Just what the doctor ordered
Who is suitable for laser vision correction? And does it have any contraindications?
Elena, Moscow
– First of all, this is not a medical, but a cosmetic procedure; it is not done according to medical indications, but only at the request of the patient himself. Excimer laser correction is intended for people with visual impairments who are tired of wearing glasses and contact lenses or for some reason cannot do so. There is also a professional need for laser correction: among the military, athletes.
These operations cannot be performed on children under 18 years of age, because until this age the eyeball is still developing. The second important condition is that the patient has stable refraction (visual acuity) over the past 1.5-2 years. An absolute contraindication for laser correction is progressive myopia. In this case, the result of the operation will not last long.
Eye diseases (glaucoma, cataracts, acute and chronic inflammatory diseases, keratoconus, corneal dystrophy) may also be contraindications for laser correction. Wearing contact lenses for a long time also has a negative impact on the cornea. In this case, it is necessary to carry out rehabilitation measures, preparing the eyes for future surgery.
Indications for surgery
The procedure allows you to restore vision without using glasses or contact lenses. Shown:
- patients over 18 years of age with refractive errors - myopia, astigmatism, hypermetropia;
- if the acuity of visual perception has not changed over the past year;
- if the disease worsens vision and progresses;
- if there are no other eye health problems that are a contraindication to laser correction.
Additionally, if the doctor has said that the patient is not a candidate for LASIK due to a thin cornea, then Epi-LASIK is an excellent opportunity to improve visual perception.
Success rate
How long does the effect of the operation last? Can there be complications and any restrictions after surgery?
Timofey, Moscow
– A positive effect is observed in approximately 98% of patients. Complications, as with any other surgical intervention, are possible. But competent selection of patients and the necessary preoperative preparation can reduce the risk.
After the operation, there are few restrictions: you should wear sunglasses for one month, you should not visit the sauna and swimming pool for two months, you should not lift weights, drink alcohol or carbonated drinks for a month, you should not use eye makeup or work on a computer for two weeks. It is not advisable for women to plan a pregnancy in the next year after surgery.
Complications
Serious complications with Epi-LASIK are extremely rare.
Epi-LASIK is a safe, effective and permanent procedure, but like any surgical procedure, there are some risks. The risks and complications associated with this procedure are reduced or eliminated through careful patient selection and preoperative testing using the latest diagnostic technologies.
Complications:
- dry mucous membrane;
- poor night vision;
- glare or halos around light sources;
- increased sensitivity of the eyes to sources of artificial and natural light;
- scarring of the cornea;
- infection.
Eye under the gun
What procedures must include a special ophthalmological examination before surgery?
Olga, Yelets
– There are quite a lot of them, but all together they will take no more than 1-2 hours. Autorefractometry is the first study that can determine the degree of visual impairment. The patient sits in front of a special autorefractometer device, brings his face closer to it, and places his chin on the stand. And for several seconds he looks at the object indicated by the doctor. The next stage is visometry (determining visual acuity) using a phoropter apparatus. The patient looks through different lenses at the sign chart. Checks visual acuity of the right, left, then both eyes together without correction and with optimal optical correction. Intraocular pressure is then measured using a pneumotonometer.
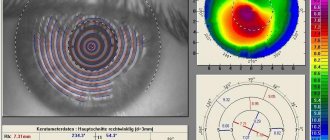
Next, keratotopography is done. With its help, the doctor receives a topographic map of the patient's cornea. This is an informative and absolutely necessary study. Without it, excimer laser correction cannot be done. All that is required of the patient is to look into the eyepieces of the device for a couple of seconds. If the cornea is too steep or, conversely, too flat, then LASIK is not suitable for such a person. Atypical corneal texture can be either congenital or acquired - for example, after wearing hard contact lenses for a long time. In this case, a person just needs to remove the lenses and within two months the cornea will take its natural shape.
All patients must undergo a tear test. By placing thin strips painted with a special composition into the lower conjunctival fornix, a conclusion is made about whether the patient’s eyes have enough of this important fluid. Next, biomicroscopy is performed - the condition of the anterior segment and optical media of the eyeball is checked.
Then an ultrasound of the eyeball is performed. The patient lies down on a couch, anesthetic drops are instilled into both eyes, and an ultrasound probe is placed on the surface of the cornea. Using echobiometry, the length of the anterior-posterior axis of the eyeball, the depth of the anterior chamber, and the thickness of the lens are measured. Next, pachymetry is performed - measuring the thickness of the cornea. The choice of correction method depends on its results. If the thickness of the patient’s cornea is less than 500 microns, then the LASIK method is categorically not suitable for him due to the risk of serious postoperative complications. In such cases, the patient is recommended a second, no less effective method of laser correction - PRK.
Next, the patient must be instilled with drops to dilate the pupils. Autorefractometry, visometry in conditions of dilated pupils and a very important study - ophthalmoscopy (detailed examination of the central and peripheral parts of the retina) are carried out. Only the entire complex of these studies can tell the doctor about the true state of the patient’s organ of vision.
Description of the Epi Lasik operation
Operation stages
Step-by-step procedure:
- instill the anesthetic drug several times at intervals of 1–3 minutes;
- an epithelial flap is created by separating the upper epithelial layer from the cornea;
- moves to the side;
- excimer laser changes the structure of the cornea;
- the epithelial flap returns to its original position.
A bandage is applied and will be removed after a few days.
After the procedure, the patient will receive a prescription for pain-relieving eye drops—usually an anti-inflammatory medication and an antibiotic to reduce the risk of infection.
PRK or LASIK?
How do laser correction methods differ from each other? Which one is preferable?
Svetlana, Tambov
– The two main methods of excimer laser correction are PRK (photorefractive keratectomy) and LASIK (laser-assisted intrastromal keratomelosis). The rest - REIK, LASEK, Epi-LASIK, super LASIK - are just variations of these methods.
LASIK is the undisputed favorite today. Unlike PRK, visual functions after surgery with this method are restored very quickly, and the rehabilitation period is short and painless. But if there are contraindications for LASIK surgery, PRK may be a worthy alternative.
Contraindications
The procedure is not performed on women during pregnancy and breastfeeding. Epi-LASIK is contraindicated in patients with Bowman's membrane striae or a history of corneal surgery.
This operation is suitable:
- if the patient suffers from eye diseases or pathologies of the retina/optic nerve (keratoconus, glaucoma, cataracts, cornea, herpes, herpes zoster);
- if you have autoimmune diseases (multiple sclerosis, rheumatoid arthritis, lupus);
- in the presence of diabetes, collagen vascular diseases.
Laser correction is not performed if the patient is taking steroids or immunosuppressants.
Chick - and you're done!
How is the laser correction procedure performed?
Alexander, Nizhny Novgorod
– The procedure itself takes on average 20 minutes (both eyes are operated on). PRK, like LASIK, is done under local anesthesia. Before the procedure, the patient is instilled with antibacterial drops, and the skin of his eyelids and face is treated with a weak iodine solution (then this “paint” will be washed off and the person will go home with a normal complexion). The patient's face is covered with a sterile napkin with two round holes for the eyes. An eyelid dilator is applied to one eye (which will be operated on), after dropping pain-relieving drops into it (it will not allow you to blink). Next, they ask you to fix your gaze on the green light. During PRK, the epithelium is removed from the surface of the cornea, then the optical zone is treated using an excimer laser beam. The duration of its exposure depends on the degree of visual impairment. Next, antibacterial and moisturizing drops are instilled into the eye and an aseptic bandage is applied (in some clinics, therapeutic contact lenses are used instead of bandages).
The patient will then have to endure what is called corneal syndrome for the next three days. Its symptoms: pain, stinging, severe lacrimation, photophobia, feeling of a foreign body in the eye. Analgesics will help alleviate these sensations (but no more than 3-4 tablets per day). For the first 4 days, it is necessary to instill drugs into the eyes 5 times a day to help prevent infection and quickly restore the corneal epithelium. From approximately the 4th day after surgery, in order to maintain the transparency of the cornea, local steroid drugs are instilled for two months according to a decreasing scheme. Distance visual acuity after PRK is restored to normal within 7-10 days, near - within 10-14 days.
After LASIK surgery there is virtually no pain, visual functions are restored quite quickly, and the postoperative rehabilitation period is short.
Advantages of SMILE over PRK
- Absence of pain and long rehabilitation: because When PRK removes the epithelium and the surface of the cornea remains “naked,” then for the period of complete epithelization (up to a week), the patient must wear protective contact lenses and use special medications (study “Results of SMILE and PRK correction for low myopia”).
- Possibility of developing corneal opacities – because If there is an inflammatory process, then at the site of operation of the excimer laser during PRK, the formation of opacities from minor (“haze”) to pronounced scars is possible, which can lead to a significant decrease in vision. To reduce the risk of such complications, a special drug, mitomycin, is used, but this substance negatively affects the posterior surface of the cornea (endothelium) and increases the patient’s pain in the postoperative period.
- The risks of infectious complications with PRK are much higher than with ReLEx SMILE, because during a long rehabilitation period, there is a “wound surface” where bacteria can enter and cause inflammation – keratitis.
- With SMILE, the superficial nerve plexus of the cornea is not injured, its normal sensitivity is preserved.
- As studies show (“Comparison of biomechanical properties” and “Mathematical model of tensile strength”), the strength of the cornea after ReLEx SMILE remains higher than with PRK, which is important for reducing the development of the risks of keratoconus.
Effect after Epi Lasik surgery - is it worth doing?
Epi-LASIK results are comparable to traditional LASIK, meaning much less reliance on corrective lenses and clearer vision. This is a testament to the advancements in vision correction technology and surgical techniques over the years.
It will take 6–7 months for the eyes to heal completely. Epi LASIK requires a slightly longer recovery period than LASIK.
The results of the operation are permanent. However, laser correction cannot prevent the natural deterioration of vision that happens over time.
What is better: Lasik or Femtolasik?
First you need to understand the difference between these two methods.
And it lies in the method of forming the corneal flap. With the Lasik technique, a special mechanical microblade is used for this. Both methods are effective and have good reviews among patients. They are safe and painless. Therefore, you need to choose the lasik or femto lasik method based on individual medical indications, the financial capabilities of the patient and the technical equipment of the clinic where the operation will be performed.
Basic methods of laser correction
All methods of laser vision correction can effectively combat disorders of the optical system of the eye. The essence of each of them is quite simple:
- Cutting the upper part of the cornea of the eye and forming a flap of tissue.
- Removal of part of the transparent layer of the cornea (stroma) to change the degree of refraction of light rays.
- Returning the formed flap of tissue to its place.
The consequence of the operation is a significant improvement in vision. As a rule, after laser correction, patients stop using glasses or contact lenses.
Currently, ophthalmologists use various methods of laser vision correction:
- Lasik
- PRK
- Lasek
- Super lasik
- Femto-lasik.
This method appeared in 1989. The advantage of the method is that such an operation does not affect the surface of the cornea. The upper layers are lifted using special devices (microkeratome), freeing the middle layers for laser evaporation.
The entire correction operation can be performed within one day, and on both eyes at once.
The recovery period after such an adjustment passes very quickly, and a positive result is almost 100% guaranteed. In addition, the operation is completely painless. More information about the methods of performing the operation can be found here.
LASIK is currently considered the most gentle method of vision correction, since it completely preserves the anatomy of the layers of the cornea.
We suggest you read: Are there any nuances after correction using the LASEK method?
The first such correction was carried out back in 1985. For laser vision correction using the PRK method, a special gas laser (excimer) is used.
The operation in this case occurs using non-contact laser action on the upper layers of the cornea. The internal structure of the eye is not affected at all.
As a result, vision improvement occurs due to microdistortions of light rays in the outer layer of the cornea.
Unfortunately, PRK has many disadvantages:
- Long-term healing of corneal tissue.
- The need to use eye drops for a long time.
- The operation cannot be performed on both eyes at once.
This method was invented and applied in 1999 by Italian ophthalmologist Massimo Camelin. LASEK is used if the surface layers of the patient’s cornea are quite thin and it is not possible to use the LASIK method.
If you look at it, this method is a slightly improved photorefractive keratectomy (PRK).
The essence of the operation is to apply a formed epithelial flap to the surface layers of the patient’s cornea. I must say that this technique is somewhat more painful than LASIK. In addition, recovery after surgery takes longer.
SUPER LASIK
This is a completely new technique that meets all modern ophthalmology standards. The essence of the method is a very precise “grinding” of the surface of the cornea in accordance with the program included in the laser installation.
Before the operation, the patient undergoes a special examination using WaveScan, a wavefront analyzer. The analysis takes into account all wave distortions that occur not only in the cornea, but throughout the entire ocular optical system.
Today SUPER-LASIK is the most advanced method of laser vision correction. It allows you to fight not only farsightedness, myopia or astigmatism, but also more complex disorders of the visual system. In this case, the patient regains almost one hundred percent vision.
FEMTO-LASIK
This method is also often called Intra-Lasik or all-laser LASIK (in the English version AllLaserLasik). It was first used relatively recently - in 2003. Essentially, this is the same LASIK, but the upper layers of the cornea are lifted not with a steel microkeratome blade, but with a special femtosecond laser.
We invite you to familiarize yourself with OCT of the optic nerve after LASIK