots and denigmented (atrophic) lesions.
For painful outer layers of the retina, the main phenomenon is the pathological development of pigment in the retina. This pathological process is associated with a circulatory disorder in the choriocapillaris layer of the choroid, which, in turn, leads to disruption of the nutrition of the outer layer of the retina - the pigment epithelium, which in some cases undergoes complete atrophy, and in others undergoes growth phenomena.
These changes lead, on the one hand, to the disappearance of pigment in the pigment epithelium, i.e., to the appearance of depigmented foci, and, on the other hand, to pathological pigmentation of the retina. In this case, a kind of pigment migration is observed; it disappears in one place, but appears in other places, penetrates the retinas and is located in the form of separate lumps or jagged spots, connected by means of delicate processes with other spots, and thus a delicate pattern resembling a network is obtained.
In retinal pigmentary degeneration, the accumulation of pigment can take on star-shaped shapes that somewhat resemble bony bodies. Pigment masses penetrating into the thickness of the retina are often concentrated along the vessels and partially cover them, as a result of which individual vessels may appear in the form of thin, branching black threads. Some authors generally believe that the delicate branching figures of the pigment represent nothing more than the pigmented walls of small vessels and capillaries of the retina. As mentioned above, along with pathological pigmentation, there are often signs of disappearance of pigment in the pigment epithelium, expressed in the fact that in addition to pigmentation, depigmented foci are observed in the fundus. The presence of depigmented foci usually indicates damage not only to the outer layers of the retina, but also to the involvement of the choriocapillary LAYER of the VACUUM (chorioretinitis) in the process.
Through depigmented lesions of large sizes, the choroid is visible; In this case, the choroidal vessels often appear altered and appear in the form of white or whitish-yellow convoluted stripes. The retinal vessels in the area of the lesions pass over the altered choroidal vessels. Thus, an ophthalmoscopic examination will reveal retinal pigmentation, often accompanied by the presence of depigmented foci. — there is every reason to recognize a disease of the outer layers of the retina.
The diseases related here practically come down to two forms:
1) chorioretinitis in various manifestations and 2) retinal pigmentary degeneration.
12. Cholesterol crystals.
The deposition of cholesterol crystals in the retina is usually associated with the development of a degenerative process in it. Crystals can be deposited both in the vessels and in the tissue of the retina itself. Ophthalmoscopically, cholesterol crystals appear in the form of silvery or golden shiny dots. Freshly formed crystals are exceptionally bright and resemble highly reflective shards of glass. Sometimes a thin but very bright beam of light is reflected from such crystals into the vitreous body, and the crystals can shimmer with the colors of the rainbow.
Over time (after a few days), the intensity of the rays reflected by the crystals weakens, which is probably due to the deposition of other substances on their surface. Cholesterol crystals are usually located near some pathological focus (external exudative retinitis), but they can be scattered throughout the fundus of the eye. for example, with changes in the retina that occur after occlusion of the central artery.
13. Retinal hyperemia can be active or stagnant.
With active hyperemia, significant dilation of the veins is observed, while the caliber of the arteries remains without noticeable changes. The arteries, and especially the veins, are more tortuous than normal, both in the plane of the retina and in the plane that is not perpendicular to the observer’s visual line. In those places where the vessels rise above the general level of the retina, the central light stripe is absent or less pronounced, which is especially noticeable on the veins.
Around the papilla and on the papilla itself there is a large number of tiny vessels, which become noticeable due to their ongoing expansion. There is a slight blurring of the boundaries of the papilla. A delicate radial striation is noticeable on the retina around the papilla.
Active retinal hyperemia usually occurs in the same conditions that cause hyperemia of the optic papilla. With congestive retinal hyperemia, the arteries are significantly narrowed, and the veins, on the contrary, are dilated and highly tortuous. On the retina, radial striations are even more noticeable and a large number of small vessels are striking both on the papilla and around it.
Congestive retinal hyperemia occurs with congestive nipple, glaucoma, and orbital tumors. It also occurs with congenital heart defects (stenosis art. pulmorialis, non-closure of the foramen ovale and septum membrana ccum). The fundus of the eye in these cases has a blue-purple tint, and the large trunks of the vessels are strongly tortuous and dilated.
In connection with. Because retinal hyperemia is diagnosed mainly by the condition of the vessels, in order to avoid mistakes, one must remember that the retinal vessels are somewhat dilated and sharply tortuous when the angioma is located near the eyeball. In general, one must be careful with the diagnosis of retinal hyperemia, since the color of the fundus and the condition of the retinal vessels, due to individual characteristics, do not normally present the same ophthalmoscopic picture.
14. Retinal ischemia
is characterized primarily by narrowing of blood vessels, especially arteries, and, in addition, the pallor of the papilla attracts attention. Retinal ischemia most often depends on local causes, much less often it is a consequence of general anemia. Local causes that cause the most severe retinal ischemia include embolism, thrombosis and spasm of the central artery, as well as rupture of the optic nerve. Retinal ischemia can sometimes be observed in retrobulbar neuritis. For toxic amaurosis associated with. poisoning with quinine, ischemia is noted not only of the retina, but also of the optic nerve papilla.
Retinal ischemia, as a consequence of general anemia, is observed after large blood losses, after the forced release of asynthetic fluid, in the algid stage of cholera.
In these painful conditions of the body, retinal ischemia is distinguished by the characteristic appearance of the veins; at some distance from the papilla they are greatly expanded and convoluted, and as they approach the papilla and on the papilla itself they become much thinner. This phenomenon is explained by a sharp drop in blood pressure, as a result of which, under the influence of intraocular pressure, flattening of the veins occurs, which is the cause of obstructed outflow and a kind of stagnation of blood in the retinal veins.
Retinal ischemia should not be confused with the ophthalmoscopic picture of the fundus observed with retinal degeneration, since in these cases the retinal vessels are also narrowed, which is where all the attention of the researcher can be focused. But with a detailed study of the fundus of the eye, in these cases, it is almost always possible to detect other signs of retinal damage.
VASCULAR
1. Fresh inflammatory foci.
The choroid, as is known, is located behind the layer of pigment epithelium, therefore, the pathological changes occurring in it are visible to the researcher in case of translucent pigment epithelium (albicotic eyes) or in eyes with atrophic (degenerated) pigment epithelium. But, due to the fact that the inflammatory process occurring in the choroid usually very quickly involves not only the pigment epithelium, but also the retina, pathological changes in the choroid can always be quickly recognized in each case.
Ophthalmoscopically visible changes in choroiditis usually occur as a consequence of fibrinous or serous hornoiditis. In this case, inflammatory foci are observed at the bottom of the eye, the size of which usually does not exceed the diameter of the optic nerve papilla. The lesion becomes noticeable for the reason that it is usually accompanied by swelling of the choroid. spreading to neighboring areas of the retina, which above the focus, due to impregnation with edematous fluid, becomes cloudy and, thus, the retinal focus seems to be superimposed on the hornoid focus.
In such cases, of course, we should no longer talk about choroiditis, but about chorioretinitis. Such lesions, in contrast to retinal lesions, have a yellowish-gray tint and blurry contours. Since the pigment epithelium is also involved in the process, an accumulation of pigment clumps can soon be seen in the area of the lesions.
Further ophthalmoscopic picture of the lesions depends on the onset of atrophic processes in the choroid and pigment epithelium.
2. Atrophic foci and age spots.
In place of the inflammatory foci of the choroid, after some time, atrophic foci appear, which in most cases are the main ophthalmoscopic sign indicating damage to the choroid.
Atrophic foci of the choroid can have different sizes and shapes; they can be almost round, oblong, jagged, but often show a wide variety of other irregular shapes. The color and pattern of the lesions depends, on the one hand, on which layer of the choroid has undergone atrophy and, on the other hand, on the degree of pigment proliferation.
In those places where only one choriocapillaris layer has atrophied, the fundus of the eye loses its uniformly red color, which, as is known, is caused by this very layer of the choroid, and acquires a yellowish tint; here it is possible to recognize large choroidal vessels and intervascular spaces between them. If not only the choriocapillaris layer has atrophied, but also the adjacent pigment epithelium, then in the area of the lesions both the uniformly red color and the delicate granularity (shagreen pattern) caused by the presence of the pigment epithelium disappear.
With the degeneration of large choroidal vessels, if they are clearly visible after the onset of atrophy of the choriocapillary layer and pigment epithelium, sclerosing vessels appear in the area of yellowish foci in the form of yellowish-white convoluted stripes. The obliteration of these vessels is determined by the fact that they do not have a blood column.
Large vessels can atrophy to such an extent that instead of convoluted stripes, only their faint shadows are visible. With complete atrophy of the choroid, the lesions are white due to the translucency of the exposed sclera. Large white lesions are usually adjacent to areas that have a yellowish or dirty yellow color; these are the places of transition from partial to complete atrophy of the choroid. The retinal vessels pass over these lesions. The described picture may be further complicated by pigmentation and involvement of the retina.
It is difficult to imagine that a painful process in the choroid, especially localized in its internal layers, does not cause changes in the pigment epithelium, which has an intimate connection with the choriocaillary layer. Usually, with choroiditis, there is a circulatory disorder in the choriocapillaris layer, which leads to damage to the pigment epithelium and the appearance of pathological pigment. In this case, the pigment moves not into the thickness of the retina, as with chorporetinitis or retinitis, but into the choroid. The pigment is deposited either at the border of atrophic foci in the form of black borders, called epithelial-glial connecting belts, or inside the foci, or around them in the form of black spots. Sometimes individual large pigmented spots are observed in the fundus, the diameter of which may exceed the diameter of the optic nerve papilla.
The abundant growth of pigment in these places is associated with the connection of the stroma of the choroid with the pigment epithelium. Of course, for this it is necessary that in a given place degeneration of the choriocapillaris layer first occurs, but these certainly existing atrophic changes in the choroid are not visible, since they are masked by pigmentation.
If, simultaneously with the choroid, the outer layers of the retina are also involved in the process, then in the retina there is a proliferation of supporting glial cells, which, with the help of their processes, connect with. processes of the pigment epithelium; Thanks to this contact, the pigment moves from the pigment epithelium to the retina. Due to the fact that supporting glial cells grow predominantly along the vessels, pigment masses are also located, mainly along the vessels and can partially cover them.
Due to the fact that trophic foci and pigment spots can be observed both in lesions of the choroid and in diseases of the outer layers of the retina, it is necessary to point out the signs that should be used to guide the differential diagnosis of these changes.
If we do not take into account the phenomena of pathological pigmentation, then only on the basis of the ophthalmoscopic picture of atrophic foci it is not possible to decide what caused them - choroiditis, chorioretinitis or retinal degeneration. This is explained by the fact that atrophic foci, which are observed in choroiditis, and depigmented foci, often accompanying hornoretinitis and retinal degeneration, are essentially the result of the same pathological process - atrophy of the pigment epithelium and partial or complete atrophy of the choroid. With regard to pathological pigmentation, it is necessary to remember the following: with hornoretinitis and retinal deheperation, the pigment penetrates into the thickness of the retina and is located mainly along the retinal vessels and can even partially cover them.
With choroiditis, the accumulation of pigment occurs in the strictly choroid and pathological pigmentation of the retina never occurs.
Thus, atrophic foci should be considered as a consequence of choroiditis only if there are no signs of pathological retinal pigmentation. With chorioretinitis and retinal degeneration, on the contrary, atrophic foci are accompanied by pathological pigmentation of the retinal membrane.
3. Hemorrhages.
The choroid, rich in anastomoses, is prone to hemorrhages to a much lesser extent than the retina. Hemorrhages of the choroid have the appearance of red or brown-red spots, which are located under the vessels of the retina, but cover the vessels of the choroid. These hemorrhages are poorly visible, since they are covered by a layer of pigment epithelium.
In practice, choroidal hemorrhages occur at high degrees of myopia, when there is stretching and atrophy of the choroid in the posterior fundus.
In such cases, they are found most often in the area of atrophic foci, i.e., where there is no pigment epithelium. Usually, hemorrhages visible in the fundus almost always belong to the retina or are located between the retina and the pigment epithelium.
4. Changes in choroidal vessels
V albinos are quite clearly visible in cases where the disease is accompanied by atrophy of the pigment epithelium (degeneratio retinae pigmentosa) and even better in the area of large atrophic foci, since here the pigment epithelium and choriocalillary layer are atrophied, and therefore the large vessels of the hornoid are covered only by a transparent retina.
Naturally, observations of the choroidal vessels cannot be as subtle as those of the retinal vessels, and, as a result, only the following most noticeable changes are usually noted.
a) Sclerosis.
Vessels that are normally red become lighter, in some cases reaching an intense yellowish-white color. These changes in the color of blood vessels are often expressed unequally throughout the entire fundus of the eye.
Choroidal vascular sclerosis is one of the manifestations of old choroiditis, pigmentary degeneration of the retina (dcgencralio retinae pigmentosa) and, to a lesser extent, chronic glaucoma;
b) ABOUT B L I T E R A T I O N
. In large atrophic foci of the choroid, obliterated vessels in the form of white convoluted stripes are often observed. If the obliteration of the vessel has not yet completely occurred, then a thin column of blood is visible in the central part of the white stripes (Table 24, Fig. 5).
_________ Article from the book: Ophthalmoscopic diagnosis (with ophthalmoscopic atlas) | Radzikhovsky B.L..