Before we talk about the treatment of endocrine ophthalmopathy, let's once again recall the definition of this disease.
Endocrine ophthalmopathy is an autoimmune inflammatory disease of the periorbital tissues and soft tissues of the orbit, most often associated with thyroid pathology, with an unfavorable cosmetic outcome, significantly worsening the quality of life and, in some cases, posing a threat to vision. Let's look at a few key words of this definition. Endocrine ophthalmopathy is an inflammatory disease, which means it has several phases. Endocrine ophthalmopathy is divided into an active and inactive phase with manifestations characteristic of each phase.
Endocrine ophthalmopathy is most often associated with thyroid pathology, namely Graves' disease, autoimmune thyroiditis. Therefore, the treatment of endocrine ophthalmopathy cannot be considered separately from conservative and radical methods of treating the thyroid gland.
At the beginning of the section devoted to the treatment of endocrine ophthalmopathy, it is necessary to highlight modern approaches to the treatment of the thyroid gland.
Varieties
There are 4 types of exophthalmos:
- Permanent , in which neoplasms appear after an injury to the hand, eyes or brain herniation.
- Pulsating , after injury to the eyes and skull.
- Intermittent , manifests itself after tilting the head.
- Progressive malignant , occurs due to dysfunction of the thyroid system.
Also, it can be one- or two-sided , pronounced or inconspicuous .
Is it possible to get rid of pathology?
Protruding eyes are treated only after drawing up a complete picture of the deviation through a full examination, medical history, and exophthalmometry. It is also necessary to find out the factors causing the pathology. Therefore, the patient is obliged to visit all doctors to make an accurate diagnosis. Only after it is known what triggered exophthalmos, the doctor prescribes treatment.
If bulging eyes occur as a result of inflammation, doctors prescribe vitamin therapy, sedatives, antibiotics, and sulfonamides.
When oncology is diagnosed, they resort to chemotherapy and radiation therapy. The tumor is removed through surgery if necessary.
Endocrinologists treat exophthalmos if the reasons for its progression are problems in the functioning of the thyroid gland. After studying the results of hormone tests, doctors prescribe appropriate medications (radioactive iodine, merkazolin). At their discretion, specialists prescribe pulse therapy with prednisolone.
In case of injury, a pressure bandage and hemostatic medications are used.
If compression of the nerve is detected, surgery is necessary. Otherwise, the person faces blindness.
Edema exophthalmos
Exophthalmos itself is not a disease, it is only a symptom . Therefore, in order to successfully treat the disease, it is worthwhile to better understand the true reasons that led to the appearance of this deviation from the norm.
Attention! Edema exophthalmos is one of its most dangerous forms, in which the eyeballs literally dislocate from the sockets , which leads to disability of the patient.
Complex forms of protrusion are extremely rare . Most often, everything is limited to quite severe swelling and protrusion of the eyeballs.
Edema exophthalmos develops in patients whose age exceeds forty years. It can occur equally in both men and women. Patients often complain of increased intraocular pressure.
Edema exophthalmos can be either unilateral or bilateral .
Diagnostics
To diagnose this type of disease, the latest equipment available in modern eye clinics is used.
With the help of this kind of equipment, it becomes possible to determine intraocular pressure during exophthalmos, as well as the degree of vascular damage, which necessarily occurs during protrusion phenomena.
Of great importance is an external medical examination , which can and should be performed by a professional doctor.
Symptoms
If we talk about the symptoms of this disease, we can distinguish the following types :
- Severe pain that can only be relieved with severe analgesics or even drugs. This kind of pain is explained by the fact that as a result of exophthalmos, the nerve fibers are compressed. They are the ones who give the body a signal in the form of pain.
- Edema of the orbital eyelids. Also, the phenomenon of edema can spread to the periorbital area. This kind of edema is quite developed in order to instantly attract the attention of a doctor.
- Complete or partial loss of visual functions. This type of loss is due to the fact that as a result of protrusion, multiple optic nerves are compressed in order to make significant adjustments to the patient's visual pattern.
Edema exophthalmos
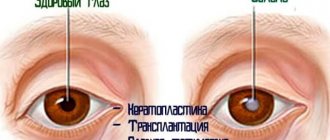
Graves' disease, endocrine, neurodystrophic, malignant, encephalitic exophthalmos, infiltrative endocrine ophthalmopathy, endocrine orbitopathy. Develops as a result of excess production of thyroid hormone from the anterior pituitary gland. It begins with transient swelling of the periorbital tissues, ptosis of the upper eyelid, diplopia when looking up or out. Exophthalmos, Graefe's symptom (lag of the upper eyelid when looking down) and Moebius' sign (convergence insufficiency), limited mobility of the eyeball, difficulty or impossibility of closing the palpebral fissure, and pain in the orbit appear.
The sensitivity of the cornea is impaired (due to compression of the ciliary nerve), conjunctival chemosis, photophobia, and lacrimation are observed. In severe cases, visual acuity decreases, keratitis, a corneal ulcer with hypopyon develop, hemorrhages occur in the retina, and a congestive optic disc develops, followed by its atrophy. Eye damage is often bilateral, usually uneven, but can also be unilateral.
The disease is observed mainly in middle-aged and elderly people, more often in men. Edematous exophthalmos occurs either spontaneously, or after surgery on the thyroid gland, or after conservative relief of thyrotoxicosis, as a result of significant edema and cellular infiltration of the external muscles of the eyeball and orbital tissue.
Treatment of edematous exophthalmos. It is carried out depending on the nature of the process and its stage (medication, radiation, surgery and combined). Drug therapy is always complex (corticosteroids, immunocorrective, dehydration, sedatives and drugs that activate metabolic processes). Corticosteroids (prednisolone) are given orally at 40-45 mg daily, gradually reducing the dose towards the end of the course to 2.5-5 mg per day, per course of treatment - 1.1-1.2 g.
Regardless of the functional state of the thyroid gland, triiodotyrosine hydrochloride is used (under the supervision of an endocrinologist) at 0.00005-0.000025 g per day, thyroidin at 0.05 g. Immunocorrective agents are prescribed: levamisole at 0.05 g, cyclophosphamide at 0.05 g 2 times a day. If the level of thyroid-stimulating hormone in the blood serum increases, the administration of bromocriptine (Parlodel) 0.0025 g 2 times a day is indicated. A 0.4% dexazone solution is administered retrobulbarically, 0.3-0.5 ml. X-ray therapy is recommended for the orbital area or the diencephalic area daily or every other day (single dose 0.75-2 Gy, total dose 6-40 Gy). Magnetic therapy has some effect.
Surgical treatment (decompression of the orbit through its lower wall) is resorted to in rare cases in order to protect the eye and preserve its functions in case of sharp protrusion of the eyeballs, damage to the cornea and optic nerve. Complex combined. Treatment causes subjective and objective improvement in most patients.
Diet for swelling of the thyroid gland
To restore normal metabolism (metabolism) during edema, you should adhere to proper nutrition (Nutrition for the thyroid gland). For your own health, you need to control some points yourself:
- Product quality;
- Amount of food consumed - eat well and not overload;
- Fractional nutrition - divide meals into five or six parts.
- Eat fruits, vegetables and greens (you should be aware that some foods in this category are prohibited). It is necessary to exclude fatty, fried, smoked foods, pickles, and sweets. Avoid fatty meats. Boiled chicken breast will not be harmful. You can also eat sea fish;
- Normalize drinking - at least a liter of clean water per day. If kidney function is impaired, you should consult a specialist.
Proper nutrition will help restore metabolism.
Thyrotoxic exophthalmos
Thyrotoxic exophthalmos is a consequence of a disease called thyrotoxicosis . It is important to note that this type of disease most often develops in women whose age exceeds fifty years. The phenomena of protrusion are often accompanied by redness of the lower eyelid, as well as inflammatory processes that occur in the eye orbit.
A huge number of visual and computer techniques are used for diagnosis. In particular, the patient is sent to undergo ultrasound, computed tomography, and magnetic resonance imaging . All these methods can provide true information about the condition of the patient's fundus, as well as the condition of the orbital and periorbital areas of the eyes.
Signs
Symptoms that can provoke this disease:
- Increased fatigue and irritability. These symptoms should be classified as general, which are the result of a serious illness.
- tremors .
- Swelling of the lower eyelid.
- Redness of the lower eyelid.
- Serious changes in the fundus of the eye, which lead to increased intraocular pressure.
- Increased sleepiness.
- Serious pain syndrome, which consists of unbearable dull or throbbing pain that may be characteristic of this disease.
How to treat thyrotoxicosis
Treatment of thyrotoxic exophthalmos can be carried out using a wide range of different methods. No method can completely eliminate this type of disease. The first and most common method is that the doctor prescribes conservative treatment , which can and should include a wide range of medications.
Medicines
An endocrinologist may recommend using a common and very inexpensive drug called L-thyroxine. This drug is used to treat endocrine diseases and is successfully used in patients who have certain thyroid diseases. As a result of the influence of this drug, the background of thyroid hormones , and the phenomena of exophthalmos may decrease.
In addition, an ophthalmologist can prescribe medications that can reduce swelling and inflammation. Here we are talking about local therapy. As such therapy, Dexamethasone is prescribed, which successfully fights inflammation.
It is also very important to prescribe eye drops that can reduce high intraocular pressure . Such drugs include Betoptik. These are unique drops that have no analogues. As a result of a unique pharmaceutical mechanism of action, they are able to influence the phenomenon of high blood pressure in order to reduce it or bring it back to normal.
Photo 2. Emoxipine, eye drops, 5 ml, solution 10 mg/ml, .
In cases of thyrotoxic exophthalmos, the retina of the eye is very often affected. Therefore, it is simply necessary to prescribe drops that can support the retina. These drops include "Emoxipin" , which is able to combat the manifestations of hemorrhages in the ocular environment, and can also strengthen the retina.
In addition, quite often the therapist resorts to prescribing prednisolone in tablet form , which can be purchased at any city pharmacy at a low price. Prednisolone is able to reduce inflammation and restore hormonal levels, which is of great importance in the thyrotoxic type of the disease.
Radioiodine therapy
Very often, with thyrotoxic exophthalmos, radioiodine therapy , which can equalize the hormonal levels in the thyroid gland. The meaning of this type of procedure is that the human thyroid gland is capable of attracting huge amounts of iodine.
Therefore, when a given chemical element is introduced into the body, this gland begins its active work in order to absorb the required amount of the element of the periodic table in a matter of hours.
This procedure is most directly related to the treatment of thyrotoxic exophthalmos, because after normalization of hormonal levels , we can observe a decrease in the intensity of symptoms of eye protrusion.
Operation
surgical methods are used to successfully treat exophthalmos . In modern surgical offices, the so-called thyroidectomy , which involves partial removal of the thyroid gland, has become widespread. After this type of operation, we can talk about a significant regression of exophthalmos, but not about its cure.
It is also worth noting that, despite the great popularity of this operation, it has a number of significant contraindications . Such contraindications include the fact that, often, after surgery, thyrotoxic exophthalmos turns into its edematous form, which is the worst prognosis for this disease.
Therefore, before carrying out this kind of surgical intervention, you should always think about the rather sad consequences . It is possible that in some cases it is worth limiting ourselves to only conservative methods of treating an insidious disease.
Thyrotoxicosis (hyperthyroidism) - symptoms and treatment
In the treatment of thyrotoxicosis, the following basic methods are usually used:
- conservative drug treatment with thyreostatic drugs;
- radioactive iodine therapy (I 131);
- surgery;
- non-drug treatment (limiting physical activity, healthy sleep, quitting smoking, preventing stress).[5][11][12]
The fight against the syndrome involves eliminating the clinical manifestations of thyrotoxicosis with normalization of T3, T4 and TSH values and achieving stable remission of the disease.
Conservative therapy
In the conservative treatment of diffuse toxic goiter in patients with a moderately enlarged thyroid gland (up to 40 ml), propylthiouracil (PTU) or thiamazole (Tirozol or Mercazolil) is prescribed. This helps to achieve normal functioning of the affected organ. In case of diagnosed cases of diffuse toxic goiter in the first trimester of pregnancy and the occurrence of side effects while taking thiamazole, PTU is prescribed. As a result of treatment, after 4-6 weeks there is an improvement - the level of free T4 is normalized. Additionally, beta-blockers are prescribed according to indications (for example, 2.5-5 mg of Concor per day).
In severe cases, it is recommended to take glucocorticoids - up to 10-15 mg of prednisolone per day. Then, over 2-3 weeks, the dose of the thyreostatic agent is reduced to a maintenance dose (no more than 10 mg per day). In parallel, the patient is usually prescribed 50 mcg of levothyroxine per day. This treatment regimen is called “Block and Replace.”[3][6][7][10][12] Stable maintenance of normal levels of free T4 and TSH will indicate the adequacy of the prescribed therapy.
If there are persistent side effects of the prescribed treatment, thyreostatic drugs are canceled, radioactive iodine therapy or surgery is prescribed. In case of relapse of thyrotoxicosis, the question arises about the need for radioiodine therapy or thyroidectomy - complete or partial removal of the thyroid gland.[5][12]
Treatment with radioactive iodine
Radioiodine therapy for diffuse toxic goiter is carried out in case of persistent relapse of thyrotoxicosis after the end of properly administered conservative therapy (for 12-18 months) and difficulties in taking thyreostatic drugs (decrease in the number of leukocytes in the blood or the occurrence of allergic reactions).
Treatment with radioactive iodine is carried out in specialized centers with radiation and environmental safety for people and nature. The only contraindications for this therapy are pregnancy and breastfeeding.
The goal of radioiodine therapy in destroying hyperfunctioning thyroid tissue is to achieve a stable hypothyroid state.[3][6][7][10][12]
Surgical treatment
Surgical intervention for diffuse toxic goiter is necessary if the goiter is located behind the sternum, with diffuse and nodular forms of goiter with compression and the patient refuses other methods of therapy. Total and subtotal thyroidectomy are the treatment of choice. If there is a nodular formation in the thyroid gland, it is necessary to perform a puncture biopsy and diagnostic cytological examination.[4][5][12]
After the operation, levothyroxine preparations (Euthyrox, L-thyroxine) are prescribed at the rate of 1.7 mcg per kg of the patient’s weight. TSH determination is carried out 6-8 weeks after surgical treatment and over time.
Treatment of diffuse toxic goiter with concomitant endocrine ophthalmopathy is preferably carried out using the “Block and Replace” scheme.[5][10][12]
In the case of thyrotoxicosis with a TSH-secreting pituitary tumor (thyrotropinoma), the TSH level is diagnosed taking into account the levels of free T3 and T4, as well as MRI (as a result, a pituitary adenoma is usually detected). Such patients require surgical intervention.[3][6][7][10][12]
Treatment
Treatment of thyrotoxicosis is carried out using methods: medications, radioactive iodine, surgery.
The severity of the disease determines the choice of drug. Treatment of eye symptoms:
- at the initial signs of the disease, do not use large doses of imidazole;
- in the future, long-term use of thyroid hormones is prescribed with constant monitoring of the pulse;
- during treatment, glucocorticosteroids and gamma therapy with simultaneous administration of high doses of hormones have a good effect;
- Daily administration of hydrocortisone helps.
Endocrine exophthalmos
Endocrine exophthalmos is associated with a kind of imbalance in the functioning of the endocrine glands . As a result of increased production of thyroid-stimulating hormone, you can often experience the phenomenon of protruding eyeballs.
Endocrine glands can increase or decrease the production of various hormones . In case of increased activity, this can lead to serious deviations in human life.
If we talk about the symptoms of this disease, they show great similarity with those symptoms that were described in the case of thyrotoxic exophthalmos . The diagnostic methods for this disease are also similar to those described above.
If we talk about treatment methods, then in cases of endocrine exophthalmos, a course of corticosteroid therapy . There is also radiotherapy , which involves administering high doses of radiation. In addition, surgical treatment methods are used. These include excision of the eye orbit , as well as its decompression .
Treatment of endocrine ophthalmopathy
Before reading this material, please read again the sections of the site devoted to the course and diagnosis of endocrine ophthalmopathy, where such concepts as “endocrine ophthalmopathy activity” as well as “severity of the disease” are discussed in detail.
When a patient comes to us for consultation, two main questions must be answered before prescribing treatment:
- Does the patient have an active stage of the disease or has the process already entered an inactive stage?
- What degree of severity of the process is developing or has already developed in the patient?
Endocrine ophthalmopathy is treated conservatively only in the active stage of the disease.
In most cases, a mild form of endocrine ophthalmopathy does not require conservative treatment, as it develops very quickly, sometimes within one day or night.
ATTENTION: DIAGNOSIS AND TREATMENT OF ENDOCRINE OPHTHALMOPATHY SHOULD BE PERFORMED BY SPECIALISTS. DEAR PATIENTS, DO NOT ENGAGE IN SELF-DIAGNOSIS AND SELF-MEDITION! YOUR MAIN TASK IS TO CONTACT A SPECIALIZED CENTER ON TIME
What treatment methods for endocrine ophthalmopathy exist today in the arsenal of doctors:
- Monitoring the patient, compensation for thyrotoxicosis/hypothyroidism
- The use of selenium in mild forms of endocrine ophthalmopathy
- Glucocorticoids
- Radiation therapy
- Surgery (orbital decompression, operations on the extraocular muscles, blepharoplasty)
- Biological therapy (use of monoclonal antibodies to treat severe forms of endocrine ophthalmopathy)
Let's take a closer look at each treatment method.
Monitoring the patient (Compensation for thyrotoxicosis/hypothyroidism)
To date, there are no accurate markers that can be used to predict the appearance and development of endocrine ophthalmopathy. Doctors have not yet learned to identify the disease at an early stage, which leads to the appearance and development of more severe forms of endocrine ophthalmopathy.
Fortunately, a significant number of patients develop a mild form of endocrine ophthalmopathy, for which we try not to prescribe so-called “severe” treatment. In mild forms of the disease, there is a slight deterioration in the quality of life, minimal swelling of the periorbital tissues, exophthalmos may appear, not exceeding the eye height by more than 2 mm from the original value.
Do not forget that endocrine ophthalmopathy should be distinguished from ocular manifestations of thyrotoxicosis, in which the following symptoms are observed:
- Expansion of palpebral fissures
- Sparkle in the eyes
- Slow blinking
In this condition, inflammatory changes in the orbit do not occur, and all symptoms are associated with the effect of thyrotoxicosis on the nervous system.
The main methods of treating mild forms of endocrine ophthalmopathy, as well as ocular manifestations of thyrotoxicosis, include compensation for thyrotoxicosis or hypothyroidism.
The risk-benefit ratio of the use of glucocorticoids and radiation therapy for mild forms of endocrine ophthalmopathy inclines doctors in most cases to refuse any treatment, since the expected effect is very low, and the risk of adverse events is high.
The use of selenium in mild forms of endocrine ophthalmopathy
In 2011, a group of European researchers completed a clinical study to evaluate the effectiveness of selenium in the treatment of mild forms of endocrine ophthalmopathy. In a clinical study, patients were given 100 mcg of selenium twice daily for 6 months and compared with another drug and placebo.
The results of the study demonstrated:
- Improving the quality of life of patients treated with selenium
- Reduction in the activity of endocrine ophthalmopathy in the group of patients treated with selenium
- No adverse effects have been reported with selenium supplementation.
Attention: The prescription of any medications should be carried out only by doctors and for existing indications. Consult a specialist.
Glucocorticoids
In their practice, ophthalmologists and endocrinologists use glucocorticoids more often than other drugs. Glucocorticoids have long been used for other autoimmune diseases such as rheumatoid arthritis, multiple sclerosis, retrobulbar neuritis, uveitis, psoriasis and many others. Let us recall that endocrine ophthalmopathy, as well as Graves' disease, are autoimmune diseases.
Glucocorticoids are steroid hormones produced by the adrenal cortex that are involved in many metabolic processes in the body. Synthetic glucocorticoids such as prednisolone, methylprednisolone, triamcinolone, dexamethasone as drugs have a pronounced anti-inflammatory and immunosuppressive effect.
In endocrine ophthalmopathy, the effect of using glucocorticoids occurs due to:
- Suppress the immune system and reduce inflammation
- Reducing the production of glycosaminoglycans (reducing tissue swelling)
- Reducing fibroblast proliferation (slowing scar tissue formation)
In clinical practice, there are several methods of using glucocorticoids:
- Para/retrobulbar injections (injections under the eyes)
- Tablet forms of glucocorticoids
- Pulse therapy with glucocorticoids
The history of the use of various methods of administering glucocorticoids for endocrine ophthalmopathy goes back more than 60 years. Many clinical studies have been conducted to evaluate the effectiveness of glucocorticoids in patients with endocrine ophthalmopathy, based on the results of which experts have identified the most effective and safe methods of administering glucocorticoids.
It is worth noting that there are differences in the effectiveness and safety of glucocorticoid administration methods.
In most developed countries, para/retrobulbar injections are avoided in clinical practice. During this manipulation, glucocorticoids are injected into the orbital cavity through the lower eyelid using a needle.
Despite the targeted delivery of drugs, this technique is not without significant drawbacks:
- With regular injection of drugs into the orbit, there is always a risk of hematoma formation, which creates an additional risk of compression of the optic nerve
- With multiple injections, additional trauma to the soft tissues of the orbit occurs, which is unacceptable in the case of endocrine ophthalmopathy, in which the soft tissues are already inflamed and increased in volume
- The amount of drug administered into the orbital cavity is insufficient for immunosuppression, that is, suppression of pathological mechanisms in the immune system.
Tablet forms of glucocorticoids are widely used in clinical practice, but the frequency of prescription of this particular form of drug delivery is gradually decreasing.
To achieve the effect of therapy for endocrine ophthalmopathy, the starting dose of the drug, according to many scientific works, should be at least 60 mg per day, i.e. 12 tablets (prednisolone). The maximum permissible single dose of prednisolone is 90 mg, i.e. 18 tablets. It should be taken into account that when prescribing treatment with tablet forms of glucocorticoids, the duration of treatment is 1.5-3 months. With this type of drug administration, the frequency of adverse events is higher than with intravenous administration (pulse therapy). While taking tablet forms of glucocorticoids, patients experience deterioration in laboratory parameters of liver function, increased blood sugar, metabolic disorders and weight gain; there is a risk of increased osteoporosis, as well as exacerbation of gastritis, gastric and duodenal ulcers.
As treatment protocols for endocrine ophthalmopathy improve, the frequency of prescription of tablet forms of glucocorticoids has been reduced. Currently, tablet forms of glucocorticoids are prescribed to prolong treatment after pulse therapy. The starting dose and duration of treatment will be determined by the doctor during your in-person visit to the clinic, having previously assessed the effectiveness of pulse therapy.
Pulse therapy with glucocorticoids
Intravenous glucocorticoids (pulse therapy) are the most common therapy for patients with active endocrine ophthalmopathy.
Over the past few decades, a large number of clinical studies have been conducted demonstrating the effectiveness and safety of this method of administering glucocorticoids.
The essence of the treatment is the simultaneous administration of large doses of the drug, which have an immunosuppressive, anti-inflammatory and decongestant effect.
Pulse therapy with glucocorticoids is carried out:
- with a combination of the active stage of the disease and moderate or severe form of endocrine ophthalmopathy
Various pulse therapy regimens have been tested in clinical studies, and today, in most cases, patients experiencing endocrine ophthalmopathy are treated on an outpatient basis, without hospitalization.
During a face-to-face consultation at the clinic, the doctor will select the most suitable pulse therapy regimen with glucocorticoids. The frequency of administration and dose of glucocorticoids during pulse therapy depend on the severity of endocrine ophthalmopathy, the age of the patient, and the presence or absence of concomitant chronic diseases of the body.
Contraindications to pulse therapy with glucocorticoids:
- Active stage of hepatitis B and C
- Diabetes mellitus in the stage of decompensation
- Gastric and duodenal ulcers in the acute stage
- Uncontrolled arterial hypertension - mental disorders in the acute stage
- Individual intolerance to glucocorticoids
PS . In case of existing contraindications to the use of glucocorticoids, the patient will be offered radiation therapy to the orbital area.
Over the past 5-10 years, pulse therapy regimens have undergone changes. In the section of the site dedicated to treatment, we will not describe all possible treatment regimens, but will describe the most commonly used pulse therapy regimen.
- Administration of 500 mg methylprednisolone intravenously, very slowly, once a week. 6 droppers are performed with an interval of 1 week
- Administration of 250 mg methylprednisolone intravenously, very slowly, once a week. 6 droppers are performed with an interval of 1 week
After the last dropper, the ophthalmologist will evaluate the effect of therapy and give his recommendations.
Once again, we draw your attention to the fact that pulse therapy regimens may differ depending on the clinical situation. It is very important to contact a specialized center in time, where they will select a treatment regimen taking into account all the patient’s characteristics.
Radiation therapy
Over the past two decades, radiation therapy has established itself as an effective treatment for endocrine ophthalmopathy. The essence of the method is to irradiate tissues using ionizing radiation, which is created by various sources. In clinical practice, there are different devices for delivering radiation therapy. Regardless of the device used, the effect of treatment occurs due to a decrease in the activity of lymphocytes that infiltrate the orbital tissue during endocrine ophthalmopathy, after which inflammation and swelling of the tissue (oculomotor muscles) decreases.
Treatment using radiation therapy to the orbital area should be carried out only in the active stage of the disease. Radiation therapy is not only effective, but also a safe treatment method.
Contraindications to the use of radiation therapy:
- Age under 35
- Presence of diabetic retinopathy (complications of diabetes mellitus on the retina of the eye)
It should be noted that, compared to pulse therapy with glucocorticoids, the effect of radiation therapy occurs somewhat later. During treatment, patients note an improvement in eye mobility.
According to some clinical studies, the use of radiation therapy simultaneously with glucocorticoid therapy leads to a more pronounced treatment effect. In their practice, Endorbit project doctors recommend combining radiation therapy and pulse therapy with glucocorticoids, especially for severe forms of endocrine ophthalmopathy.
The patient should know that when prescribing radiation therapy to the orbital area for endocrine ophthalmopathy, the duration of treatment will be 15-30 days, depending on the number of sessions. The standard radiation dose is 20 Gy, which the patient receives in 10-15 sessions.
Surgical treatment of endocrine ophthalmopathy
Endocrine ophthalmopathy is a disease that leads to significant cosmetic, anatomical and functional changes in the orbit.
Separately, we note that the overwhelming majority of patients are women of working age, who experience changes in appearance especially painfully. In this regard, the issue of cosmetic/aesthetic surgery for patients with endocrine ophthalmopathy can be considered one of the pressing issues that the Endorbit project solves.
In the vast majority of cases, surgical treatment of endocrine ophthalmopathy is carried out in the inactive stage of the disease, as well as with long-term stabilization of thyroid hormone levels.
When we talk with patients about surgical treatment of endocrine ophthalmopathy, we often talk about psycho-emotional rehabilitation, since it is surgical treatment that will allow patients to return to their former appearance.
Indications for surgical treatment of endocrine ophthalmopathy:
- Retraction of the upper eyelid (widening of the palpebral fissure)
- Increased hernial protrusions of periorbital tissues (bags above and below the eyes)
- Exophthalmos (protrusion of the eyeballs forward)
- Ghosting
- Decreased vision due to optic neuropathy/keratopathy
Urgent surgical treatment of endocrine ophthalmopathy is carried out only when a diagnosis is made: endocrine ophthalmopathy, active stage, severe, optic neuropathy/keratopathy.
If there is no effect from powerful treatment with the simultaneous use of pulse therapy with glucocorticoids with radiation therapy and progressive vision loss, the patient will be offered urgent surgery.
Depending on the severity of the endocrine ophthalmopathy, the surgical options we can offer the patient vary. In some cases, multiple surgeries may be required to achieve good aesthetic and functional results.
Eyelid surgeries
Mild forms of endocrine ophthalmopathy, as we have already described in the section “Course of endocrine ophthalmopathy,” account for 55-60% of all cases of the disease. With these forms of endocrine ophthalmopathy, patients are concerned about the widening of the palpebral fissures, a slight increase in the upper and lower eyelids, and slight exophthalmos.
For endocrine ophthalmopathy of moderate or severe severity, eyelid surgery is performed in the second or third stage after orbital decompression and surgery on the extraocular muscles.
The surgical team of the Endorbit performs any eyelid surgery for endocrine ophthalmopathy. This may be blepharoplasty of the upper and lower eyelids or lengthening of the muscle that lifts the upper eyelid (anterior blepharotomy, müllerectomy). These operations can be performed under local anesthesia, however, for the patient’s comfort, we offer short general anesthesia, during which the operation proceeds faster and, most importantly, with fewer complications for the patient.
During a face-to-face consultation at the clinic, we will tell you when it is best to perform eyelid surgery and discuss different options for surgical techniques and rehabilitation methods.
Operations on the extraocular muscles
With the development of moderate or severe endocrine ophthalmopathy, patients may encounter problems such as diplopia or double vision. This occurs due to the development of a pathological process in the extraocular muscles with the appearance of cicatricial changes in them. The normal functioning of enlarged extraocular muscles with scarred changes leads to a disorder of synchronous eye movements, as well as to limited eye mobility in different directions with the further development of a double image.
Minor double vision and strabismus can be corrected with the help of special prismatic lenses, but for most patients it is not possible to choose such lenses.
Surgeries on the extraocular muscles are performed under general anesthesia. As a rule, the operation is performed on one eye, although there are cases when it is necessary to correct complex strabismus by operating on both gases at the same time.
In a number of clinical cases, before operations on the extraocular muscles to eliminate strabismus and diplopia, it is necessary to perform orbital decompression, which we will discuss below. When exophthalmos is eliminated, the range of movements of the extraocular muscles may increase, and, therefore, the nature of diplopia may change.
During a face-to-face consultation at the clinic, the surgical team of the Endorbit will determine the degree of strabismus, the nature of damage to the extraocular muscles and suggest the appropriate time for surgical treatment.
Orbital decompression
Orbital decompression is a surgical method for the treatment of endocrine ophthalmopathy, in which the pressure in the orbit is reduced by removing the bone walls and fatty tissue, as well as creating additional space for the eye, extraocular muscles, and optic nerve. Let us recall that the orbit is a space limited on 4 sides by bone walls. With the development of the inflammatory process in endocrine ophthalmopathy, there is an increase in the volume of fatty tissue and the size of the extraocular muscles, which become cramped in the space enclosed by bone walls. Therefore, the only possible option is to keep the eyes forward, which leads to exophthalmos.
It is worth noting once again that in the vast majority of cases, orbital decompression is carried out during the inactive stage of the disease. The extent of surgical intervention depends on how much we want to reduce the size of exophthalmos. Removal of one orbital wall leads to a decrease in exophthalmos by 2-3 mm. There are cases when the level of exophthalmos differs from normal values by 10 - 12 mm. In such cases, it is necessary to remove 3 orbital walls to eliminate the changes. By conducting preoperative preparation, evaluating old photographs of patients, CT images of the orbit, the Endorbit project surgical team will determine the extent of removal of fatty tissue and bone walls of the orbit.
Symptoms
In each case, the symptoms may be different, and here everything depends on the degree of development of the disease. If the patient consults a doctor late, the disease is visible to the naked eye. What symptoms should cause alarm in a person and force him to see a doctor:
- Swelling of the eyelids.
- Drooping of the upper eyelid, which may disappear by evening.
- Enlargement of the palpebral fissure.
- Bug-eyed.
- The vessels of the sclera become tortuous and very noticeable.
- A feeling of dryness and sand in the eyes.
- Visual acuity deteriorates, and over time a cataract may form.
- The eye loses visual mobility.
This disease in rare cases leads to complete loss of vision. However, it can cause a significant deterioration in its severity. As a result of the disease, cataracts, keratitis and neuropathy often develop.
The easiest way to notice decent bulging eyes, which occurs in advanced stages of the disease. However, doctors advise not to let it get to this point, as this may complicate healing.
Find out what ailments Tsipromed eye drops will help you get rid of here.
You should be wary if a too noticeable vascular pattern of the sclera appears
Broad-spectrum antibiotic – Cipropharm eye drops.
Read the article about what ailments Ciprofloxacin eye drops will help you get rid of.
Eye symptoms in thyrotoxicosis
When suffering from thyrotoxicosis, the palpebral fissures widen, and the person seems to be scared or surprised.
Increased shine is observed, patients complain of “sand” in the eyes, photophobia, and pain.
Symptoms of the disease include:
Delrymple - wide widening of the slits of the eyes (surprised look).
Shtelvaga is an extremely rare blink.
Graefe - delay of the outer eyelid during eye movement. Occurs due to increased tone of the muscles that are responsible for the movement of the eyelid. White stripes of sclera are visible. When the pupil moves, the eyeball moves freely with it.
Moebius - the convergence of the eyeballs is impaired, the ability to fix objects close to them is inability. The result is greater tone of the oblique muscles than the internal rectus muscles.
Kocher - displacement of the eyelid towards the lower or upper edge of the orbit, thereby exposing the sclera. The displacement may be minor, unnoticeable, or expose the cornea.
We recommend reading: Recovery after thyroid removal
Jellinek - staining of the eyelids and significant darkening of the skin occurs.
Geoffroy - forehead wrinkling does not occur when looking up.
Rosenbach - tremor of the eyelids with closed eyes.
Brown - there is no narrowing of the eyes when laughing.
Ecrota - the upper eyelid swells.
Wilder - the eyeball moves with stops, in steps.
Protrusion of the eyeballs.
Impaired lacrimation - in patients with bulging eyes. Inflammation of the cornea occurs due to the inability to close your eyes either day or night.
All these signs of the disease, especially protrusion of the eyes and widened palpebral fissures, make the face of a sick person look as if he is frozen with fear.
Usually these symptoms are bilateral; unilateral exophthalmos is less common.
With moderate and severe eye damage, vision is significantly reduced and there is double vision.
But eye symptoms do not always appear; some patients with severe disease do not have them.
Therefore, the disease cannot be assessed based on eye symptoms.
Doctors distinguish three severity of exophthalmos disease:
- I - slight - (15.9±0.2) mm, slight swelling of the eyelids occurs;
- II - average - (17.9±0.2) mm, with severe swelling of the eyelids and obvious signs of deformation of the eye muscles;
- III - strong - (22.8+1.1) mm, ulceration of the cornea, movement of the eyeballs is severely limited.
Pulsating exophthalmos
With pulsating exophthalmos, a significant disturbance occurs in the vascular bed. This kind of disorder manifests itself in the fact that vascular tone in the cavernous sinus is upset. Very often, this kind of disease can be observed in children who have a disease called cerebral hernia . If we talk about diagnostics, the following types are used:
- Ultrasound.
- CT scan.
- Magnetic resonance imaging.
The same methods are used as for the types of exophthalmos mentioned above.
If we talk about the main symptoms of this disease, they are similar to the symptoms of thyrotoxic exophthalmos, however, with pulsating protrusion, the patient’s vision does not disappear.
It is disrupted so that the patient has enormous visual discomfort. Often with this disease, we can talk about nystagmus of the eyeballs.
Therapy
The disease is treated with radiotherapy . It is important to use large enough doses of radiation to achieve a significant effect. Small doses of radiation are not able to have a significant effect on this disease.
A radical method in the treatment of pulsating exophthalmos is the method in which the so-called ligation of the carotid artery . As a result of this type of fixation, the pressure on the eyeballs is reduced, which means the symptoms of bulging are reduced.
However, with this surgical method of exposure, serious side effects may occur in the form of increased intraocular pressure. Therefore, the surgeon is obliged to weigh all the pros and cons before performing this type of operation in order to avoid serious complications in the form of complete or partial loss of vision.
Damage to the musculoskeletal system in diseases of the thyroid gland
With pathology of the thyroid gland, increased (hyperthyroidism) or decreased (hypothyroidism) production of thyroid hormones is observed.
Hyperthyroidism occurs in diseases such as diffuse toxic goiter, toxic nodular goiter, thyroid adenoma, as well as when taking thyroid hormones, thyroid cancer. The combination of rheumatic diseases with thyroid pathology primarily refers to Hashimoto's thyroiditis and diffuse toxic goiter, in the genesis of which autoimmune mechanisms are important. In both diseases, antibodies to thyroglobulin and to the microsomal fraction of the thyroid gland, rheumatoid factor and antinuclear antibodies are detected. The most common combination of autoimmune thyroid diseases and rheumatoid arthritis is observed. The spectrum of musculoskeletal manifestations of hyperthyroidism includes myopathy, systemic osteoporosis, periarthritis, and acropathy.(7)
Thyrotoxic myopathy (TM)
It was identified as an independent nosological form in 1938. Currently, TM is rarely diagnosed, which is largely due to the existing opinion that weakness in thyrotoxicosis is always caused by general asthenia, and not by damage to skeletal muscles. There are also objective reasons that make the diagnosis of TM difficult: relatively mild damage to individual muscles; absence (with rare exceptions) of paralysis; masking myopathy with symptoms of thyrotoxicosis. Thus, patients with TM, as a rule, do not complain of muscle weakness, and existing motor difficulties are explained by other reasons (weight loss, nervous fatigue, age, “salt deposition,” etc.). Diagnosis is also complicated by the fact that muscles often have a “healthy” appearance due to the absence of their atrophy, therefore the neuromuscular system is not examined and myopathy is not recognized. Although during a special clinical study it is detected in 61-81.5%, and with electromyography, according to various authors, in 92.6-100% of patients with thyrotoxicosis. Tests that make it possible to objectify muscle weakness in clinical practice are standing up from a squatting position and from a low chair, from a supine position, etc. (4).
In most patients, symptoms of myopathy develop within the first 6-7 months from the onset of symptoms of thyrotoxicosis. The severity of myopathy does not depend on the severity and duration of thyrotoxicosis, the degree of enlargement of the thyroid gland and the severity of eye symptoms (4).
The most commonly involved muscles in TM are the iliopsoas, gluteus maximus, palmar interosseous and lumbrical muscles, neck flexors and biceps brachii muscles. Detection of weakness of these muscles can serve as one of the important diagnostic criteria for TM.
Opinions about the relationship between the frequency (and degree) of muscle weakness and atrophy in patients with TM are contradictory in the literature. Some researchers believe that muscle weakness is invariably accompanied by muscle atrophy (5). Others say that muscle atrophy is many times more common than muscle weakness (5,14). This issue was studied in detail by Kozakov V.M. et al. taking into account anatomical regions and muscle groups (5). In the muscles of the shoulder girdle (trapezius, serratus anterior), shoulder girdle (supra- and infraspinatus), shoulders (triceps), hips (quadriceps and adductors), atrophy is more often detected than weakness. In other muscle groups (facial muscles, neck flexors, interosseous and lumbrical muscles, rectus and oblique abdominis, gluteus maximus, iliopsoas), on the contrary, weakness is detected more often than atrophy.
Another feature of TM is excessive folding of the skin over the affected muscles. This is most commonly observed in the triceps brachii and quadriceps femoris regions. It is these muscles, which seem the most atrophied, that invariably retain full strength. Apparently, the disappearance of subcutaneous fat creates the false impression of severe muscle atrophy.
In the clinical picture of the disease under study, other peculiar features were noted: frequent mild to moderate damage to the facial muscles (frontal and orbicularis oculi), preservation or increase of deep reflexes, absence of muscle pseudohypertrophy and terminal atrophy, tendon and muscle retractions, pathological deformations of individual body segments ( 5).
For diagnosis of neuromuscular disease, in addition to knowing the frequency of weakness and atrophy of individual muscles, the topography (formula) of muscle lesions is important. Kozakov V.M. et al. The location of muscle weakness in relation to the severity of myopathy has been studied (5). In patients with mild myopathy, weakness of the iliopsoas muscles (93.4%), gluteus maximus (70.3%), interosseous and lumbrical muscles of the hands (69%) and/or neck flexors (54%) was initially detected. As the myopathy progressed, the muscles of the shoulders (biceps, deltoid), hips (adductors and posterior group) and shoulder girdle (trapezius, serratus anterior, supraspinatus and infraspinatus muscles) were successively involved.
It is widely believed that with TM (as with other myopathies), the muscles of the shoulder and pelvic girdle and proximal limbs are mainly affected; cases of involvement of the distal parts and intrinsic muscles of the hands have been rarely described. Kozakov V. M. et al. The frequency of detection of weakness of the thenar and hypothenar muscles was specifically studied in comparison with the frequency of detection of weakness of the palmar interosseous and lumbrical muscles of the hands (5). The muscles of the first group were rarely involved (in 1.9% of patients). Weakness of the muscles of the second group was quite common (in 74.1% of patients).
Thus, at the earliest phase, TM can be recognized by the following criteria:
1) “Formula” for the spread of muscle weakness involving the iliopsoas, gluteus maximus, interosseous palmaris and lumbrical muscles of the hands and/or neck flexors;
2) Atrophy of the triceps muscles of the shoulders and quadriceps muscles of the thighs without reducing their strength;
3) Excessive folding of the skin over these muscles. The diagnosis is confirmed by thyroid function tests.
It should be noted that TM, according to clinical data and morphological changes in muscles, as well as electromyography, is a phenocopy of a number of hereditary and non-hereditary neuromuscular diseases, which requires an appropriate differential diagnosis. It is extremely important to distinguish this exogenous myopathy from similar diseases, since adequate and timely treatment in most cases leads to almost complete regression of TM. In the absence of specific treatment for TM, muscle weakness increases progressively, and the patient stops moving independently. In rare cases, acute thyrotoxic myopathy develops (3,7). The disease manifests itself as generalized flaccid paralysis and paresis, accompanied by impaired swallowing and breathing. Pathological muscle fatigue is observed. These symptoms can last from a few minutes to several hours or even days. In their pathogenesis, a certain role is played by a decrease in the concentration of potassium in the blood, which requires immediate determination of its concentration in the blood. Taking potassium supplements sometimes interrupts these symptoms and prevents the onset of new ones (7). Cases of death from TM have been described.
The group of diseases with which TM must be differentiated is determined by the degree of its severity (4). Severe forms with pronounced muscle atrophy must be distinguished from muscular dystrophies, carcinomatous myopathy, proximal spinal muscular atrophy and diabetic proximal amyotrophy; with the addition of bulbar disorders - from polymyositis, myotonic dystrophy and myasthenia. Mild forms, in which muscle weakness predominates, should be differentiated from polymyositis, Addison's disease, and steroid myopathy.
There is a phenotypic similarity between TM and the hip variant of myodystrophy (4). However, in patients with myodystrophy, complaints of muscle weakness and movement disorders caused by it are leading, while in patients. In addition, the hereditary form of muscular dystrophy develops slowly (over a number of years). In both diseases, the iliopsoas and gluteus maximus muscles are involved early in the process. However, in patients with TM, as a rule, weakness of the palmar interosseous and lumbrical muscles and/or neck flexors is simultaneously detected; in patients with myodystrophy, the function of these muscles is preserved even in the late stage of the disease. Differences are also observed in the further generalization of muscle lesions. In the hereditary form of myodystrophy, weakness of the quadriceps and gluteus medius muscles, as well as the muscles of the interscapular region, occurs early. Patients often fall (weakness of the quadriceps muscles), when walking they roll from side to side (“duck walk” - weakness of the gluteus medius muscles), it is difficult to raise their arms above the head (weakness of the trapezius and serratus anterior muscles). Due to a significant imbalance in muscle balance, various persistent skeletal deformities are formed (increased lumbar lordosis, displacement of the shoulder girdle downwards and inwards, “sunken chest”, “wing-shaped shoulder blades”). The described disorders do not occur in patients with TM. In patients with myodystrophy, muscle weakness usually follows atrophy (the exception is pseudohypertrophied muscles). With TM, “weak” muscles often retain normal volume, while atrophied ones largely retain muscle strength. It should be added that deep reflexes in patients with myodystrophy early decrease and disappear, while in patients with TM they remain normal or increase. In addition, in patients with myodystrophy, the phenomenon of excessive folding of the skin over the affected muscle does not occur even with the complete disappearance of the muscle belly.
In a number of patients with TM, damage to the bulbar muscles is detected simultaneously with weakness of the proximal and distal muscles. In such cases, it is necessary to differentiate TM not only from myodystrophy (oculopharyngeal form), but from proximal spinal muscular atrophy (PSMA), which begins with damage to the muscles of the pelvic girdle and hips, and subsequently the process spreads to the shoulder girdle and shoulders; in a later phase, the muscles of the distal arms and legs, and the 5,7,9-12th nuclei of the cranial nerves are affected (4). Mild dysphagia and dysarthria occur, and fasciculations are observed in the muscles of the face, tongue, limbs and trunk. Unlike TM, with PSMA, along with weakness, atrophy of the facial and masticatory muscles and tongue is detected. Atrophy and weakness of the thigh muscles occur early. Damage to the distal extremities is more severe: atrophy and weakness of the small muscles of the hands (especially thenar and hypothenar), pronounced weakness of the flexors and extensors of the hands and feet is detected.
Great difficulties arise in the differential diagnosis of TM and idiopathic polymyositis (6). Clinical similarities between these diseases have been found: pronounced general weight loss and increasing muscle weakness, early involvement of the neck flexors and pelvic girdle muscles in the process, the predominance of muscle weakness over the degree of atrophy; creatinuria. However, in polymyositis, in contrast to TM, muscle weakness is more common; Along with the proximal ones, the distal parts of the limbs are often involved in the process. The flexors and extensors of the hands and feet can be affected early and severely. Unlike TM, atrophied muscles are always weakened; there is never excessive folding in the area of the affected muscle. In muscle biopsies with polymyositis, signs of myofibril necrosis, phagocytosis, and regeneration with mononuclear infiltration are found, which is not found in TM. However, along with inflammation of the striated muscles, the development of polymyositis and other idiopathic inflammatory myopathies is often characterized by striking systemic manifestations, such as fever, Raynaud's phenomenon, skin lesions in the form of Gottron's papules over the interphalangeal and metacarpophalangeal joints, redness, hyperpigmentation, hyperkeratosis , peeling and cracking on the palms (the so-called “mechanic’s hands”), polymorphic rash, panniculitis, cutaneous vasculitis, non-erosive inflammatory arthritis and arthralgia, respiratory failure due to interstitial pulmonary fibrosis, which sometimes leads to pulmonary hypertension; myocarditis, manifested by severe rhythm and conduction disturbances, sometimes leading to congestive heart failure, damage to the gastrointestinal tract.
The study of thyroid function is of great diagnostic importance. If conventional methods fail to establish a definitive diagnosis and clinical evidence supports TM, ex juvantibus methylthiouracil should be prescribed followed by 24-hour urine creatinine determination (4). In case of thyrotoxicosis, its large doses (80 g/day) cause a significant decrease or disappearance of creatinuria within several days. The absence of regression of myopathy upon achievement of euthyroidism indicates in favor of polymyositis.
Clinical signs of muscle lesions that occur with steroid therapy may resemble those with TM (4). Weakness and atrophy of the muscles of the pelvic girdle and hips develop. At the time of muscle lesions, all patients, as a rule, have features of Itsenko-Cushing syndrome. Muscle atrophy is more pronounced than with TM. Simultaneously with changes in the muscles of the pelvic girdle, significant atrophy and weakness of the muscles of the forearms and hands are revealed. The electromyogram reveals mixed changes (myogenic and neurogenic). There is regression of myopathy after drug withdrawal. Pathological muscle weakness and fatigue are characteristic features of myasthenia gravis (4). Muscle weakness in TM is constant in nature and affects certain muscles. With myasthenia gravis, muscle weakness is more generalized, intensifying with the slightest physical exertion to the point where it is impossible to perform physical work. This causes the severity of various symptoms to fluctuate throughout the day. Ptosis, diplopia, limited upward and outward movement of the eyeballs, dysarthria, dysphagia, and amymia are also characteristic. TM can also be complicated by weakness of the bulbar muscles, but weakness of the external eye muscles, as well as “sagging” of the lower jaw due to pronounced weakness of the masticatory muscles themselves, is not observed. In patients with TM, unlike myasthenia gravis, the administration of anticholinesterase drugs is not accompanied by an increase in muscle strength, and the potential amplitude does not recover to normal.
In the treatment of TM, the most favorable results were obtained using a combined method: taking thyreostatic drugs followed by subtotal thyroidectomy. The results were worse when only conservative treatment was prescribed. However, with both methods, the signs of myopathy regressed slowly, over many months after the removal of thyrotoxicosis. These data, taking into account the results of histological, histochemical, and electroneuromyographic studies of skeletal muscles in patients and experimental animals with TM, made it possible to raise the question of pathogenetic treatment of the myopathy itself (5). Based on theoretical premises about the participation of cyclic nucleotides in the pathogenesis of muscle weakness in TM, the use of drugs that increase the level of c-AMP in skeletal muscle (allopurinol, aminophylline) should be considered indicated. To normalize calcium metabolism - sodium oxalate; drugs that improve skeletal muscle metabolism - vitamin B12, tocopherol, anabolic hormones. After relieving thyrotoxicosis, repeated courses of pathogenetic treatment of myopathy are quite justified.
Hyperthyroidism leads to increased bone turnover due to an increase in the number of osteoclasts and resorption surfaces, as well as a violation of the ratio of resorption and bone-forming spaces. Increased resorption is the cause of hypercalcemia, which occurs in almost 50% of patients with thyrotoxicosis, while the levels of PTH and 1,25(OH)2D3 are reduced and intestinal absorption of calcium is reduced. However, increased bone formation does not compensate for the sharp increase in bone resorption. As a result, bone mass in the proximal femur and spine is reduced. It should be noted that with an excess of thyroid hormones, women during menopause, patients with long-term untreated endogenous thyrotoxicosis, and persons receiving thyroid hormones in suppressive doses (more than 150 mcg of thyroxine per day) after surgery for thyroid cancer are most susceptible to osteoporosis. Osteopenia is primarily detected in bones with a predominantly cortical type of structure. Disorders of bone tissue metabolism are manifested in an increase in both indicators of bone formation (osteocalcin and alkaline phosphatase activity) and resorption (fasting hypercalciuria and increased excretion of hydroxyproline in the urine). The identified changes are directly dependent on the duration and activity of the disease and tend to normalize with persistent remission of the disease. A number of recent studies have shown that reduced bone mineral density in patients with thyrotoxicosis can be restored after achieving a euthyroid status (9).
In hyperthyroidism, periarthritis of the shoulder joints is most often observed (7). Damage to the periarticular tissues of the knee, hip, metacarpophalangeal and interphalangeal joints occurs with less frequency. X-ray reveals thickening of the joint capsule. Periarthritis in hyperthyroidism is usually resistant to treatment with corticosteroid hormones and disappears when thyreostatic drugs are prescribed. Acropathy in hyperthyroidism is characterized by a change in the shape of the distal phalanges of the fingers like “drumsticks”, stiffness in the joints, swelling of the soft tissues of the hands and feet without signs of inflammation. The most common changes are observed in the area of the metacarpophalangeal, proximal interphalangeal and metatarsophalangeal joints. X-ray reveals periosteal changes in the diaphysis of the bones, having the appearance of soap bubbles, which distinguishes their periosteitis observed in hypertrophic osteoarthropathy, pachydermopereosteosis, syphilis and hypervitaminosis A. The combination of acropathy with exophthalmos and pretibial myxedema in patients with diffuse toxic goiter is called Graves' disease. Acropathy can be observed with a disease duration ranging from several weeks to 28 years. In some patients, it develops after relief of symptoms of hyperthyroidism. There is no effective treatment (7).
Hypothyroidism
A disease characterized by severe tissue edema due to extracellular deposition of proteoglycans, which sharply increase the hydrophilicity of connective tissue. Hypothyroidism can be accompanied by the development of a number of rheumatic syndromes, in particular arthropathy and myopathy (7). Arthropathy is manifested by stiffness, swelling of the joints, and sometimes the appearance of effusion in the joint cavity, which is non-inflammatory in nature. Typically there is no joint tenderness on palpation. Typically, the knee, wrist, small joints of the hands (metacarpophalangeal and proximal interphalangeal), and metatarsophalangeal joints are symmetrically affected. In some cases, destructive arthropathy is observed with localization of changes mainly in the proximal interphalangeal joints and less often in the distal interphalangeal joints. When small joints of the hands and feet are involved, a differential diagnosis with rheumatoid arthritis often has to be made.
A number of patients may develop weakness of the ligamentous apparatus of the knee joints and form a Baker's cyst. In some cases, tenosynovitis of the hand flexor muscles is observed. A biopsy of the synovial membrane reveals its thickening without signs of inflammation, which is explained by the activating effect of TSH on synoviocyte adenylate cyclase. Crystals of calcium pyrophosphate are often found in the synovial fluid, which, as a rule, do not cause the development of attacks of pseudogout, which is explained by a decrease in the functional activity of neutrophil leukocytes (7). Prescribing thyroid hormone replacement therapy can provoke the development of pseudogouty arthritis. Despite the frequent increase in serum uric acid levels in patients with hypothyroidism, uric acid crystals are usually not found in the synovial fluid. The development of acute gouty arthritis is also uncharacteristic, although in some cases tophi are formed.
There is evidence of an increased incidence of ischemic bone necrosis. Necrosis of the lunate, tibial tuberosity, and femoral heads has been described (7).
Without treatment, in patients with hypothyroidism, calcium metabolism disorders are detected: there is a tendency to decrease the level of calcium in the blood and its excretion in the urine, the level of PTH and 1.25(OH) D3 increases. In patients, bone remodeling is slowed down - the rate of bone resorption and bone formation is reduced by 2-3 times. It is difficult to trace the dynamics of the influence of hypothyroid status on the condition of the skeleton, since patients are immediately prescribed treatment with thyroid hormones, which increase the rate of bone remodeling. A number of studies draw attention to an increase in the rate of bone loss. During the first year of thyroxine replacement therapy, an acceleration of bone loss in the spine and femoral neck was noted (8.9). At the same time, there is evidence of no bone loss in the radius after three years of treatment with thyroid hormones (9,13). Rozhinskaya L. Ya. et al. 36 women of reproductive age with various types of hypothyroidism were examined (postoperative - due to diffuse toxic goiter or nodulation due to autoimmune thyroiditis and congenital) (9). Women with untreated hypothyroidism showed signs of decreased bone formation and bone resorption, with no signs of osteopenia in the spine or proximal femur. In patients on replacement therapy, increased rates of bone turnover were detected, most pronounced in congenital hypothyroidism, which may be associated with the duration of therapy and the early (before peak bone mass) onset of the disease. In patients with postoperative hypothyroidism who underwent thyrotoxicosis, osteopenia of the proximal femur was detected. Thus, the development of osteopenia in hypothyroidism in premenopausal women is influenced by the duration of thyroid therapy and the early age of its initiation.
Hypothyroid myopathy is characterized by weakness and stiffness of muscles, mainly of the proximal parts of the arms and legs, painful cramps and nagging pain in the muscles, increased levels of serum creatine phosphokinase (CPK), and decreased tendon reflexes (2,3,7). There may be dysfunction of the facial muscles (dysarthria). Muscle atrophy is not typical for hypothyroidism. A typical muscle disorder is myopathy with muscle hypertrophy (Hoffmann syndrome). In addition to weakness and stiffness, it is characterized by cramps, an increase in muscle volume and density. Muscle hypertrophy is associated with an increase in muscle fibers due to the deposition of proteoglycans in them. When thyroid hormone replacement therapy is prescribed, muscle symptoms disappear completely.
Signs of damage to the peripheral nervous system occur in the vast majority of patients with hypothyroidism. They are manifested by numbness, paresthesia, pain in the distal parts of the extremities, often accompanied by wasting of the muscles of the hands and, occasionally, the muscles of the feet. Carpal tunnel syndrome is often observed, which develops due to compression of the median nerve by the flexor ligament in the wrist joint due to swelling and tissue hardening characteristic of hypothyroidism, which causes characteristic nocturnal paresthesias, which sometimes progress to loss of sensitivity and muscle weakness of the finger when the thumb is abducted (2, 7). According to Steven G. Atcheson, carpal tunnel syndrome associated with hypothyroidism ranked first among the metabolic causes of this syndrome and occurred in 41 (13.8) of 297 patients with carpal tunnel syndrome, while in hyperthyroidism it was observed in only 1(0.3) of these patients (10).
Hyperparathyroidism
It is primarily characterized by excessive secretion of parathyroid hormone by adenoma or hyperplastic tissue of the parathyroid glands, which leads to a sharp activation of bone metabolism with a predominance of resorption processes. Damage to the skeletal system is manifested by pain in the bones, most often in the limbs, aggravated by movement, and pain on palpation of the bones. Later, skeletal deformities occur, the so-called “duck” gait, fractures of the limb bones at the slightest injury, and sometimes spontaneously. Generalized osteoporosis occurs, which is one of the main manifestations of hyperparathyroid osteodystrophy.
The classic manifestation of long-term hyperparathyroidism is osteitis fibrocystis (osteodystrophy). It is based on high activity of osteoclasts and lacunar resorption of bone elements with the subsequent development of fibrous tissue, the formation of cysts and giant “brown” tumors (reminiscent of osteoclastoma of bone). Cysts and giant tumors are located in the diaphysis of long tubular bones, ribs, lower jaw, bones of the wrist, pelvis, and skull. When percussing over the skull cysts, a “watermelon sound” is detected (7). A peculiar osteoporosis of the bones of the calvaria is characteristic - spongy, as if “moth-eaten”, can have the appearance of “frosted glass”, often resembles “clumps of cotton wool” - pagetoid form of hyperparathyroidism (1). In contrast, in Paget's disease, blood tests show an increase in the concentration of alkaline phosphatase with normal concentrations of calcium and phosphorus, despite a 40-50-fold acceleration of metabolic processes in the bone (15). Clinically they manifest as vague pain in the bones, sometimes palpated as tumors. After anectomy, the parathyroid glands may become ossified. Gradually, curvature of long tubular bones (legs, thighs) and increased curvature of the spine may occur (1.7). Today, the classic picture of osteitis fibrocystis is becoming less common, since the diagnosis of primary hyperparathyroidism is usually made at the stage of asymptomatic hypercalcemia (2).
An early radiological sign of hyperparathyroidism is subperiosteal resorption of bone tissue, which consists of subperiosteal resorption of bone substance, most often the middle and terminal phalanges of the fingers, mainly on their radial side (1,7). At the same time, the terminal phalanges seem to be “moth-eaten”, “sucked”. After removal of the parathyroid glands, resorption stops. Bone resorption is often accompanied by subperiosteal erosions in the area of the middle phalanges, carpal bones, proximal tibia and femur, both ends of the clavicle, pubic and sacroiliac joints. With erosions in the small joints of the hands, there may be arthralgia, swelling, and morning stiffness, which requires a differential diagnosis with rheumatoid arthritis. There may be a breakthrough of the cyst into the joint cavity, which leads to the development of synovitis (usually the knee). Less commonly, hypermobility occurs due to weakness of the ligamentous apparatus and joint capsule, which may be accompanied by tendon rupture (usually the quadriceps femoris tendon).
In 35-50% of patients with long-term primary hyperparthritis, chondrocalcinosis is detected, accompanied by asymptomatic calcification of the menisci, knee cartilage, wrist joints, intervertebral discs, triangular cartilage of the wrist, which can lead to carpal tunnel syndrome (2,7). After parathyroidectomy, acute attacks of pseudogout may occur. With hyperparathyroidism, hyperuricemia also occurs with the development of gouty arthritis. Muscle damage is manifested by weakness of the proximal muscles without an increase in the content of muscle enzymes in the blood serum, myalgia, and atrophy. Symptoms usually disappear after parathyroidectomy.
Hypoparathyroidism
It exists in two forms: hypoparathyroidism and pseudohypoparathyroidism (Albright's syndrome), in which the secretion of PTH is not affected, but due to the insensitivity of target tissues to its action, the same biochemical and clinical disorders develop as in hypoparathyroidism (12). One of the few clinical differences between Albright's syndrome and idiopathic hypoparathyroidism is a peculiar skeletal symptom complex: a round face, a short neck, a wide, stocky body, growth retardation, shortening of the metacarpal and metatarsal bones, and in some cases, the phalanges of the fingers; subcutaneous calcifications are detected in the area of large joints; Asymptomatic hyperuricemia is observed. The disease is familial in nature. A characteristic combination of a decrease in calcium and an increase in phosphorus in the blood serum is observed in hypoparathyroidism, Albright's syndrome and resistance to PTH in patients with chronic renal failure. A particularly rare complication is myopathic syndrome, manifested by weakness of the proximal muscles of the limbs, decreased deep reflexes, increased blood CPK, in the absence of changes in electromyographic parameters (11). One of the manifestations of myopathy may be ptosis, tetanic convulsions, often in the distal muscles of the limbs; painful spasms of the muscles of the chest or anterior abdominal wall, simulating acute diseases of the chest and abdominal organs, arising mainly due to damage to the nervous system. As a result of treatment with vitamin D2, muscle weakness regresses, which is accompanied by a decrease in blood CPK levels (11).
With hypoparathyroidism, spinal damage is observed, reminiscent of idiopathic ankylosing skeletal hyperostosis, but unlike it, it is accompanied by stiffness and limitation of movements. X-ray reveals ossification of the spinal ligaments with normal iliosacral joints (7). With hypoparathyroidism, osteosclerosis, periostosis of long tubular bones, premature calcification of the cartilage of the ribs, band-like compactions of the metaphyses, transverse metaphyseal “growth lines” occur, calcification of soft tissues is observed (choroid plexuses of the brain, vascular walls, dura mater, basal ganglia, lens, skin) (1).
List of used literature
- Bukhin V.S. “Problems of endocrinology” 1983 v. 29 No. 6. To X-ray diagnosis of hypo- and hyperparathyroidism.
- West S.J. Secrets of rheumatology / Transl. from English - M.-SPb. “Publishing house BINOM” - “Nevsky dialect”, 1999.-768 p., ill.
- Ilyina N.A. “Clinical Medicine” 1983 No. 9. Myopathic syndromes
- Kazakov V.M. “Clinical Medicine” 1991 vol. 69 No. 1. Differential diagnosis of thyrotoxic myopathy.
- Kazakov V.M. “Journal of Neuropathology and Psychiatry named after. Korsakov” 1987 vol. 87 issue. 3. Thyrotoxic myopathy (clinic, diagnosis, treatment).
- Nasonov E.L., Shtutman V.Z., Salozhin I.V., Guseva N.G., Nasonova V.A., Plotz P. “Clinical Medicine” 1995 No. 2. Clinical and immunological heterogeneity of idiopathic inflammatory myopathies.
- Nasonova V.A., Bunchuk N.V. Rheumatic diseases. Guide for doctors. M., Medicine. 1997, 520 p.
- Ribot C., Tremollieres S. et al. Bone mineral density and thyroid hormone therapy.- Clin. Endocrinol.- 1990-Vol 33, P143-153.
- Rozhinskaya L.Ya. Systemic osteoporosis: A practical guide. 2nd edition, revised. and additional –2000, 196 pp.
- Steven G. Atcheson. Carpal Tunnel Syndrome: Is it Work-Related? Hospital Practice. 1999, 03.
- Stekhin P.E. Journal of Neuropathology and Psychiatry named after. Korsakova 1982 t 82 issue 11. Myopathic syndrome and other neurological disorders in familial pseudohypoparathyroidism.
- Stern LZ, Fagan JM- In: Handbook of clinical Neurology Amsterdam, 1979 V 41, Pt 2, Z 246-248.
- Toh SH, Brown PH Bone mineral content in hypothyroid male patients with hormone replacement: A 3-year study J. Bone Mineral Res. 1990 Vol. S. P463-467.
- Ramsay//Lencet- 1996- Vol. 2 – P931-935; Ramsay ID Thyroid Disease and Muscle Dysfunction-London 1974 P 57
- Kumar P., Clark M. Clinical Medicine, 4th ed, 1999, P 501-513. Consilium medicum 2000, volume 2 no. 6.
Traditional methods
Only hormonal therapy can get rid of excess swelling by establishing hormonal balance in the body. Traditional methods can only eliminate some symptoms. In combination with therapy, to eliminate edema in hypothyroidism, it is recommended to use the following herbs:
- Field horsetail.
- Bearberry.
- Anise.
- Parsley.
- Eleutherococcus.
- Lily of the valley.
Before starting to use any herbal raw materials, you should definitely consult with your doctor, since some herbal components can aggravate the situation if they are not compatible with the patient’s medical history.
Soy products and seaweed (kelp and cabbage) will help eliminate swelling. They perfectly replenish iodine deficiency and improve the condition of the body.
Thyrotoxicosis and pregnancy
If a woman develops thyrotoxicosis, pregnancy is practically impossible due to numerous disturbances in the hormonal levels and the reproductive system as a whole. If conception does occur, then such a patient should register with the antenatal clinic as soon as possible.
The danger of pathology for expectant mothers and babies is the formation of congenital deformities in the fetus against the backdrop of disease progression (all chronic diseases worsen during pregnancy).
If a woman knows that she has thyrotoxicosis, then pregnancy should definitely be planned. Planning includes a full examination, course of treatment and consultation with an endocrinologist. With the right approach, a woman can carry and give birth to a healthy child.
Causes of thyrotoxicosis
An increase in hormones - thyrotoxicosis, leads to an increase in the body's need for oxygen and increased heat production.
This is expressed in such signs as severe sweating, tachycardia, hand tremors, and anxiety.
The cardiovascular system is disrupted, changes occur in the skin, hair, and eye diseases appear.
Eye diseases are mainly associated with impaired movement of the eyes and facial muscles.
Most often it is unilateral. The autonomic system plays a certain role in this.
The reason is the increased tone of the extraocular muscles, the volume of tissue and fat increases.
All this leads to stagnation in the eyelids, increased pressure and swelling.
At the first suspicion of a disease, you should contact an endocrinologist and undergo diagnostics.
It includes an examination of hormone levels in the blood, ultrasound findings and a cardiogram.
Preventive measures
First you need to take care of your immunity and improve your lifestyle. To do this, give up all bad habits, if any, play sports and protect yourself from stress. Don't forget about proper nutrition. Fresh fruits and vegetables have a beneficial effect on the overall health of the body. Thanks to healthy food, you can protect yourself from protruding eyes. After all, a common cause of this phenomenon is Trichinella, which is found in raw pig fat.
If a person is seen by a doctor due to any illness, he must follow all his instructions. Otherwise, the result of an irresponsible attitude towards one’s health may be bulging eyes. At the initial stage, the disease does not bring any trouble, but no one is immune from complications.
It is much easier to prevent any disease than to treat it later. Exophthalmos is no exception. In order to see well and not lose your vision forever, do not neglect visits to ophthalmologists, seek advice on every question that arises.