Reasons: why does accommodation spasm occur?
The main causes of accommodation spasm are excessive or improperly organized visual stress, lack of lighting, severe eye fatigue (long-term work at the computer, reading, working with optical instruments and small parts at close range).
Among the secondary reasons are malnutrition, vitamin deficiencies, disturbances in sleep and wakefulness, lack of physical activity necessary to maintain health, weakness of the back and neck muscles, the consequence of which is incorrect posture, leading to insufficient blood supply to the brain and visual system.
Causes of accommodation spasm (false myopia) in children
Children of preschool and primary school age are at risk of developing a spasm of accommodation more than others. This is due to the fact that the child’s visual system is being restructured at this time and is in a phase of active development.
The main causes of accommodation spasm in schoolchildren:
- excessive visual stress (TV, computer, tablet, phone);
- doing homework in the evening and at night;
- poor workplace lighting;
- non-compliance with the daily routine (lack of walks in the fresh air, exercise, lack of sleep);
- the desk and chair do not match the child’s height;
- failure to maintain the optimal distance to the book (30–35 cm);
- weakness of the neck and back muscles;
- impaired blood supply to the cervical spine;
- poor nutrition, hypovitaminosis;
- insufficient physical activity.
Loss of the ability to accommodate with age
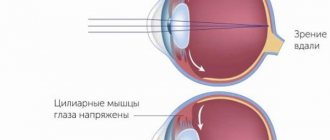
One of the conditions for normal accommodation is the elasticity of the lens . With age, it decreases, the lens becomes denser and harder.
The lens has the best accommodative properties in childhood. Then, due to the aging process and changes in the biochemistry of the body, the ability to see well up close gradually decreases (usually after 40–45 years), and presbyopia develops - age-related farsightedness. This is a natural and irreversible process; vision can be restored in the case of developing presbyopia only with the help of optical correction, implantation of a phakic lens, or replacement of the lens with an intraocular lens.
results
The results of studying the wavefront parameters without correction and with contact correction of the eye before and after cycloplegia are presented in Table. 1.
The total level of aberrations (RMS) increased with cycloplegia. In myopia, this increase was significant without correction (from 0.36±0.05 to 0.6±0.05 µm, p
<0.05), with hypermetropia - in the CL (from 0.34±0.01 to 0.57±0.01 µm,
p
<0.05).
For both myopia and hypermetropia, there was a statistically insignificant tendency towards an increase in RMS in the CL compared with the uncorrected state. No significant differences in wavefront changes were found in the types of SCLs we studied. Putting on K.L. caused significant changes in the following Zernike polynomials. With myopia, vertical coma (Coma 7) decreased from 0.04±0.01 µm without correction to 0.001±0.001 µm in the CL ( p
<0.05 in non-cycloplegic conditions) and horizontal coma (Coma with (–)0.01)
with (–)0.01)
±0.01 to 0.01±0.01 µm ( p
<0.05 under cycloplegia).Horizontal trefoil (Tref.9) increased from (–)0.01±0.01 to 0.01±0.005 µm (
p
<0.05) with a narrow pupil and from (–)0.01±0.01 to (–)0.1±0.005 μm (
p
<0.05) under cycloplegia. The positive SA present before correction changed to negative in all types of SCL: from 0.01±0.003 to (–)0.04±0.01 µm (
p
<0.05) with narrow and from 0.03±0.02 to (–)0.03 ±0.01 µm (
p
<0.05) with a wide pupil.
With hyperopia, the vertical trefoil decreased in absolute values (Tref.6): from (–)0.06±0.01 to (–)0.01±0.01 µm to cycloplegia ( p
<0.05) and from (–)0.04±0.01 to 0.01±0.01 µm under cycloplegia;
in the latter case - with a transition to the positive range. Coma 7 passed from positive to negative values: without cycloplegia from 0.01±0.001 to (–)0.02±0.01 μm ( p
<0.05), and under cycloplegia from 0.04±0.01 to ( –)0.04±0.01 µm (
p
<0.05). Coma 8 under non-cycloplegic conditions acquired negative values, changing from 0.001±0.001 to (–)0.03±0.01 µm, and under cycloplegia it did not change (–)0.02±0.002 and (–)0.02±0.003 µm respectively. SA, as with myopia, became negative, changing from 0.06±0.002 to (–)0.02±0.001 µm without cycloplegia and from 0.08±0.003 to (–)0.01±0.01 µm under cycloplegia .
Thus, SCLs changed the wavefront differently in myopia and hypermetropia. In myopic eyes, vertical coma decreased, horizontal coma increased (only under cycloplegia) with a transition to positive values, and horizontal trefoil increased. In hypermetropic eyes, the vertical trefoil decreased (in absolute values), changing sign to (+) under cycloplegia, the vertical coma decreased more significantly and turned into negative values (both in natural conditions and during paralysis of accommodation), the horizontal coma turned into negative values coma. Only SA in the SCL underwent the same changes in myopia and hypermetropia both in natural and in cycloplegic conditions, namely, it turned from positive to negative. This fact seems to us to be especially important, since it is known that negative SA stimulates the work of accommodation [16, 17]. We checked the state of accommodation under conditions of spectacle and contact correction in children and young people with myopia and hypermetropia. The results of the study are presented in table. 2.
Table 2. Accommodation parameters and pseudoaccommodation in glasses and contact lenses Table 2 (end) Note. * — p<0.05 between spectacle and contact correction; ** — p<0.05 between the indicators of the myopia and hypermetropia groups.
As follows from the table. 2, accommodation parameters (BAO, MAO, ZOA) were higher with hypermetropia than with myopia, both in glasses and in K.L. The only exception was the ZOA indicators in the CL, which turned out to be equally high in myopia and hypermetropia - (–)2.8±0.11 and (–)2.89±0.2, respectively. On the contrary, the PA value both in glasses and in CL was significantly higher in myopia than in hyperopia - 0.9±0.1 versus 0.6±0.08 diopters and 1.24±0.05 versus 0.78± 0.09 D, respectively ( p
<0,05).
A comparison of accommodation parameters depending on the correction method showed the following. In myopia, all indicators of accommodation (BAO, MAO, ZOA) and PA were significantly higher in CL than with spectacle correction. At the same time, the value of the objective accommodative response and accommodation reserves in the lenses approached the norm: BAO was (–)2.28±0.04 diopters with the norm being (–)2.5—(–)3.0 diopters, MAO was (–) 2.29±0.05 diopters with the same norm for a distance of 33 cm, ZOA - (–)2.8±0.11 diopters with the norm of 3.0-4.0 diopters for this age. The value of P.A. also turned out to be higher in CL than in glasses - 1.24±0.05 and 0.9±0.1 diopters, respectively ( p
<0,05).
With hypermetropia, the objective accommodative response was also significantly higher in CL than in glasses: MAO was (–)3.11±0.06 and (–)2.43±0.08 D, BAO — (–)2.95± 0.06 and (–)2.56±0.07 diopters, respectively. In both cases, the accommodative response corresponded to the norm. The subjective indicator of the POA did not differ significantly in different correction conditions and also corresponded to the norm. The value of P.A. tended to increase in CL, but the difference was not significant.
The results of our studies showed that high accommodative ability was recorded simultaneously when putting on contact lenses, compared with spectacle correction, and is obviously associated with the optimization of the conditions of visual activity created by the lenses.
Thus, contact correction, compared to spectacle correction, increases the accommodative ability, as well as the magnitude of PA (i.e., the ability to visually work near without the participation of accommodation itself). Both effects create better conditions for increasing visual performance. The identified differences can obviously be associated with changes in the wavefront parameters in the CL: induced negative SA promotes increased accommodation [16, 17], and an increase in the total level of aberration provides relief from PA [6].
The tendency we discovered towards an increase in RMS in CL is consistent with the data of F. Lu (2003), B. Roberts et al. (2006), R. Gatti (2008), who showed that SCLs when correcting myopia increase the total aberrations of the wavefront [18-20]. At the same time, some authors found a direct correlation of total (RMS) aberrations with a lag in the accommodative response: a high level of aberrations increases the depth of focus, which reduces sensitivity to image defocusing and reduces the accommodative response [1, 6]. However, in contrast to the cited works, in our study the increase in RMS was insignificant and unreliable. Obviously, this should explain the increase, and not the decrease, in accommodation indicators that we identified in lenses compared to glasses. J. He et al did not find a connection between the SA level and accommodation indicators; B. Roberts et al noted an increase in SA in the CL. S. Awward (2008) and co-authors showed that SCLs with a power of (–)2.0 D significantly increase SA, and SCLs with a power of (–)6.0 D reduce it [6, 19, 21]. A decrease in SA in 6 types of CL was also noted by R. Gatti (2008). In our study, the average degree of myopia was (–)5.6 diopters; however, in addition to this coincidence, in case of hypermetropia, CLs reduced positive SA and, on average, induced a negative one.
Decentration of the CL relative to the center of the pupil can increase HOA. A number of studies have noted an increase in coma and trefoil in the CL [19–21]. Our results showed a significant decrease in vertical coma and a less pronounced increase in horizontal coma - only in myopia. The study revealed a positive correlation between vertical coma (Z7) and the volume of accommodation, which is not consistent with our data and requires further study [22]. The connection between trefoil and accommodation has also not been studied. In our work, the vertical trefoil in the CL increased only with hypermetropia, and the horizontal trefoil increased with myopia.
Accommodation indicators
The accommodative ability of the eye is expressed in diopters or linear values.
Accommodation indicators obtained from examining each eye separately are called absolute. And both at once are relative, since they are performed with a certain convergence (reduction) of the visual axes.
- The area of accommodation is the distance between the farthest (distance vision) and the nearest (near vision) points of clear vision.
- The volume of accommodation is the difference in the refractive index of the eye (in diopters) when set to the nearest and farthest points of clear vision.
- The accommodation reserve is the unused part of the accommodation volume (in diopters) when the eye is placed at the fixation point.
Volume of relative accommodation
The volume of relative accommodation is the accommodation associated with convergence and performed binocularly when fixating a common object. It is made up of negative and positive parts.
Age norms of accommodation. * - POA results greater than 5 always turn out to be overestimated in myopia and in the case of dissociation between accommodation and convergence.
Relative accommodation reserve
The margin of relative accommodation (ROA) is the positive part of the volume of relative accommodation. To determine in clinical practice, use a text corresponding to a visual acuity of 0.7 tables for near at a distance of 33 cm. Binocularly, under conditions of full correction for distance, the correction is increased in steps of 0.25 - 0.5 diopters as long as the patient reads the text. The difference between the corrective and the found lens is the margin of relative accommodation.
Spent part of relative accommodation
The expended part of relative accommodation is the negative part of the volume of relative accommodation. For determination in clinical practice, a text corresponding to a visual acuity of 0.7 of the table for near at a distance of 33 cm is used. Binocularly, under conditions of full correction for distance, the correction is weakened in steps of 0.25 - 0.5 diopters until the patient reads the text. The difference between the correcting and the found lens is the expended part of the relative accommodation.
Forms of accommodation disturbance:
- spasm of accommodation;
- asthenopia;
- paralysis of accommodation;
- age-related weakening of accommodation (presbyopia).
Accommodative asthenopia
In other words, this is chronic fatigue of the muscles responsible for accommodation. Most often, the pathology develops in people with farsightedness, astigmatism, or in the absence or incorrectly selected glasses correction.
Patients complain of rapid eye fatigue when reading, blurred book text, redness of the eyes and edges of the eyelids, burning sensation, itching, foreign body sensation, headache, episodes of nausea and vomiting.
The main cause of accommodative asthenopia is excessive strain of accommodation near, while its reserves are limited. Treatment of pathology is optimal spectacle or contact correction.
Paralysis and paresis of accommodation
As a rule, these conditions are neurogenic in nature or occur as a result of injury or poisoning. In people with normal visual acuity and farsighted people, near vision deteriorates. In myopic people, visual acuity does not drop so sharply, and sometimes does not change at all. With paralysis, the volume of accommodation is reduced and its reserves are lost.
Age-related weakening of accommodation (presbyopia)
A physiological phenomenon that is associated with age-related changes in the lens, its hardening and gradual loss of elasticity. Treatment is the selection of optimal correction for near vision in accordance with age and initial refraction.
Possible violations
In some cases, vision problems are genetically transmitted diseases. Negative changes in the condition of the eye muscles also occur during the aging process, due to overstrain of the visual organs and due to fatigue of the human body as a whole. In this case, the following violations are observed:
- Paralysis - focus is only possible on a distant object.
- Spasm - the eye adapts poorly or not at all to focus on an object located at a great distance. The disease is called “false myopia.”
- Presbyopia is caused by age (aging of the lens).
- Excessive tension is the result of prolonged violation of visual hygiene rules.
- Asthenopia is a problem with functioning caused by another eye disease (farsightedness).
Sometimes, for preventive purposes, in order to identify emerging eye diseases, it is also worth performing skiascopy and computer perimetry of the eye.