What is it and how does it manifest itself?
Convergence is the process of bringing the visual axes of the eyes closer to the nose, with fixation on a located object. Physiologically, this act is justified by the simultaneous contraction of the internal muscles, which is accompanied by miosis and accommodation of the eyeballs. Convergence of the eyes is a reflex process of binocular vision. Characterized by disorders of the neuromuscular and sensory systems.
If binocular vision impairment is detected in a child in time, treatment can only be based on the use of special exercises.
Ocular convergence insufficiency occurs in every 5 children; most often it is not diagnosed, since a routine check by an ophthalmologist is not able to detect deviations. Sometimes children are mistakenly diagnosed with hyperactivity because they have difficulty concentrating while reading.
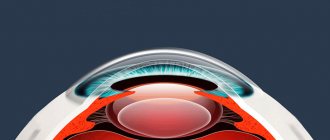
The structure of the human eye
People receive more than 80% of information thanks to what and how we see. The structure of the visual organ is very complex. It depends on the function of the eyes.
The human eyeball is an irregularly shaped sphere. It is located inside the orbits of the skull. From birth to death, the eye sockets double in size.
The optic nerve plays an important role. It transmits information to the occipital cortex, then analyzed.
The lacrimal gland keeps the surface of the eye moist. Tears lubricate the conjunctiva well.
In the structure of the human eye, the muscles of the eyeball act in concert with each other. The eyelids cover the eye, protecting it from negative factors. Eyelashes perform a similar function.
Reasons for violations
The most common factor in the occurrence of disorders of conjugate movements of the eyeballs are problems with the central nervous system, since the process of pupil activity is regulated by the centers of the cerebral cortex, midbrain, pons and cerebellum. In adulthood, the cause of convergence is a previous stroke or problems with the motor roots of the nerve endings.
- Bridge One-sided violation. Horizontal paresis towards the affected side.
- Bilateral damage. Movement of the eyeballs is allowed only in the vertical plane.
- Paresis of upward gaze and poor reaction of the pupils to light. The cause of the condition is hydrocephalus and pinealoma in people under 45 years of age, and stroke in older people.
- The parallelism of the visual axes is disrupted, and strabismus occurs in the vertical plane. Characterized by the presence of oculomotor disorders.
Return to contents
Diagnostic methods
Testing oculomotor functions:
- study of the range of ocular movements in various directions;
- pupil stabilization;
- saccade;
- progressive sliding movements of the pupils;
- the ability to bring your eyes to your nose;
- Diagnosis of strabismus using a closed eye test.
Study of oculomotor reflexes:
- "doll's eye" test;
- presence of Bell's sign (turning the eye upward when closing it).
Return to contents
Treatment of Convergence Disorders
If there is no convergence of the eyes, a therapeutic exercise should be performed daily:
- Place a pencil at a distance of 30 cm and look past it. In this case, two images of the object should be seen.
- First you need to look at the image of the “right” pencil so that the “left” one is also visible, then turn your gaze to the “left” one without losing sight of the other one.
- Continue to do this fixation, first at a slow, then at an accelerating pace.
To enhance convergence, exercises are used that are done daily. They can alternate during the day.
Exercise 1. Place the pencil vertically 20 cm from the eyes, look far away for 20 seconds, fixing your attention on the double images of the object, then move your gaze to the pencil and look at it for 5 seconds, then look into the distance again and repeat the actions.
Exercise 2. Place the pencil vertically at arm's length, slowly bring it closer to your eyes until double vision occurs, and then slowly move it away from you.
Exercise 3 is used for volitional convergence. Stand facing the window so that the horizon is visible. By an effort of will, bring your eyes to the bridge of your nose, holding in this position for 7 seconds, then look into the distance and bring your eyes back again.
Treatment of pathology
For poor vision associated with convergence insufficiency, therapeutic training is recommended every day, which consists of the following exercises:
- Place the pen at a distance of 30 cm from the eyes and direct your gaze past it. A person should see 2 images.
- It is necessary to look at the outline of the handle on the left, while not losing sight of the right one. Turning your gaze to the right, repeat in the other direction.
- At the beginning of the training, do the fixation slowly, then speed up the pace.
Exercises used to increase the ability to evenly bring the eyes to the nose are carried out regularly 1-2 times a day. Training the eye muscles comes down to monotonous repetition of the same movements in order to stabilize vision. With the progressive development of strabismus, surgical intervention is indicated. Doctors surgically fix the extraocular muscles and stabilize the position of the pupils.
The role of ocular convergence
Convergence of the eyes plays an important role in binocular vision during the combination of monocular visual images, creating the necessary conditions for their fusion. In children it is often disrupted.
Convergence disorders often lead to the appearance and intensification of myopia and the development of axial myopia. The phenomenon is serious and undesirable, especially for children and their parents. To do this, eye convergence must be diagnosed. How to check?
- An adult needs to make the child face him and close one eye.
- Approximately in the middle of the distance, place the pencil vertically so that an adult with an open eye sees it superimposed on half of the child’s face, and the upper end is located at the level of his eyes.
- Invite the child to look into the open eye of an adult and find out how many pencils he sees.
- If the child sees “one” pencil, the process is completed. His binocular vision is impaired.
- If there are “two” pencils, he needs to look only at the top of the object, which should be slowly brought closer to the child’s face.
- If there is no convergence, as the pencil gets closer to the child’s face, one eye tends more towards the nose, the other towards the temple.
- If convergence is present, the child's eyes turn symmetrically towards the nose until the distance decreases to 5 cm.
- Then ask the child to look at the pencil for 1-1.5 minutes. If the convergence of the eyes is stable, they should be equally turned towards the nose.
- Invite your child to focus both eyes toward his nose without a pencil. If this works, then he has “volitional convergence.”
Convergence of the eyes: causes of disorders and treatment
In the case of diagnosis of diseases such as tumors, brain gliomas, strokes and some others, disorders associated with the eyes often appear - voluntary movements, strabismus. In cases where the nerve is affected, most often only one eye is affected, or changes are observed in both, but to varying degrees.
Damage to the central nervous system leads to oculomotor disorders such as vertical and horizontal gaze paresis, various forms of nystagmus, vertical strabismus, and ocular dysmetria. All these pathologies relate to oculomotor disorders.
Conjugate eye movement disorders
Friendly eye movements are determined by the central zones of the cerebral cortex, the cerebellum, and the midbrain. Such pathologies are diagnosed quite often when it comes to lesions of the central nervous system.
Horizontal gaze paresis occurs when one side of the pons is affected and the reticular formation is involved. If a lesion is diagnosed on both sides, then we will be talking about a complete form of horizontal paresis, and the eyes will be able to move exclusively within the vertical plane. Sometimes, if the lesion is relatively weak, only partial horizontal gaze paresis is observed or nystagmus is diagnosed. As a rule, the patient is also concerned about some other neurological signs. Moreover, the upper part of the brain stem, as well as the cerebral cortex, can lead to the manifestation of horizontal gaze paresis. Often, the so-called vestibulo-ocular reflexes that occur during such processes are virtually impossible to change.
The midbrain has the function of regulating eye movement in the vertical direction. When it comes to damage to the roof of the midbrain, upward gaze paresis is likely to occur over time. In some cases, this disease is accompanied by a weakening of the reaction of the pupils to light, but a sufficient reaction of accommodation is preserved. Young people most often suffer from such diseases as a result of hydrocephalus, and older people - due to a stroke. Downward gaze paresis is not diagnosed so often and can manifest as an acute form, for example, after a stroke, or develop gradually, which quite often manifests itself as a consequence of Parkinson’s disease, or some other diseases of the central nervous system.
If the site of the lesion is localized in the midbrain, then a change in the parallelism of the visual axes in the vertical plane is possible. This pathology is also called vertical strabismus. This disease is actually no different from trochlear nerve palsy, but some individual signs are also noted. For example, symptoms of a focal neurological nature, as well as oculomotor disorders, are noted.
NEWS LIBRARY SITE MAP LINKS ABOUT THE SITE16.5.4. Mammal eye
The mammalian eye is a sensory organ consisting of a large number of receptor cells (rods and cones of the retina), sensory neurons that form the optic nerve, and a complex system of auxiliary devices. This device allows the eye to perceive light of different wavelengths reflected by objects in the field of view at different distances, and convert it into electrical impulses that are sent to the brain and generate amazingly accurate perceptions.
Light travels in the form of waves of electromagnetic radiation, and the waves perceived by the human eye make up a narrow, so-called visible part of the spectrum
(wavelengths 380-760 nm; see Appendix 1.7).
Light is a type of energy; it is emitted and absorbed in discrete portions - quanta
, or
photons
. Each quantum in the visible part of the spectrum carries energy sufficient to cause a photochemical reaction in the sensitive cells of the eye. The operation of the eye is based on the same principles listed below as the camera, namely it 1) controls the amount of light passing inside; 2) focuses images of objects in the external world using a lens system; 3) registers the image on the sensitive surface; 4) processes an invisible image into an internal image of a visible picture of the world.
Structure and function of the human eye
The eyes are located in hollows of the skull called orbits
;
the eye is strengthened here with the help of four rectus
and two
oblique
muscles that control its movements.
The human eyeball has a diameter of about 24 mm and weighs 6-8 g. Most of the eye is made up of auxiliary structures, the purpose of which is to project the field of view onto the retina
- a layer of photoreceptor cells lining the inside of the eyeball.
The wall of the eye consists of three concentric layers: 1) sclera (albuginea) and cornea; 2) choroid, ciliary body, lens and iris; 3) retina. The shape of the eye is maintained by hydrostatic pressure (25 mmHg) of the aqueous humor and vitreous humor. A diagram of the structure of the human eye is shown in Fig. 16.33. Below is a brief listing of its various parts and the functions they perform.
Rice. 16.33. Structure of a mammal's eye
Sclera
- the outermost layer of the eye. This is a very dense capsule containing collagen fibers; protects the eye from damage and helps the eyeball maintain its shape.
Cornea
- transparent anterior side of the sclera. Thanks to the curved surface, it acts as the main light-refracting structure.
Conjunctiva
- a thin transparent layer of cells that protects the cornea and extends into the epithelium of the eyelids. The conjunctiva does not extend into the area of the cornea that covers the iris.
Eyelid
- protects the cornea from mechanical and chemical damage, and the retina from too bright light.
Choroid
- middle shell; penetrated by vessels supplying blood to the retina, and covered with pigment cells that prevent the reflection of light from the inner surfaces of the eye.
Ciliary (ciliary) body
- the junction of the sclera and cornea. Consists of epithelial cells, blood vessels and ciliary muscle. The ciliary muscle is a ring consisting of smooth muscle fibers, circular and radial, which change the shape of the lens during accommodation.
Ciliary (cinnamon) ligament
- attaches the lens to the ciliary body.
Lens
- transparent elastic biconvex formation. Provides fine focusing of light rays on the retina and separates the chambers filled with aqueous humor and vitreous humor.
Aqueous moisture
- a transparent liquid representing a solution of salts. It is secreted by the ciliary body and passes from the eye into the blood through Schlemm's canal.
Iris
- annular muscular diaphragm, contains pigment that determines eye color. Divides the space filled with aqueous humor into the anterior and posterior chambers and regulates the amount of light entering the eye.
Pupil
- a hole in the iris through which light passes into the eye.
Vitreous body
- a transparent semi-liquid substance that maintains the shape of the eye.
Retina
- the inner membrane containing photoreceptor cells (rods and cones), as well as the bodies and axons of neurons that form the optic nerve.
Fossa fovea
- the most sensitive part of the retina, containing only cones. In this area, the light rays are most accurately focused.
Optic nerve
- a bundle of nerve fibers that conduct impulses from the retina to the brain.
Blind spot
- the place on the retina where the optic nerve exits the eye; it contains neither rods nor cones and therefore has no light sensitivity.
16.8. List in order the structures through which light passes on its way to the retina.
Accommodation
Accommodation is a reflex mechanism by which light rays emanating from an object are focused on the retina. It includes two processes, each of which will be discussed separately.
Reflex change in pupil diameter.
In bright light, the circular muscles of the iris contract, and the radial muscles relax; as a result, the pupil constricts and the amount of light falling on the retina decreases, which prevents damage to it (Fig. 16.34). In dim light, on the contrary, the radial muscles contract and the circular muscles relax. An additional benefit of constricting the pupil is that the depth of field is increased, so that differences in the distance from the subject to the eye have less impact on the image.
Rice. 16.34. Reaction of the iris (and thus the pupil) to changes in light
Refraction (refraction) of light.
From an object more than 6 m away, almost parallel rays of light enter the eye, while rays coming from closer objects diverge noticeably.
In both cases, for light to be focused on the retina, it must be refracted
(that is, its path is curved), and for close objects the refraction must be stronger. The normal eye is able to accurately focus light from objects at a distance of 25 cm to infinity. Refraction of light occurs when it passes from one medium to another, which has a different refractive index, in particular at the air-cornea interface and at the surfaces of the lens. The shape of the cornea cannot change, so refraction here depends only on the angle of incidence of light on the cornea, which in turn depends on the distance of the object. The strongest refraction of light occurs in the cornea, and the function of the lens is the final “focusing”. The shape of the lens is regulated by the ciliary muscle: the degree of its contraction determines the tension of the ligament that supports the lens. The latter affects the elastic lens and changes its shape (surface curvature), and thereby the degree of refraction of light. As the curvature increases, the lens becomes more convex and refracts light more strongly. A complete picture of these relationships is presented in Table. 16.8. In Fig. 16.35 shows the changes that occur in the eye during accommodation for the perception of distant and close objects.
Rice. 16.35. Accommodation in the perception of light rays from objects located at different distances. A. Side view of the eye. B. Front view of the eye
Table 16.8. The relationship between the structures involved in changing the shape of the lens and the degree of refraction of light
On the retina, the image appears upside down, but this does not interfere with correct perception, since the whole point is not in the spatial position of the image on the retina, but in its interpretation by the brain.
Structure of the retina
The retina develops as an extension of the forebrain called the optic vesicle. During the embryonic development of the eye, the photoreceptor portion of the vesicle invaginates inward until it comes into contact with the vascular layer. In this case, the receptor cells find themselves lying under a layer of bodies and axons of nerve cells that connect them to the brain (Fig. 16.36).
Rice. 16.36. Schematic section of the retina with details of the ultrastructure of rods and cones. The connections between sensory cells and neurons of the optic nerve are shown. Light rays must pass through layers of ganglion cells and other neurons before reaching the rods and cones
The retina consists of three layers, each containing a specific type of cell. The outermost (farthest from the center of the eyeball) light-sensitive layer contains photoreceptors - rods and cones.
, partially immersed in the pigment layer of the choroid.
Then comes the intermediate layer
, containing bipolar neurons that connect the photoreceptors to the cells of the third layer.
In the same intermediate layer there are horizontal and amacrine cells that provide lateral inhibition. The third layer, the inner superficial layer
, contains ganglion cells, the dendrites of which are connected by synapses with bipolar cells, and the axons form the optic nerve.
Structure and function of rods and cones
Rods and cones are very similar in structure: in both, light-sensitive pigments are located on the outer surface of the intracellular membranes of the outer segment; both consist of four sections, the structure and functions of which are briefly described below.
Outer segment.
This is the photosensitive area where light energy is converted into receptor potential. The entire outer segment is filled with membranous discs formed by and separated from the plasma membrane. In sticks, the number of these disks is 600-1000; they are flattened membrane sacs and arranged like a stack of coins. Cones have fewer membrane disks and are folds of the plasma membrane.
Padding.
Here the outer segment is almost completely separated from the inner segment by an invagination of the outer membrane. The connection between the two segments is carried out through the cytoplasm and a pair of cilia passing from one segment to another. Cilia contain only 9 peripheral doublets of microtubules: the pair of central microtubules characteristic of cilia is absent.
Internal segment.
This is an area of active metabolism; it is filled with mitochondria, which supply energy for vision processes, and polyribosomes, on which proteins involved in the formation of membrane discs and visual pigment are synthesized. The core is located in the same area.
Synaptic region.
In this area, the cell forms synapses with bipolar cells.
Diffuse bipolar cells
can form synapses with several rods.
This phenomenon, called synaptic convergence, reduces visual acuity but increases the eye's light sensitivity. Monosynaptic bipolar cells
connect
one cone to one
ganglion cell, which provides greater visual acuity compared to rods.
Horizontal
and
amacrine
cells bind together a number of rods or cones. Thanks to these cells, visual information undergoes certain processing even before leaving the retina; these cells, in particular, are involved in lateral inhibition.
Differences between rods and cones
There are more rods in the retina than cones (120⋅106 and 6-7⋅106, respectively). The distribution of rods and cones is also unequal. Thin, elongated rods (dimensions 50 x 3 µm) are evenly distributed throughout the retina, except for the central fovea, where elongated conical cones (60 x 1.5 µm) predominate. Since the cones in the fovea are very densely packed (15⋅104 per 1 mm2), this area is distinguished by high visual acuity (Section 16.4.2). At the same time, rods are more sensitive to light and respond to weaker lighting. Rods contain only one visual pigment, are unable to distinguish colors and are used primarily for night vision. Cones contain three visual pigments and this allows them to perceive color; they are used mainly in daylight. Rod vision is less sharp because the rods are less densely packed and the signals from them converge, but this is what provides the high sensitivity necessary for night vision.
16.9. Explain why convergence should increase the eye's sensitivity to low light.
16.10. Explain why objects are seen better at night if you don't look directly at them.
Photoreception mechanism
The rods contain the light-sensitive pigment rhodopsin.
, located on the outer surface of the membrane disks.
Rhodopsin, or visual purple
, is a complex molecule formed as a result of the reversible binding of the lipoprotein
scotopsin
with a small molecule of a light-absorbing carotenoid,
retinal
. The latter is the aldehyde form of vitamin A and can exist (depending on lighting) in the form of two isomers (Fig. 16.37).
Rice. 16.37. Transition of 11 - cis - retinal to completely - trans - retinal under the influence of light
It has been established that when rhodopsin is exposed to light, one photon is capable of causing isomerization, shown in Fig. 16.37. Retinal plays the role of a prosthetic group, and it is believed that it occupies a specific site on the surface of the scotopsin molecule and blocks the reactive groups involved in the generation of electrical activity in the rods. The exact mechanism of photoreception is not yet known, but it is thought to involve two processes. The first of them is the conversion of 11- cis
-retinal into all-
trans
-retinal under the influence of light, and the second is the cleavage of rhodopsin through a series of intermediate products into retinal and scotopsin (a process called bleaching):
After cessation of exposure to light, rhodopsin is immediately resynthesized. Initially, completely - trans - retinal with the participation of the enzyme retinal - isomerase
turns into 11 -
cis
- retinal, and then the latter combines with scotopsin. This process underlies dark adaptation. In complete darkness, it takes about 30 minutes for all the rods to adapt and the eyes to acquire maximum sensitivity. However, during this process, the permeability of the outer segment membrane to Na+ decreases, while the inner segment continues to pump Na+ ions out, and as a result, the negative potential inside the rod increases, i.e. hyperpolarization occurs (Fig. 16.38). This is exactly the opposite of what is typically observed in other receptor cells, where stimulation causes depolarization rather than hyperpolarization. Hyperpolarization slows down the release of the excitatory transmitter from the rods, which is released in the greatest quantity in the dark. Bipolar cells connected through synapses with rods also respond with hyperpolarization, but in ganglion cells, the axons of which form the optic nerve, a propagating action potential arises in response to a signal from the bipolar cell.
Rice. 16.38. Diagram of the structure of the rod, illustrating the proposed changes in the permeability of the outer segment to Na+ under the influence of light. Negative charges on the right side of the rod correspond to resting potential, and on the left side - hyperpolarization
Color vision
In the visible part of the spectrum, the human eye absorbs light of all wavelengths, perceiving them in the form of six colors, each of which corresponds to a specific part of the spectrum (Table 16.9). There are three types of cones - "red", "green" and "blue", which contain different pigments and, according to electrophysiological studies, absorb light of different wavelengths.
Table 16.9. Colors of the visible spectrum and their approximate wavelengths
Color vision is explained in terms of the tripartite theory, according to which the sensations of different colors and shades are determined by the degree to which each type of cone is stimulated by light reflected from an object. For example, equal stimulation of all cones causes the sensation of white. Primary color discrimination occurs in the retina, but the final color that is perceived is determined by the integrative functions of the brain. The color mixing effect is the basis of color television, color photography and painting.
Color blindness.
The complete absence or deficiency of any type of cone can result in various forms of color blindness or color vision abnormalities. For example, people who do not have “red” or “green” cones do not distinguish between red and green, and those who do not have enough of either of these two types of cones have difficulty distinguishing some shades of red and green. To identify defects in color vision, test tables such as Isahari tables are used, on which specks of different colors are applied. On some tables, numbers are made from these spots. A person with normal color vision easily distinguishes these numbers, but people with impaired color vision see a different number or do not see any number at all.
Color blindness is inherited as a recessive trait linked to the X chromosome. Among men, about 2% do not distinguish between red and 6% green, while among women only 0.4% suffer from color vision anomalies.
16.11. The subject places a green filter in front of one eye and a red filter in front of the other and looks at the object. Using the data given in table. 16.9, describe his color sensations.
Binocular vision and stereoscopic vision
Binocular vision occurs when the visual fields of both eyes overlap in such a way that their fovea are fixed on the same object. Binocular vision has a number of advantages over using one eye, including a wider field of vision and the ability to compensate for damage to one eye at the expense of the other. In addition, binocular vision eliminates the blind spot effect and, finally, underlies stereoscopic vision. Stereoscopic vision is caused by the fact that slightly different images simultaneously appear on the retinas of two eyes, which the brain perceives as one image. The more the eyes are directed forward, the larger the stereoscopic field of view. In humans, for example, the total field of vision covers 180°, and the stereoscopic field of vision covers 140°. A horse's eyes are located on the sides of its head, so its frontal stereoscopic field of vision is limited and is used only for viewing distant objects. To better see a close object, the horse turns its head and uses monocular vision. Good stereoscopic vision requires forward-facing eyes with foveae located in the middle of their fields, which provides greater visual acuity. In this case, stereoscopic vision allows you to get a more accurate idea of the size and shape of an object, as well as the distance at which it is located. Basically, stereoscopic vision is characteristic of predatory animals, for which it is absolutely necessary if they catch prey by suddenly pouncing on it or diving from a height, as do representatives of the cat family, hawks or eagles. Animals that need to escape predators, on the other hand, have eyes on the sides of their heads, giving them a wider field of vision but limited stereoscopic vision. For example, a rabbit has a total visual field of 360°, but a frontal stereoscopic field of only 20°. Analysis of images obtained on the retina during stereoscopic vision is carried out in two symmetrical areas that make up the visual cortex.
Visual pathways and visual cortex
Nerve impulses originating in the retina travel along the million or so optic nerve fibers to the visual cortex, located at the back of the occipital lobes. This area is where all the smallest areas of the retina are projected, perhaps including just a few rods and cones, and it is here that visual signals are interpreted and we “see.” However, what we see becomes meaningful only after the exchange of signals with other areas of the cortex and, above all, with the temporal lobes, where previous visual information is stored and where it is used to analyze and identify current visual signals (Section 16.2.4). In the human brain, axons from the left halves of the retina of both eyes go to the left half of the visual cortex, and axons from the right halves of the retina of both eyes go to the right side of the visual cortex. The axons coming from the nasal halves of both retinas intersect; the place where they intersect is called the optic chiasm
or
chiasma
(a diagram of the visual pathways is shown in Fig. 16.39). About 20% of the optic nerve fibers do not reach the visual cortex, but enter the midbrain and participate in the reflex regulation of pupil diameter and eye movements.
Rice. 16.39. Diagram of human visual pathways. View from the underside of the brain
Do you expect to enjoy unforgettable sex with pleasant escorts? Fans of experienced service tend to be entertained by escorts from all over the world on the Internet resource prostitutkivolgogradacity.com
Internuclear ophthalmoplegia
Internuclear ophthalmoplegia is a permanent central oculomotor disorder that manifests itself as a result of changes in the area of the medial longitudinal fasciculus, which is the connecting link between the midbrain and the nuclei of the oculomotor nerves. This pathology can lead to the appearance of nystagmus in one eye and paresis of the medial rectus muscle at the site of the direct lesion. Such a disease can be either unilateral or bilateral in nature and does not tend to manifest itself with any additional neurological signs.
One of the causes of bilateral internuclear ophthalmoplegia is multiple sclerosis. As a rule, this diagnosis is made in young women. The unilateral form of the disease, on the contrary, most often occurs in older people and can manifest itself as a result of diabetes mellitus, heart attack, cerebral aneurysm and some other serious diseases.
When the central nervous system is damaged, both slow and relatively fast eye movements can be observed voluntarily. Violation of saccades leads to the development of eye dysmetry: when looking from one object to another, the eyes either “do not reach” it or “skip” it. In the most difficult situations, opsoclonus of varying severity is observed. A person may experience symptoms ranging from short bouts of saccades in the horizontal plane (ocular myoclonus) to constant chaotic saccades. Similar problems can occur in cases where the brain stem or cerebellum is affected.
Paraneoplastic syndromes, as well as neuroblastoma in children of different ages, are the cause of opsoclonus. Saccade disorders can occur as a result of various degenerative diseases of the central nervous system. Quite often the causes are Wilson's disease, as well as rapidly developing supranuclear palsy.
Congenital oculomotor apraxia
If we are talking about oculomotor apraxia, which was diagnosed from the moment of birth, then a person cannot direct his gaze to a specific point. During the first two years, saccadic movements of the head itself, which have a compensatory nature, begin to be developed. Such disorders can appear after birth as a result of problems associated with the brain stem and cerebral hemisphere.
In some cases, when the central nervous system is damaged, the smoothness of eye movements is lost - slow tracking movements become intermittent. But this is not always a symptom of pathology. These changes may occur due to certain medications or due to extreme fatigue. If such changes exist for a long time, and reading is impaired, then most likely we are talking about damage to the brain stem.
Pathologies of vergence movements can be psychogenic in nature. In some cases, it is very difficult to differentiate these changes from organic damage. Quite often, convergence is disrupted as a consequence of a stroke or severe trauma to the skull. Such patients are diagnosed with double vision, but their movements are completely normal, if convergence is not taken into account. In the case where such signs bother a person for quite a long time, we can talk about a congenital form of convergence insufficiency.
In some cases, convergence tends to persist even if a person looks into the distance. This may be caused by a convergence spasm, which is combined with constriction of the pupils and a spasm of accommodation. In this case, a spasm of accommodation can have both an organic and psychogenic nature.
How to treat convergence weakness?
a) Spasm of the reflex when looking close
(
convergence spasm
). Near gaze spasm, also called convergence spasm, is characterized by periodic spasms of convergence, miosis, and accommodation.
Complaints include headache, photophobia, eye strain, blurred vision and double vision. The patient may appear to have bilateral sixth cranial nerve palsy, but careful examination reveals miosis, and retinoscopy without cycloplegia reveals high myopia (8-10 D), combined with an abduction defect. These key clinical signs will help you avoid misdiagnosis and avoid unnecessary tests.
Most often, the spasm of the near gaze reflex is psychogenic in origin, and its treatment may include simple reassurance, psychiatric counseling or cycloplegia and the prescription of bifocals.
Near gaze reflex spasm associated with organic diseases has been described in encephalitis, tabes, labyrinthine fistulas, pituitary adenoma, Arnold-Chiari malformation, posterior fossa neoplasms, trauma, myasthenia gravis, toxic effects of anticonvulsants, midbrain neoplasms, metabolic disorders and cyclic oculomotor palsy nerve.
At the same time, it is noted that clearly functional disorders do not exclude concomitant organic pathological changes!
b) Divergence insufficiency/paralysis
. Divergence insufficiency is characterized by esotropia in distance gaze, orthophoria in near gaze, and normal convergence; esotropia may be constant or intermittent. Fusional divergence may be weakened or completely absent.
Divergence paralysis is characterized by the complete disappearance of any amount of divergence. It manifests as persistent esotropia on distance gaze with normal convergence, and usually indicates an underlying neurological disorder, such as a tumor or head injury causing increased intracranial pressure, or the onset of Miller Fisher syndrome.
In such cases, it is necessary to exclude bilateral sixth cranial nerve palsy.
c) Convergence insufficiency/paralysis
. Convergence insufficiency is characterized by weakened fusional convergence on close vision and varying degrees of exophoria (sometimes intermittent exotropia) on close vision.
It usually develops in adolescents and is accompanied by vague complaints of eye fatigue, headache, diplopia, and blurred vision when working at close distances. Eye movements and visual acuity when reading are normal, and there should be no associated neurological disorders.
Convergence insufficiency is usually not accompanied by any underlying pathology, but can accompany stress, fatigue and anxiety, and it can develop after injury or infection. Associated intracranial neoplasms are rare.
The child and parents should be reassured that there is no concomitant pathology and orthoptic exercises should be prescribed for close gaze. If orthoptic exercises are ineffective, prisms may be needed.
Complete convergence palsy is highly likely to indicate an intracranial pathological process, including encephalitis, demyelinating disease, neurosyphilis, or a condition caused by trauma or intoxication. Usually such a patient is not able to convert at all.
Diagnostics
In the case of central oculomotor disorders, patient complaints are often vague, so they provide little help in diagnosis. The main signs are poor vision, diplopia, difficulty reading, oscillopsia and some other symptoms.
As soon as there is the slightest suspicion of damage to the central nervous system, it is necessary to immediately assess the neurological status. Specialists must evaluate all oculomotor functions, eye movements in different directions, and determine strabismus. At the very end, they resort to methods that will help evaluate oculomotor reflexes. For this purpose, Bell's symptom is checked and a doll's eye test is performed.
Vergence dysfunctions
Vergence dysfunctions include:[10][11]
- Basic exophoria
- Convergence insufficiency
- Micropsy convergence
- Redundancy of divergence
- Basic esophoria
- Convergence Redundancy
- Divergence Insufficiency
- Fusional convergence dysfunction
- Heterophoria
There is evidence of a connection between vergence anomalies, in which there is a reverse crossing of the foveal projection, such that the stimulation of foveal convergence is performed as a divergence movement (instead of a convergence movement) and the emergence of schizophrenia. In this case, both conditions can be treated with non-neuroleptic methods.[12]
Convergence of the eyes: causes of disorders and treatment
In the case of diagnosis of diseases such as tumors, brain gliomas, strokes and some others, disorders associated with the eyes often appear - voluntary movements, strabismus. In cases where the nerve is affected, most often only one eye is affected, or changes are observed in both, but to varying degrees.
Damage to the central nervous system leads to oculomotor disorders such as vertical and horizontal gaze paresis, various forms of nystagmus, vertical strabismus, and ocular dysmetria. All these pathologies relate to oculomotor disorders.
Conjugate eye movement disorders
Friendly eye movements are determined by the central zones of the cerebral cortex, the cerebellum, and the midbrain. Such pathologies are diagnosed quite often when it comes to lesions of the central nervous system.
Horizontal gaze paresis occurs when one side of the pons is affected and the reticular formation is involved. If a lesion is diagnosed on both sides, then we will be talking about a complete form of horizontal paresis, and the eyes will be able to move exclusively within the vertical plane. Sometimes, if the lesion is relatively weak, only partial horizontal gaze paresis is observed or nystagmus is diagnosed. As a rule, the patient is also concerned about some other neurological signs. Moreover, the upper part of the brain stem, as well as the cerebral cortex, can lead to the manifestation of horizontal gaze paresis. Often, the so-called vestibulo-ocular reflexes that occur during such processes are virtually impossible to change.
The midbrain has the function of regulating eye movement in the vertical direction. When it comes to damage to the roof of the midbrain, upward gaze paresis is likely to occur over time. In some cases, this disease is accompanied by a weakening of the reaction of the pupils to light, but a sufficient reaction of accommodation is preserved. Young people most often suffer from such diseases as a result of hydrocephalus, and older people - due to a stroke. Downward gaze paresis is not diagnosed so often and can manifest as an acute form, for example, after a stroke, or develop gradually, which quite often manifests itself as a consequence of Parkinson’s disease, or some other diseases of the central nervous system.
Peripheral vision
Thanks to it, a person can navigate in space and see in semi-darkness.
You should turn your head to the right and catch some object with your eyes, let it be a picture on the wall, and fix your gaze on a separate element of it. If it is clearly visible, this indicates central vision. However, besides this object, other big things come into view. For example, a door to a room, a closet, a dog sitting nearby on the floor. These objects are not clearly visible, but are in the field of view, and it is possible to capture movement. This is peripheral vision. People's eyes, without moving, can cover 180 degrees of the horizon and a little less (about 130 degrees) along the vertical meridian. The acuity of central vision is greater compared to peripheral. This is due to the fact that the number of cones from the center to the peripheral part of the retina is much reduced.
Internuclear ophthalmoplegia
Internuclear ophthalmoplegia is a permanent central oculomotor disorder that manifests itself as a result of changes in the area of the medial longitudinal fasciculus, which is the connecting link between the midbrain and the nuclei of the oculomotor nerves. This pathology can lead to the appearance of nystagmus in one eye and paresis of the medial rectus muscle at the site of the direct lesion. Such a disease can be either unilateral or bilateral in nature and does not tend to manifest itself with any additional neurological signs.
One of the causes of bilateral internuclear ophthalmoplegia is multiple sclerosis. As a rule, this diagnosis is made in young women. The unilateral form of the disease, on the contrary, most often occurs in older people and can manifest itself as a result of diabetes mellitus, heart attack, cerebral aneurysm and some other serious diseases.
When the central nervous system is damaged, both slow and relatively fast eye movements can be observed voluntarily. Violation of saccades leads to the development of eye dysmetry: when looking from one object to another, the eyes either “do not reach” it or “skip” it. In the most difficult situations, opsoclonus of varying severity is observed. A person may experience symptoms ranging from short bouts of saccades in the horizontal plane (ocular myoclonus) to constant chaotic saccades. Similar problems can occur in cases where the brain stem or cerebellum is affected.
Paraneoplastic syndromes, as well as neuroblastoma in children of different ages, are the cause of opsoclonus. Saccade disorders can occur as a result of various degenerative diseases of the central nervous system. Quite often the causes are Wilson's disease, as well as rapidly developing supranuclear palsy.
Congenital oculomotor apraxia
If we are talking about oculomotor apraxia, which was diagnosed from the moment of birth, then a person cannot direct his gaze to a specific point. During the first two years, saccadic movements of the head itself, which have a compensatory nature, begin to be developed. Such disorders can appear after birth as a result of problems associated with the brain stem and cerebral hemisphere.
In some cases, when the central nervous system is damaged, the smoothness of eye movements is lost - slow tracking movements become intermittent. But this is not always a symptom of pathology. These changes may occur due to certain medications or due to extreme fatigue. If such changes exist for a long time, and reading is impaired, then most likely we are talking about damage to the brain stem.
Pathologies of vergence movements can be psychogenic in nature. In some cases, it is very difficult to differentiate these changes from organic damage. Quite often, convergence is disrupted as a consequence of a stroke or severe trauma to the skull. Such patients are diagnosed with double vision, but their movements are completely normal, if convergence is not taken into account. In the case where such signs bother a person for quite a long time, we can talk about a congenital form of convergence insufficiency.
In some cases, convergence tends to persist even if a person looks into the distance. This may be caused by a convergence spasm, which is combined with constriction of the pupils and a spasm of accommodation. In this case, a spasm of accommodation can have both an organic and psychogenic nature.
Types
The following types of vergence operate in superposition:
- Tonic vergence
: Vergence with normal extraocular muscle tone, without accommodation and without stimulation to binocular fusion. Tonic vergence is the movement of the eyes from the anatomical resting position (the position without innervation) to the physiological resting position.[2] - Accommodative vergence
: Vergence for the purpose of focusing. - Fusional vergence:
(also:
disparity vergence
,
motion disparity vergence
or
vergence reflex
[2]): vergence induced by a binocular fusion stimulus. - Proximal vergence
: Vergence due to the conscious fixation of objects that are close or far away in the absence of incongruity and signals for accommodation. This also includes vergence, which is the subject's intention to see an object in the dark.[3]
Proximal vergence is sometimes called volitional vergence, which, however, more generally means vergence of volitional control and is sometimes considered a type five vergence.[4] Volitional vergence is also required for viewing autostereograms and for volitional gaze crossing. Volitional convergence, as a rule, is accompanied by accommodation and miosis (constriction of the pupil); However, often, with widespread practice, people can learn to dissociate accommodation and vergence.[5]
Vergence is also designated according to its direction: horizontal vergence, vertical vergence and cyclovergence (torsion). Horizontal vergence is further divided into convergence (aka: positive vergence) and divergence (aka: negative vergence). Vergence eye movements are the result of the activity of six extraocular muscles. They are controlled by three cranial nerves: the abducens nerve, the trochlear nerve, and the oculomotor nerve. Horizontal vergence is provided mainly by the medial and lateral muscles.
Convergence
In ophthalmology, convergence is the simultaneous inward movement of both eyes toward each other, usually to maintain a single binocular vision when viewing objects.[6] Only this is not a conjugate movement, but only an adduction of the eyes.[7] Convergence is one of three processes in the eye that correctly focuses images on the retina. The visual axis of each eye will point toward the object of interest in order to focus it correctly.[8] This action is mediated by the medial rectus muscle, which is innervated by the cranial nerve. This is a type of vergence that is performed by the external muscles. Diplopia, commonly referred to as double vision, can occur if one of the outer eye muscles is weaker than the other. This happens because the object in question is projected onto different parts of the retina, causing the brain to see two images.
Convergence insufficiency is a common eye problem and a leading cause of eye fatigue, blurred vision, and headaches.[9] This problem most often occurs in children.
Near Point of Convergence (NPC) is measured by holding an object close to the nose and observing when the patient begins to see double or when one eye no longer deviates. Normal NPC values are up to 10 cm. Any NPC value at a distance greater than 10 cm is usually a consequence of high exophoria nearby.
Divergence
Divergence of the right eye while the left is relatively stable is an example of partial divergence.
Divergence in ophthalmology is the simultaneous movement outward of both eyes from each other, usually in order to maintain binocular vision when viewing objects. This is a type of vergence eye movement.
Diagnostics
In the case of central oculomotor disorders, patient complaints are often vague, so they provide little help in diagnosis. The main signs are poor vision, diplopia, difficulty reading, oscillopsia and some other symptoms.
As soon as there is the slightest suspicion of damage to the central nervous system, it is necessary to immediately assess the neurological status. Specialists must evaluate all oculomotor functions, eye movements in different directions, and determine strabismus. At the very end, they resort to methods that will help evaluate oculomotor reflexes. For this purpose, Bell's symptom is checked and a doll's eye test is performed.
EYE CONVERGENCE
Convergence of eyes
(lat. convergere converge, come closer) - the physiological act of bringing together the visual axes of both eyes on a fixed object.
Convergence of the eyes is carried out due to the simultaneous contraction of the internal rectus and partly the superior and inferior rectus muscles of both eyes; accompanied by constriction of the pupils - miosis (see) - and tension in the accommodation of the eyes (see). These three reflexes are components of one complex act of visual placement of the eyes at a close distance (Fig. 1). The following types of blood pressure are distinguished: 1) tonic, caused by the tone of the external muscles of both eyes; 2) accommodative, associated with the tension of accommodation and due to the synchronous interaction between accommodation and convergence; 3) fusion, caused by the reflex of binocular fixation of an object; 4) proximal, which occurs when an object approaches the eyes. The metroangle is taken as a unit of K., i.e., the angle that the visual line (see) forms with the perpendicular restored from the middle of the nose, when the eyes fix a point located at a distance of 1 m from them. Thus, at two metroangles, the eyes converge to a point lying at a distance of 0.5 m, etc. The state of the eye is determined by the nearest point of convergence (normally it is 6 - 10 cm) - the distance from the approaching object to the external one the corner of the orbit at the moment when one eye stops fixating the object and begins to deviate outward. Increased convergence of the eyes with significant hypermetropia and weakened convergence with myopia in some cases can lead to strabismus (convergent or divergent, respectively). Maximum K. g., with a cut binocular fusion is still possible, characterizes the amount of positive fusion reserves. The normal positive value of fusion (see) for distance and near is 24-28 prism diopters. Objective registration of K. and changes in pupil size is possible using the method of photoscanning pupillography (Fig. 2).
Determination of eye accommodation
Accommodation is an adaptive reaction of the eye that has developed over millions of years of evolution and allows a person to see clearly and clearly in a wide range of illumination, from almost any distance to an object, be it a tiny splinter in the little finger or a herd of mammoths on the horizon. This optical adaptation is achieved by the automatic “triggering” of a special intraocular mechanism: the multifunctional ciliary (ciliary) body, connected by muscle fibers to the pupil and lens, tenses or relaxes, depending on the brightness and distance. If we turn to the obvious and generally accepted analogy between the structure of the eye and the design of the camera (in both cases the same physical laws of optics apply), the pupil performs the function of a diaphragm, and the lens, by the force of the ciliary muscle, changes the curvature of the surface from almost spherical to flatter. the role of an autofocusing lens with variable refractive power.
Needless to say about the importance of the biomechanical mechanism of accommodation. Any paresis (partial paralysis), lack of muscle effort, or, conversely, inability to relax to the required degree (spasm of accommodation) naturally leads to ametropia - myopia or farsightedness, i.e. inability to see clearly at distance or near. Therefore, ophthalmologists have long sought to find, and persistently developed, methods for reliable, accurate and reliable diagnosis of the functional status of the accommodative system. Considering the exceptional fragility and tightness of the visual organ (obviously, it cannot be subjected to even simple palpation or, say, percussion, i.e., palpating or “tapping”), diagnostic methods must be non-invasive, non-contact and, by and large, indirect. Today, this methodology is quite well developed in ophthalmology: special concepts characterizing accommodative capabilities (absolute, relative, vergence, cycloplegic accommodation) have been introduced into scientific and clinical circulation, and various methods of assessing these most important indicators for vision are used - ergography, volume measurement accommodation, etc.
Thus, the volume of absolute accommodation is the increment in the optical power of the lens “lens” between two extreme states available in a specific individual case - from complete relaxation to maximum tension of the ciliary muscle. In each eye, this indicator can vary, sometimes quite significantly, so it is diagnosed separately on the right and left. The volume of absolute accommodation is measured in the same extra-system units of refractive power as the optical “power” of glass lenses - in diopters. Calculation formula A = P ± R), where P is the so-called. clinical refraction of the eye (position of the focal point in relation to the retina), and ±R is the clinical refraction when setting the gaze at the closest and most distant points of clear vision.
To determine the greatest available distance for clear discrimination, special medications (eye drops) are used that block the ability of the ciliary muscle to contract, i.e. temporarily holding the accommodative apparatus in its most relaxed state. It is easier to identify the closest accessible point of clear vision: the patient is presented with a text in small print and asked to read it fluently. To convert the result into diopters, divide 100 by the distance (in centimeters) with which the patient confidently completes the task.
Actually, absolute accommodation (as opposed to its volume) is the adaptive reaction of one eye independently of the other. As is known, human vision is binocular - the presence of two organs of vision separated horizontally (even if the distance between the pupils is only ten centimeters) allows us to see the world in volume and to estimate with sufficient accuracy, for example, the distance between two cars located in the distance on the same road as us lane. If the gaze is directed to infinity, the ocular optical axes are almost parallel; when focusing on a specific object, these conditional straight lines must intersect on it. Usually this is not felt physically and is not noticed by an outside observer, but when we try to examine, for example, the tip of our own nose, it is noticeable from the outside how the eyeballs turn towards the bridge of the nose, sharply reducing the distance between the pupils and bringing together the longitudinal optical axes. This process is called “convergence” (from the Latin “to converge”, “to come closer”). It is obvious that as the observed object approaches the eyes, to clearly distinguish it, increasingly stronger accommodation (an increase in the curvature and, accordingly, the refractive power of the lens) and convergence (convergent rotation of the eyeballs) are required. Thus, accommodation and convergence are normally interdependent, coordinated - technically speaking, autosynchronized - processes.
Normal (emmetropic) vision is considered to be such vision in which focusing on a point one meter away from the eyes requires an accommodation shift of one diopter, and when this distance is reduced to exactly one third (0.333 m), accommodation of up to three diopters is required.
Accommodation is called relative, defined taking into account its interdependence with the process of convergence. This indicator is always less than absolute accommodation, which would be observed in the absence of converging muscle effort. But, since the eye is still a living and elastic biological organ, the external oculomotor muscles, upon convergence, exert noticeable pressure on the eyeball and somewhat lengthen its anatomical axis.
Relative accommodation is considered in its positive and negative parts. With a fixed convergence, the negative part is the share of the accommodation resource already spent on focusing, and the positive part is the accommodation capabilities that remain in reserve and are available in case of further approach of the object. It is not difficult to deduce the basic pattern of the mutual relationship between accommodation and convergence: with weak refraction and strong convergence of the eyeballs, the negative part of the relative accommodation is greater, and under the opposite conditions - strong refraction and weak convergence - the accommodation expended is correspondingly less.
Relative accommodation and its “floating” components (negative and positive) are determined empirically: the patient is put on special glasses and the strongest lenses are selected for them, concentrating and dispersing, through which it is difficult, but clarity of vision is maintained at a fixed point (i.e. with a further slight increase in the optical power of these glasses, focusing vision on the object would no longer be possible). The negative part of the accommodation is equivalent to the refractive power of the collecting lens, and the positive part is equivalent to the diverging power.
Despite the scientific and technical sound and the seemingly theoretical detachment of these calculations, they are extremely important, first of all, in practice. Thus, during vocational guidance, selection and prevention of occupational diseases, it should be taken into account that many types of activities require constant intense concentration of attention on nearby objects (small parts, text, symbols on the monitor, sewing, etc.). Under such conditions, the eyes must have sufficient accommodative reserve (positive accommodation) so that work does not require the maximum available visual voltage. Otherwise, the ciliary muscles work in a forced mode, i.e. if they provide clear vision, it is only at the cost of constant overload, which leads to asthenopia (chronic fatigue, rapid eye fatigue) and can significantly reduce visual acuity as such. Many people are familiar with the uncomfortable feeling of visual helplessness, when objects of activity lose clarity, merge, blur, and therefore a person is forced to stop work for one time or another (in a number of professions, continuing it “by force of will” is simply dangerous). Typically, this type of activity requires more than just healthy normative vision; the positive, reserve part of accommodation should be approximately twice as large as the negative, used part of the adaptive capabilities of vision. This individual proportion must be taken into account not only when choosing a profession, but also when prescribing corrective glasses to patients with refractive errors.
In addition to the direct selection of lenses, other methods are also used, including instrumental methods for studying accommodation. Thus, in ophthalmology (as well as in related branches of knowledge - physiology, psychology, etc.) they use special “action recorders”, or ergographs (literally “to record work”). Using an ergograph, special curves are drawn, reflecting, in particular, the dynamics of the spatial position of a point of clear focus over a certain period of time - which makes it possible to judge the endurance and adaptability of the oculomotor muscular system and accommodating ciliary muscles.