Loss of vision (total or partial)
Loss of vision
is a problem whose solution cannot be delayed. Patients with this diagnosis experience complete or partial loss of vertical or horizontal visual fields, a gradual decrease in visual acuity, up to complete blindness.
The first steps to restoring the basic functions of the visual system are timely diagnosis of the causes of vision loss and the underlying disease that provoked a sharp deterioration, and the prescription of drug or surgical treatment.
Quality of life in patients who suddenly lost vision in one eye
People who have lost an eye need a long period of adaptation to their condition, daily activities, driving a car, and performing various jobs.
In order to identify what problems patients experience during the period of adaptation to monocular vision and determine its duration, we examined the quality of life (QoL) in 65 patients suddenly blind in one eye using the SF-36 questionnaire and a specially designed questionnaire. In the initial period after the injury, we found a statistically significant (p < 0.05) decrease in all quality of life parameters compared to a group of healthy individuals and individuals who had long adapted to monocular vision. This indicated a decrease in well-being in all spheres of life of the study population and the presence of psychological, physical, everyday, social and professional problems.
The presence of similar problems was noted in their studies by Schiff (1980), Schein (1988), Knoth (1995), Cooper (2000), N. Buys, J. Lopez (2004).
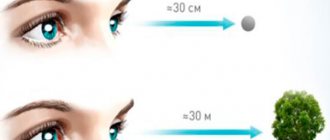
The most pronounced decreases in quality of life indicators were on the scales of “household activity,” “production activity,” and “orientation outside the home.” This was associated with a sudden loss of binocular vision, impairment in assessing the distance and depth of space and, because of this, difficulties arising both in performing the simplest functions (performing cosmetic procedures, housework, etc.) and in production activities.
Indicators of role functioning (the role of physical and emotional factors) and psychological well-being suffered to a greater extent, which was determined by the influence of subjective factors. Thus, all respondents felt that their lives had changed greatly after the injury; to varying degrees, they experienced feelings of restlessness, anxiety, and mood swings due to the loss of vision in one eye; many had fears that their vision might deteriorate; one patient admitted that tried to commit suicide.
Low values of QoL indicators characterizing vision-related activities were recorded. Almost all respondents in the main group noted that they began to get tired faster during their traditional visual work, when watching television. Most respondents noted tension when reading and difficulty viewing distant objects located at a distance of more than 5 meters. In all likelihood, this was due to a decrease in the field of vision on the side of the injured eye and fatigue of the accommodative apparatus of the fellow eye.
A decrease in indicators characterizing social functioning occurred in 70% of cases. Some patients associated low social activity (limited contacts, acquaintances, visits to public places) with poor vision and difficulties in orienting in an unfamiliar space, others with a feeling of inferiority, anxiety, depression, and personal experiences. It seemed to many that the sight of an injured eye was unpleasant to others, while others explained this by constant fatigue.
As patients adapted to monocular vision and depth perception was restored, all indicators of quality of life improved (significant changes occurred 9 months after injury). By 1 year, the average values of QOL indicators did not differ from those of healthy people. But on the “psychological well-being” and “production activity” scales, even by a year after the injury, statistically significant differences (p<0.05) remained between the indicators of the study and comparison groups. This indicated that not all patients completed the adaptation process by the specified period. 35% of the respondents had psychological problems and difficulties in the professional sphere.
Causes of complete or partial loss of vision
The causes of vision loss can be associated both with pathology of the visual system and with other diseases. Even the most harmless mild head injury or systemic disease can be dangerous.
The most common reasons that can provoke complete or partial loss of vision:
- Inflammation of the mucous membrane of the eye due to infection or allergens
- Trauma to the front and back of the head
- Postoperative complications during long-term rehabilitation
- Infectious diseases aggravated by complications from ENT organs, lesions of blood vessels
- Stress, fatigue, excessive mental stress
- Failure to maintain visual hygiene when working with electronics and equipment.
And also against the background of other diseases:
- Diabetic retinopathy (damage to the vessels of the retina in diabetes)
- Trachoma is a chronic infectious eye disease caused by chlamydia.
- Macular degeneration (a retinal disease that affects the macula (yellow spot) located at the back of the eye)
- Glaucoma (increased intraocular pressure)
- Cataracts (clouding of the lens) and other diseases that affect the blood vessels and nerve endings of the eyes.
Short-term vision loss
Temporary blindness is called “intermittent blindness” in scientific medical circles. This symptom is most often diagnosed in people over sixty years of age, but can occur at any age. It represents a sharp deterioration in vision, a person is absolutely unable to distinguish details, or a certain narrowing of the field of vision, when so-called “blind spots” arise, in which a person partially or completely sees dark spots in front of him. This temporary loss of vision most often occurs in one eye, but there are cases when darkening occurs in both eyes. A person may suddenly lose vision and remain in a state of vision for up to twenty minutes. Such a temporary blackout. As a rule, it indicates problems of a cardiovascular nature and are symptoms of a heart attack or stroke.
Types of partial or complete vision loss
With complete, absolute or total loss of vision, the Patient sees nothing, but he retains the sensation of light and color.
Partial vision loss is possible with:
- Color blindness is an eye disease associated with the inability to recognize colors or their shades
- Night blindness and snow blindness - poor vision at dusk and at night
- Temporary impairment, for example, caused by strong exposure to ultraviolet radiation on the organs of vision.
Loss of vision is also possible with diseases such as: ischemic (damage to the optic nerve) and toxic (disease of the peripheral nerves) neuropathy, increased intracranial pressure, infarction of the occipital lobes of the brain, hysteria.
The provoking background for the appearance of complete or partial loss of vision can be arterial hypotension (persistent increase in blood pressure from 140/90 mm Hg and above), anemia (decreased hemoglobin concentration in the blood), massive blood loss due to surgery or injury.
A sharp decrease in vision is a signal from the body that cannot be ignored. We recommend that you seek help from specialists as soon as possible.
Stroke and Vision Loss: Warning Signs and Recovery
Many stroke patients complain of various visual impairments. What they are like and how the ability to see after a stroke is restored is discussed in this article.
Symptom of a “mini-stroke”
Loss of vision on the left or right side of the visual field may be a sign of a transient ischemic attack (TIA). It is called a “mini-stroke” because the symptoms and causes are the same as a stroke, but disappear after a few minutes or hours. Also, with a transient ischemic attack, computed tomography and MRI will not show brain damage.
Vision loss occurs differently due to TIA and stroke. Often symptoms affect only one eye. In this case, at first there is a feeling that everything is visible through a haze, and only then does vision completely disappear. However, this does not last long, which is why this disorder is called transient monocular blindness.
As a result of a stroke
After a stroke, various visual impairments may appear: color vision anomalies, inability to recognize objects, faces, and movement. They arise as a result of damage to the visual cortex of the brain. These changes can negatively affect recovery after a stroke—as doctors report, about 20% of patients will not recover visual function to the same extent.
Types of Visual Impairment
- hemianopsia - one-sided blindness. If the stroke occurs in the left hemisphere of the brain, the right visual field in each eye will be affected. If this happened in the left hemisphere, then the left sides will be affected.
- Quadrantopsia is the same as hemianopsia, but it causes vision loss of a quarter rather than half of the visual field.
- Scotoma is a disorder in which blind spots appear. Scotoma is also a name for vision loss in which the affected area is smaller than with hemianopsia and quadrantopsia.
- Tunnel vision is a loss of peripheral vision that makes it appear as if there are blinds in front of your eyes. Appears in both eyes if the stroke occurred in both hemispheres of the brain.
How is vision restored after a stroke?
Treatment depends on how badly your vision is affected. Most often, it will be aimed at compensating for emerging shortcomings. If your eye movements are impaired, your doctor may prescribe glasses with prisms or glasses with a single lens to correct double vision. Eye exercises may also be prescribed, although their effectiveness has not yet been proven. To make it more convenient for the patient to read, the doctor may suggest using a magnifying glass, improved lighting, and choosing texts with a larger size.
Although vision loss from a stroke can be significant, there are certain ways to compensate for it.
Source
Diagnosis and treatment of partial or complete vision loss
We recommend that you consult an ophthalmologist as soon as you notice a sharp drop in vision, blind spots appear during vigorous activity, in an excited or overexcited state.
To check vision, Dr. Belikova’s Eye Clinic uses a comprehensive diagnostic examination, including a complete examination. The patient is assigned a attending physician who will accompany him during the prescribed complex treatment.
In our clinic, only experienced ophthalmologists of the highest and first categories, laser surgeons, Ph.D., as well as Doctor of Medical Sciences, Professor Elena Ivanovna Belikova personally receive treatment.
Sign up for a full diagnostic examination, we will definitely take care of the health of your eyes.
Take care of your vision and remember that nothing can replace the bright colors of the world around you if you suddenly lose it.
Classification of color vision disorders
To make a diagnosis, a doctor must classify the type of color vision disorder in a child or adult. Most often, the patient does not perceive only one color. But there are times when a person sees the world around him in black and white.
There are several types of color blindness:
- Protanopia. When a person has the disease, there are no cones on the retina that perceive red colors. The pathology is quite rare and occurs more often in men. In such patients, the difference between red, orange, and yellow colors is reduced.
- Deuteranopia. If the patient has the disease, there are no cones on the retina that perceive a green tint. The disease belongs to a rare category that most often occurs in men.
- Tritanopia. A disease in which the perception of many colors is impaired. This is a fairly rare disease that occurs in both men and women. When sick, a person does not perceive short light waves. Red and green colors are overly dull for him, almost gray. Patients see the violet shade as red.
- Lack of perception of any colors. Pathology refers to both congenital and acquired forms. A person does not perceive all shades; surrounding objects are seen in black and white colors.
- Retinal damage. Only acquired diseases fall into this category. The reasons may be neurological conditions, retinal nutritional disorders.
The main difference between congenital and acquired defects is in treatment. The first type cannot be treated. The patient will need to learn to live with color vision impairment. Acquired defects are completely eliminated after treatment, if possible.