Anatomical structure
The lacrimal apparatus of the eyeball is a complex system of organs through which tears and tear fluid are secreted and drained.
This section contains a gland that produces fluid. The glandular tissue constantly works, due to which the surface of the eyes is constantly lubricated. Human lacrimal glands are twin organs, the size of which reaches twenty millimeters, and their shape is very similar to an almond. They consist of palpebral (smaller) and orbital (larger) parts. The first runs along the eyelid, on its inner side. It can be detected by palpation or seen if you turn out the upper eyelid.
The second is hidden in a depression in the frontal bone, which is called the fossa of the lacrimal gland. The separation into parts is not complete; connective tissue runs behind, which is a kind of bridge between them.
| The anatomy of the lacrimal gland is complex primarily due to the fact that the structure of the organ is multi-stage. It consists of several dozen lobules separated by connective tissue. They also contain lobules composed of epithelial cells. |
The structure of each lobe is influenced by the features of its anatomical location. So, since the orbital part is located inside the bone, its elements are closely pressed to each other. But the lower one has a slightly different structure - the lobules are located at a short distance.
Regardless of location, all parts are equipped with blood vessels and excretory ducts, as well as a network of nerves. Blood flows to the gland constantly. Innervations of both types (both circulatory and reflex) are designed in such a way that the life support of the eye does not stop if the stable operation of the main system is interrupted or disrupted. The large excretory ducts that form in the upper part transform into smaller ones in the lower part. And through them, the secretory fluid is released out.
Plastic punctum
Plastic surgery of the lacrimal punctum is a surgical operation performed by excision of the inner edge of the lacrimal punctum and plastic surgery of the eyelid in order to eliminate pathologies of the lacrimal duct of the eye due to congenital developmental anomalies or injuries.
The content of the article:
- The course of plastic surgery of the lacrimal punctum
There are a number of pathologies of the lacrimal punctum of the eye that require surgical correction of this area. These include:
- absence of lacrimal opening;
- underdevelopment of the lacrimal opening;
- narrowing of the lacrimal opening;
- dislocation of the lacrimal opening;
- dry eye syndrome;
- pathology of the lacrimal ducts as a result of frequent damage to the conjunctiva by infectious diseases.
The above pathologies can be either congenital or acquired.
The absence of the lacrimal punctum is defined by the term “aplasia”, underdevelopment - “hypoplasia”, narrowing - “stenosis”. Both the lacrimal openings of each eye and one can be affected. In this case, the patient suffers from constant lacrimation and accumulation of tear fluid in the corner of the eye. However, with the normal state of the second lacrimal punctum and its optimal functioning, problems associated with pathologies of the first lacrimal punctum may not appear, which means that the operation will not be urgent.
Eversion of the lacrimal opening is also an indication for surgical intervention. It is this pathology that is the most common among those acquired, less common as a congenital abnormality. The state of the lacrimal punctum can be called normal when it is facing the eyeball and hidden by the lower eyelid. When everted, it is noticeable even without retracting the lower eyelid. Discomfort in this case is due to constant lacrimation. Like others, this anomaly can only be corrected surgically.
It is worth noting that plastic surgery of the lacrimal punctum can be carried out only after the formation of the lacrimal ducts, nasolacrimal duct, skull bones, and nasal cartilage has been completed. As a rule, this operation becomes possible once the patient reaches 14 years of age. Individual cases are determined by a specialist.
Plastic surgery of the lacrimal punctum of the eye is one of the operations of high complexity.
Initially, it is worth considering the structure of the lacrimal ducts of the eye. They consist of the lacrimal canaliculi, lacrimal sac and nasolacrimal duct. Tears are discharged into the nasal cavity using the nasolacrimal duct, into which the lacrimal sac passes into its lower part. Various pathologies of the lacrimal opening require their own algorithm for performing the operation. For example, when the lacrimal punctum is underdeveloped (atresia), the film covering it is pierced or cut crosswise. Thus, the specialist restores patency, then within two days the point must be bougienage.
With aplasia, the point must be formed and then connected to the lacrimal canaliculi.
Stenosis of the lacrimal opening is often accompanied by inflammation in this area, which is chronic in nature. Since in this case the operation is significantly complicated, initial treatment is required - rinsing the nasolacrimal duct. If this is not possible, intubation is performed with a specialized tube, and then the operation itself can be performed.
In the case of dry eye syndrome, surgical intervention can be avoided: initially, the problem is usually eliminated with conservative treatment, and if the required result is not achieved, the specialist is forced to perform surgical intervention.
Dislocation of the lacrimal opening is corrected by several methods. Fazakas' operations for dislocation of the inferior lacrimal punctum suggest focusing on excision of the lacrimal papilla using various methods. Operations using the Nemeth method are used for anterior and posterior dislocation and involve the introduction of a thin conical probe into the lacrimal canaliculi.
Most plastic surgery clinics in Moscow offer lacrimal punctal plastic surgery. Detailed information about them, including contact details and price list, is available on our website.
Functions of the lacrimal gland
- Moisturizing the surface of the cornea
- Elimination of xerophthalmia, that is, dry eye syndrome resulting from fatigue and visual strain
- Delivery of nutrients to the cornea. In particular, lysozyme is an enzyme that destroys bacterial cells, and beta-lysine is a whey protein that has antimicrobial activity.
- Protection from the harmful effects of microorganisms
- Cleansing the surface of the eyeball from external contaminants, dust, and foreign objects
- Tears released in stressful situations or under the influence of emotions control the sudden release of hormones and help stabilize the mental state.
Tear film
| The tear film is a multicomponent substance distributed over the surface of the eyeball. It helps the substances released during the functioning of the gland to fully realize their functions. |
This means protection from exposure to atmospheric oxygen and from excessive drying out. When blinking, part of the secretion settles on the front convex side of the eyeball, while the water component of the flow mechanically cleanses the cornea.
The tear film has a complex structure and consists of three layers that never mix:
- Interior. Adjacent directly to the cornea. Its main component is the mucous substance mucin. Allows fluid to be distributed freely and evenly throughout the epithelium by reducing the surface tension of the film.
- Average. Formed by auxiliary small lacrimal glands, it has a liquid base. Is the thickest of all. Cleanses the surface of the eye and serves as a conductor for nutrients.
- Outer. Otherwise called lipid or oil, it consists of fats. Prevents the evaporation of the water layer, and also maintains the smoothness of the film and promotes its better distribution.
Eyeball
The eyeball itself is located in the orbit, and is surrounded on the outside by protective soft tissues (muscle fibers, fatty tissue, nerve pathways). In front, the eyeball is covered with eyelids and the conjunctival membrane, which protect the eye.
The apple has three shells that divide the space inside the eye into the anterior and posterior chambers, as well as the vitreous chamber. The latter is completely filled with vitreous humor.
Fibrous (outer) layer of the eye
The outer shell consists of fairly dense connective tissue fibers. In its anterior section, the shell is represented by the cornea, which has a transparent structure, and the rest of the shell is white in color and has an opaque consistency. Due to elasticity and elasticity, both of these shells create the shape of the eye.
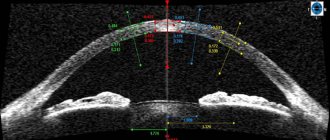
Cornea
The cornea makes up about a fifth of the fibrous membrane. It is transparent, and at the point of transition to the opaque sclera it forms a limbus. The shape of the cornea is usually an ellipse, the dimensions of which in diameter are 11 and 12 mm, respectively. The thickness of this transparent shell is 1 mm. Due to the fact that all the cells in this layer are strictly oriented in the optical direction, this shell is completely transparent to light rays. In addition, the absence of blood vessels in it also plays a role.
The layers of the cornea can be divided into five, similar in structure:
The cornea contains a large number of nerve receptors and endings, and therefore it is very sensitive to external influences. Due to the fact that it is transparent, the cornea allows light to pass through. However, at the same time, it refracts it, since it has enormous refractive power.
Sclera
The sclera refers to the opaque part of the outer fibrous membrane of the eye and has a white tint. The thickness of this layer is only 1 mm, but it is very strong and dense, as it consists of special fibers. A number of extraocular muscles are attached to it.
Choroid
The choroid is considered medium, and its composition mainly includes various vessels. It consists of three main components:
- The iris, which is located in front.
- Ciliary (ciliary) body, belonging to the middle layer.
- The choroid itself, which is the posterior part.
Iris
The shape of this layer resembles a circle, inside of which there is a hole called the pupil. It also contains two orbicularis muscles, which provide optimal pupil diameter in different lighting conditions. In addition, it contains pigment cells that determine eye color. If there is little pigment, then the eye color is blue, if there is a lot, then brown. The main function of the iris is to regulate the thickness of the light flux, which passes into the deeper layers of the eyeball.
The pupil is an opening inside the iris, the size of which is determined by the amount of light in the external environment. The brighter the lighting, the narrower the pupil, and vice versa. The average pupil diameter is about 3-4 mm.
Ciliary body
The ciliary body is the middle part. The choroid has a thickened structure, shaped like a circular ridge. This body includes the vascular part and the ciliary muscle itself.
In front of the vascular part there are 70 thin processes that are responsible for the production of intraocular fluid that fills the inside of the eyeball. From these processes extend the thinnest ligaments of Zinn, which are attached to the lens and suspend it inside the eye.
The ciliary muscle itself has three sections: external meridional, internal circular, and middle radial. Due to the location of the fibers, during relaxation and tension they directly take part in the process of accommodation.
Choroid
The choroid is represented by the posterior region of the choroid and consists of veins, arteries and capillaries. Its main task is to deliver nutrients to the retina, iris and ciliary body. Due to the large number of vessels, it has a red color and stains the fundus of the eye.
Retina
The reticular inner shell is the first section that belongs to the visual analyzer. It is in this shell that light waves are transformed into nerve impulses that distribute information to central structures. In the brain centers, the received impulses are processed and an image is created that is perceived by a person. The retina consists of six layers of different tissues.
The outer layer is pigmented. Due to the presence of pigment, it scatters light and absorbs it. The second layer consists of processes of retinal cells (cones and rods). These processes contain large amounts of rhodopsin (in rods) and iodopsin (in cones).
The most active part of the retina (optical) is visualized during fundus examination and is called the fundus. This area contains a large number of vessels, the optic disc, which corresponds to the exit of nerve fibers from the eye, and the macula. The latter is a special area of the retina in which the largest number of cones are located, which determine daytime color vision.
The apple has three shells that divide the space inside the eye into the anterior and posterior chambers, as well as the vitreous chamber.
Diseases of the lacrimal apparatus of the eye
Symptoms indicating damage to the eye organ can be very different. They manifest themselves as a sensation of a foreign body, sand in the eyes, as well as burning, dryness, or, on the contrary, the outflow of tear fluid may be impaired and excessive tearing will appear. Large secretions can occur at the lacrimal punctum, in the nasal cavity or at the border of the lower eyelid.
The lacrimal apparatus of the eye has 12 very thin ducts, which are located in the glandular tissue. With the help of ducts, fluid can enter the conjunctival sac through openings in the conjunctival vault in the area of the upper eyelid vault. When a person blinks, the tear fluid is evenly distributed over the entire surface of the eyeball, and then collects in the inner corner of the eye, in the tear lake.
The human organ of vision also includes the upper movable and lower fixed eyelids. On the inside there are small tubercles with small holes inside. In medicine they are called lacrimal puncta. Excessive amount of tear fluid penetrates the points and is drained through thin canaliculi - ducts.
In order for the produced secretion to be freely transmitted throughout the entire system, the lacrimal glands must communicate with each other. This communication is carried out using ducts, which are similar in structure to a network of branching tubes and pass from the upper gland through the eyelid, reaching the lower one. The number of output channels may vary, but most often there are twelve.
Ducts can be divided into subtypes:
- Located in the lobules of the gland itself (intralobular)
- They are located between the lobules and are a system of intermediaries between them (interlobular)
- They connect the glands and carry fluid throughout the body until they exit into the external environment (main excretory)
The lacrimal fluid secreted from the superior orbital gland is combined with the secretion of the lower part through the ducts. The tears then collect in the conjunctival sac under the upper eyelid and, after passing through the entire cornea of the eye, enter small holes in the inner surface of the eyelids, which are called lacrimal puncta.
Some of the liquid is retained there. It is thanks to it that hydration occurs when blinking. Next, passing the narrow area between the cornea and the lower eyelid (tear stream), flowing into the inner corner of the eye (tear lake).
From there to the upper part of the nasolacrimal canal (lacrimal sac), and from there the liquid is removed into the nasal cavity, where it evaporates, thereby providing hydration.
The blood supply follows the following scheme. The lacrimal artery emerges from the main ophthalmic artery. Its tubes unite with the main excretory ducts. Next, they are divided into tubules of smaller size and diameter, which, having reached the glandular lobules, branch into small capillaries.
They entangle all tissues in a network and gradually organize themselves into small blood vessels, and larger ones flow out of them. And then through the lacrimal vein, which passes in the same way as the artery, the outflow of blood follows into the ophthalmic vein. Both of them: both the vein and the artery are located on the posterior surface of the gland.
The gland receives innervation, that is, the presence in the tissues of conductive fibers that work to establish communication with the central nervous system, of three types:
- Afferent (sensitive). Provided by the lacrimal nerve, which leaves the eye
- Parasympathetic secretory. Originates in the facial ganglion, the nucleus of which causes lacrimation
- Sympathetic secretory. It is carried out by fibers of the main cervical ganglion.
Inner nucleus of the eye
In the cavity of the eyeball there are light-conducting (also known as light-refracting) media, which include: the lens, aqueous humor of the anterior and posterior chambers, as well as the vitreous body.
Aqueous moisture
The intraocular fluid is located in the anterior chamber of the eye, surrounded by the cornea and iris, as well as in the posterior chamber, formed by the iris and lens. These cavities communicate with each other through the pupil, so fluid can move freely between them. The composition of this moisture is similar to blood plasma; its main role is nutritional (for the cornea and lens).
Lens
The lens is an important organ of the optical system, which consists of a semi-solid substance and does not contain blood vessels. It is presented in the form of a biconvex lens, on the outside of which there is a capsule. Lens diameter 9-10 mm, thickness 3.6-5 mm.
The lens is located in the recess behind the iris on the anterior surface of the vitreous body. The stability of the position is ensured by fixation using the ligaments of Zinn. From the outside, the lens is washed by the intraocular fluid, which nourishes it with various useful substances. The main role of the lens is refractive. Due to this, it helps focus the rays directly on the retina.
Vitreous body
In the posterior part of the eye, the vitreous body is localized, which is a gelatinous transparent mass similar in consistency to a gel. The volume of this chamber is 4 ml. The main component of the gel is water, as well as hyaluronic acid (2%). In the area of the vitreous body, fluid constantly moves, which allows nutrition to be delivered to the cells. Among the functions of the vitreous body it is worth noting: refractive, nourishing (for the retina), as well as maintaining the shape and tone of the eyeball.
Pathologies of the lacrimal gland
Disorders of the lacrimal gland can be either acquired at birth or acquired during life. The first are associated with insufficient development or absence of one of the components of the lacrimal apparatus. The main cause of such anomalies is intrauterine trauma. These include:
- Insufficient development of the gland
- Lack of the required number of ducts
- Nasolacrimal duct blockage
- Displacement of lacrimal openings
- Excessive or, conversely, inadequate fluid production
Diagnosis of the disease
To diagnose diseases, an in-person examination by a specialist is necessary. When palpating the lacrimal sac, as a rule, painful sensations occur. It is possible to examine the required part of the lacrimal gland using a slit lamp; to do this, the upper eyelid should be everted. Eye microscopy will help assess the condition of the lacrimal openings, as well as the level of hydration of the conjunctiva and cornea. As a result of disturbances in the functioning of the lacrimal glands, tissue cells begin to die, which leads to atrophy of the organ.
In ophthalmology, several ailments associated with disturbances in the functioning of the lacrimal gland have been recorded.
- Dacryocystitis is an inflammatory process that occurs at the top of the nasolacrimal duct due to its obstruction
- Sjögren's syndrome is an autoimmune connective tissue disorder that occurs against the background of pronounced dysfunction of the secretory activity of the glands, and is a common cause of excessive dry eyes.
- Dacryoadenitis is an inflammation that affects the tissue of the lacrimal gland. It can be both acute and chronic. It does not often occur on its own; it is often a complication of various diseases.
- Canaliculitis – inflammation of the tear ducts caused by infection
- Mikulicz's disease - originates from a pathology of the immune system, causes swelling and an increase in the size of the lacrimal and salivary glands
Diagnostic methods
- Diseases of the lacrimal gland usually do not go away in isolation, since it is an obligatory and integral part of the lacrimal apparatus and affects the performance of the visual organs as a whole. Therefore, at the first suspicion of any pathological processes in the lacrimal gland, it is necessary to undergo special studies.
- Diagnosis of the level of secreted liquid secretion using the Schirmer test. A thin strip of filter paper is placed in the outer corner of the eye, and then the degree of saturation is assessed. A normal result is considered if the sample gets wet by 15 millimeters in five minutes.
- Tubular nasolacrimal test using dye. A colored substance (3% collargol solution) is instilled into the conjunctival cavity, and a cotton swab is placed in the lower nasal passage. A normal result is considered if within 5 minutes the dye is absorbed and comes out, which is confirmed by staining the tampon.
- Ultrasonography
- Bacteriological study of produced tear fluid
- Massage of the lacrimal canal in newborns: eye massage for obstruction of the lacrimal canal