Diabetes mellitus is a dangerous disease in which blood sugar becomes higher than normal. This occurs due to insufficient insulin production. This disease affects the blood vessels of various organs, including the retina. That is why such patients often have vision problems.
Many people receive a diagnosis of diabetes mellitus when they visit an ophthalmologist, complaining of dark spots before the eyes, blurred objects, etc. And this is not surprising, since with this disease changes in the fundus of the eye occur, which can only be noticed during examination.
The main eye diseases that diabetics face are cataracts, glaucoma and diabetic retinopathy.
Diabetes mellitus and vision: is there a connection, how does it affect the eyes?
Diabetes mellitus begins to affect vision early in its development and is the leading cause of blindness in adults aged 20-75 years. Elevated blood glucose levels cause swelling of the lens, which affects the ability to see clearly.
Diabetes mellitus negatively affects the condition of blood vessels, the tissues of the eyeballs are poorly supplied with oxygen, and if a person does not undergo treatment and ignores the symptoms, then already in the first 5 years after diagnosis, patients begin to go blind.
Diabetes can cause temporary myopia, but if a person corrects and maintains normal sugar levels, vision will be restored.
Is blindness real?
Complete blindness in diabetes mellitus is quite real, but it does not occur immediately; complications develop gradually.
First, high blood sugar levels cause small blood vessels in the retina to become blocked. If there is no treatment at this stage, then blood circulation is disrupted - this leads to chronic oxygen starvation of the tissues of the organs of vision. The body will definitely compensate for this condition, which leads to the growth of new vessels in the eye - they are small and fragile, often burst, and hemorrhage only aggravates the clinical picture.
The result of the described process is “wrinkling” of the retina, its detachment and complete loss of vision, which is already irreversible.
Eye diseases in diabetes: glaucoma, cataracts, retinopathy
Three eye diseases most often develop with diabetes are glaucoma, cataracts and retinopathy. At the same time, diabetic retinopathy accounts for 70-80% of all cases, and the rest only 20-30%.
Diabetic retinopathy
This complication of diabetes mellitus of a vascular nature is associated with irreversible damage to small vessels in the retina of the eyeball. The longer a person refuses treatment for diabetes, the more he violates the rules and recommendations from the endocrinologist, the faster the destruction of blood vessels will occur.
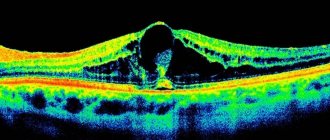
As the disease progresses, vision also deteriorates: at first the patient simply sees everything “in a fog,” then parts of the picture literally begin to “fall out” - this means that the cells of the eyeball are already dying. Diabetic retinopathy occurs in 4 stages, the most dangerous is considered to be the one in which fibrous tissue grows and retinal detachment occurs. If surgical intervention is not performed at this moment, the patient will become completely blind.
Glaucoma
The formation of new blood vessels in the eyeballs is the cause of increased eye pressure, which leads to the development of glaucoma. This disease is accompanied by severe symptoms:
- light circles/halos appear before your eyes;
- in the evening a person experiences pain in the eyeballs;
- there is a feeling of pressure in the eyes from the inside.
Also, the eyes can be very itchy, the person begins to react sharply to light and prefers twilight. If treatment for glaucoma is not started, it will lead to complete loss of vision within 1-2 years. In the absence of stabilization of blood sugar levels, glaucoma develops 5 times faster - from the onset of the first symptoms to complete blindness, it can take only a few months.
Cataract
This disease is associated with clouding of the lens, and this occurs due to constant surges in blood sugar, with the accumulation of glucose in the structure of the lens, and this is what thickens it and makes it cloudy. Diabetic cataracts can be true or false, and can appear at any age and at any stage of the disease.
If the patient visited the doctor in a timely manner, underwent examination and a full course of treatment, then recovery will occur within 2-3 weeks of therapy. Particularly advanced cases lead to complete loss of vision.
Other causes of eye complications
Eye complications in diabetes are not always associated with high or unstable blood sugar levels; visual impairment can be caused by:
- multiple sclerosis;
- some systemic diseases (lupus);
- persistently low blood pressure;
- inflammatory and infectious diseases of the organs of vision;
- eye injuries;
- long-term use of certain medications.
If a person with diabetes notices a decrease in visual acuity, then there is no need to panic; this does not always mean the development of retinopathy, glaucoma or cataracts.
Diabetic retinopathy
The retina of the eye is a whole complex of specialized cells that perform a very important function. They are the ones who turn the light passing through the lens into a picture. Next, the optical nerve is activated, which transmits visual information to the brain.
When the blood circulation of the eye organs is impaired, they begin to receive less nutrients, which is why there is a gradual decline in the functions of the retina and optic nerve, as a result of which diabetic retinopathy begins to develop.
In this case, a decrease in visual acuity occurs as a result of increased intraocular pressure, damage to capillaries and nerve endings. This condition in medicine is referred to as microangiopathy, which also occurs with kidney pathologies. In the case when the disease affects large vessels, then we are talking about macroangiopathy, which also includes such pathological conditions as myocardial infarction and stroke.
Diabetes and vision: symptoms of the onset of the process
Symptoms of visual impairment may be subtle, literally barely noticeable, but if you have a history of diabetes mellitus, they should definitely alert you:
- periodic appearance of spots, circles of light, “flies” before the eyes;
- blurred image;
- tingling in the eyes, a feeling of “sand” against the background of a lack of general fatigue and drowsiness;
- severe dry eyes;
- decreased visual acuity.
Diagnostics
Diagnosing vision problems in diabetes mellitus is difficult because the symptoms of the pathologies are identical and sometimes are not at all related to a specific disease. Therefore, the ophthalmologist will refer such a patient to examine the fundus with special instruments, which will help:
- assess the level of transparency of the lens;
- determine the degree of detachment or “wrinkling” of the retina;
- identify the beginning of destruction of the blood vessels of the organs of vision.
The doctor will clarify the diagnosis and determine the severity of the disease, which will help determine treatment prescriptions: for some, nutritional correction and constant monitoring of sugar levels will help, but many patients will need to be treated with specific medications after the first visit to the ophthalmologist.
Loss of vision due to diabetes: how to restore it with surgery
Laser coagulation of the retina
The operation is prescribed for diabetes mellitus only in case of critical vision loss, when it cannot be restored with medications. Surgical interventions are justified for glaucoma, cataracts and retinopathy.
Laser coagulation of the retina is considered the most popular and effective - the formation of pathological blood vessels (new ones as compensation) stops, sometimes complete removal of the vitreous is required. If the operation is performed when the lens is completely clouded (complex cataract), then it is completely removed, and vision is restored by installing an intraocular lens.
Any surgical interventions are carried out using laser technologies, which involve reducing the risk of complications/side effects to a minimum, the absence of a recovery period and long hospitalization.
Vision correction for diabetes
If vision in diabetes begins to steadily decline, then measures will need to be taken to correct it:
- Visit an ophthalmologist twice a year for follow-up examinations. This will allow timely detection of critical changes in the eyeball and prevent complete blindness.
- Follow all the instructions of the treating endocrinologist exactly - take medications, perform insulin injections. This will help maintain blood sugar levels within normal limits at all times, which will reduce the likelihood of rapid progression of cataracts, glaucoma and retinopathy.
- If necessary, wear corrective glasses at all times. Regarding the advisability of using contact lenses, you should consult with specialists; often diabetes mellitus becomes a contraindication to this type of visual acuity correction.
- Follow the rules of rest and wakefulness/work during the day. If the patient is forced to spend a lot of time at the computer or reading papers (specifics of work activity), then he must break away from the usual “picture” every hour, look out at the window, and blink frequently.
According to statistics, those patients with diabetes who closely monitor the condition of their visual organs and follow all the recommendations of doctors reduce the risk of complete blindness significantly.
Cataract
As a result of all the processes described above, cataracts begin to develop, which is characterized by darkening of the lens, when in a normal state it has a transparent appearance. When the lens darkens, the ability to focus a picture and distinguish objects decreases, resulting in a person almost completely losing his vision.
It should be noted that in diabetics, cataracts are detected much more often than in healthy people, and it manifests itself with such symptoms as blurred images and featureless vision. Cataracts are not treated with medication because they do not produce any results. To restore vision, surgery is required to replace the poor lens with an implant. But even after this, the patient will have to constantly wear either glasses or contact lenses.
Often, with complicated retinopathy in diabetics, ocular hemorrhage is detected. The anterior chamber of the eye fills with blood, which entails an increase in the load on the eye organs and a sharp decrease in vision over several days. If the hemorrhage is severe and the entire posterior chamber of the eye is filled with blood, you should immediately consult a doctor, as there is a high risk of complete loss of vision.
Vision in type 2 diabetes: treatment with drops
If type 2 diabetes is diagnosed, then for vision problems, eye drops are prescribed that can stop the development of glaucoma, retinopathy or cataracts. Prescriptions depend on what kind of ophthalmological disease will be diagnosed by the doctor:
- Fotin, Timolol and Betaxolol - will help with glaucoma;
- Katachrom, Katalin and Taufon - will be effective only for cataracts;
- Vitafacol, Quinax and Riboflavin are prescribed for retinopathy.
Typically, eye drops for diabetes are administered into each eye, 2-3 drops twice a day. The duration of treatment is usually 2 weeks, but sometimes therapy can last for one and a half to two months.
Vision decreases with diabetes: what to do, what vitamins to take
If vision loss has begun due to diabetes mellitus, then you need to take vitamin supplements on a daily basis, possibly simultaneously with eye drop therapy. The fact is that such an endocrinological disease provokes metabolic disorders, the body does not receive micro/macroelements in sufficient quantities, and the result will be oxygen starvation, slowing down the functionality of all organs and systems, including the eyes.
It is believed that diabetics with diagnosed ophthalmic diseases should take:
- ascorbic acid – strengthens the general immune system, makes the walls of blood vessels more elastic;
- B vitamins – stabilize blood sugar levels, normalize the functioning of the central nervous system;
- retinol – increases visual acuity, improves the functioning of the eyeballs in the dark;
- tocopherol – “works” as a strengthening agent for blood vessels, ensures rapid removal of glucose breakdown products from the body;
- Vitamin P – helps to dilate blood vessels and improve circulation in them.
Diabetics should also take vitamin complexes, which are also available in the form of drops. For example, at the initial stage of diabetic retinopathy, Prenacid or Quinax drops are prescribed. Dietary supplements such as Blueberry-Forte and Selenium-Active practically do not work, but if diabetes mellitus has just been diagnosed, then they can be recommended as a preventive measure for the early onset of vision problems.
Diabetic retinopathy
Diabetic retinopathy is a common eye complication in diabetes mellitus, characterized by damage to the retinal vessels. The likelihood of developing such a pathological condition increases with the course of hyperglycemia. The longer a person is sick, the higher the risk of irreversible retinal changes and vision loss. And if the patient additionally suffers from anemia, hyperlipidemia or obesity, then the rate of progression of diabetic retinopathy increases significantly.
You can suspect the presence of eye diabetes based on the following symptoms:
- blurred vision;
- flickering of “flies” and dark spots before the eyes;
- a veil covering the eyes;
- poor visibility up close.
The severity of symptoms and treatment depend on the stage of the disease. At the initial stage of hyperglycemia, visual impairment is minor; to restore it, it is enough to change your lifestyle, follow a diet and control your sugar levels. In more complex cases, conservative or surgical treatment is prescribed. Laser coagulation is often used for treatment.