With conjunctival chemosis, severe swelling of the conjunctiva of the eye occurs. The mucous membrane consists of two parts (bulbar and tarsal), which are connected by a transitional fold. Near the inner corner of the eye there is a lacrimal caruncle and a semilunar fold.
The tarsal zone of the conjunctiva is directly adjacent to the base and is tightly connected to it. The bulbar part, on the contrary, is loosely connected to the base, so it is easy to lift. The transition from the epithelial cover of the conjunctiva to the epithelial layer of the cornea is very smooth, because both of these types of cells are close in embryological origin.
Symptoms
The peculiarity of the disease is that in the initial stages it occurs without any visible symptoms. The amount of fluid accumulated between the layers of the conjunctiva at the beginning of the disease is small, so only an ophthalmologist can detect the development of pathology. As a rule, this happens by chance during a routine medical examination of the eyes.
As chemosis progresses, the following symptoms begin to appear:
In the absence of treatment and poor hygiene, the pathology can spread to the second eye, as a result of which the patient has serious problems with visual perception. When a bacterial infection occurs, photophobia develops.
How does conjunctival chemosis manifest?
At the very beginning of the development of the disease, symptoms are almost absent. The disease can only be detected by a doctor during an examination, but patients turn to an ophthalmologist when signs such as:
- severe itching, burning, pain in the eyes;
- blurred vision;
- painful sensations when blinking;
- purulent discharge from the eyes.
The last sign occurs when an infection is added to the inflammation. In severe forms of chemosis, swelling spreads to both eyes.
Causes
Conjunctival chemosis can be caused by the following factors:
- chemicals or foreign bodies that may have gotten into the eye;
- neoplasms and tumors developing in the periorbital region;
- problems with the outflow of fluid in the conjunctival region and beyond;
- constant contact with harmful substances when working in the chemical industry;
- use for therapy of drugs, the components of which may cause the development of individual intolerance or hypersensitivity;
- living in a dry climate;
- dust entering the organ of vision.
With the development of a severe form of the disease, inflammation of the mucous membrane is a completely expected complication, which is caused by the formation of a huge number of harmful microorganisms in the upper layer of the organ of vision.
Causes of the disease
Note! Chemosis of the conjunctiva can develop for the following reasons and in the presence of such predisposing factors as:
- contact with the conjunctival membrane of chemicals and contact with foreign bodies in the eyes;
- conjunctivitis, phlegmon, barley and other infectious pathologies that cause inflammatory processes;
- the appearance of tumors and neoplasms in the bulbar region;
- stagnation of fluids in the conjunctival area and under it;
- constant contact with chemicals and reagents (for example, when working in chemical plants);
- use for treatment of medications to the components of which the patient may have hypersensitivity;
- dry climate;
- dust getting into your eyes.
In severe forms of conjunctivitis, chemosis is a completely expected complication caused by the accumulation of a large number of pathogenic microorganisms on the conjunctival membrane.
In this case, the lesion can spread both to individual areas of the conjunctiva and to its entire surface , which can lead to the inability to completely close the eyelids due to protrusion of the conjunctiva.
As a rule, the pathology is characterized by unilateral development, but often the painful processes spread to the second organ of vision.
Causes
The main and most common cause of the disease is conjunctivitis.
If the disease develops against the background of conjunctivitis, long-term swelling is observed and intense pain occurs in the eyes.
The causes of chemosis that occurs with conjunctivitis may be dry air, infections, corneal swelling, allergies, or periorbital edema.
Dry eyes
In conditions of increased dry air, the risk of developing edema in patients with conjunctivitis increases significantly. Swelling can also form after prolonged exposure to the street in hot, windy weather, or as a result of prolonged work at the computer. Dry eyes are accompanied not only by the formation of conjunctival edema, but also by a feeling of sand and discomfort in the eyes.
Infectious conjunctivitis
Chemosis in conjunctivitis can also be caused by infections. If they penetrate the mucous membranes, pain occurs when moving the eyes, burning, tear production increases, and sometimes pus is present in the tear fluid.
Corneal edema
Another cause of chemosis that occurs against the background of conjunctivitis is inflammation of the cornea due to its damage by viruses, bacteria or fungi. With this pathology, a person is bothered by eye pain, severe swelling, photophobia, and burning. In the morning, after waking up, it is impossible to open the eyelids without rinsing the eyes with warm water. In case of damage to the deep tissues of the cornea, a significant decrease in vision may occur.
Periorbital edema
The development of periorbital edema is caused by damage to the eyes, brain and other organs. Often, after a brain injury, chemosis is localized in the area of the bridge of the nose, since brain injuries cause internal organs to swell and blood flow to be disrupted. One of the distinctive signs of this pathology is the formation of large bruises under the eyes.
Chemosis in allergies
In people prone to allergies, chemosis can develop upon contact with cosmetics, pollen, room dust and other allergenic factors. The pathology is accompanied by swelling and redness of one or both eyes.
Other reasons
Chemosis can also be caused by:
- Barley is a pathology in which a compaction with purulent contents forms on the lower or upper eyelid.
- Blepharitis is characterized by inflammation and redness of the edge of the eyelids in the eyelash area. Blepharitis often occurs due to damage to the sebaceous glands by mites.
- Eyelid abscess - this pathology is characterized by the development of infiltrative purulent inflammation.
- Orbital phlegmon is a condition in which a purulent-inflammatory process occurs in the orbital retina.
- Burns to the mucous membranes of the eyes can occur due to exposure to UV rays or any chemical substance.
- Entry of a foreign body, injury to the eye.
In addition, chemosis can develop due to any pathological process in the body. So, often the disease occurs against the background of:
- endocrine diseases;
- brain inflammation;
- tumor processes;
- exophthalmos (pathological displacement of the eyeball);
- vascular diseases, stagnation of blood in the veins;
- skin tuberculosis.
If chemosis occurs as a result of the listed pathologies, the disease is characterized by a long course, and local treatment does not give a positive result.
Causes of the disease
There are many reasons for the development of chemosis. The following factors can provoke it:
- exposure to a number of chemical substances on the tissues of the eye, which at first may seem harmless to health (also provoke swelling and chemical substances in the air that constantly affect the conjunctiva, for example, when working in chemical plants);
- getting foreign bodies, as well as dust and pollen into the eyes;
- development of conjunctivitis;
- the appearance of phlegmon and abscesses;
- a number of other infectious and bacterial pathologies that provoke the development of inflammatory processes;
- the appearance of neoplasms;
- stagnation of fluids;
- use of certain medications;
- too dry indoor and outdoor air;
- barley (meibomite).
Attention! Chemosis is a common complication observed with conjunctivitis. True, it usually develops with severe forms of the disease or lack of timely treatment.
Chemosis can also be provoked by allergic reactions, blepharitis, exophthalmos, that is, displacement of the eyeball, and demodicosis of the eyelids. Sometimes the cause of the development of pathology is problems with blood vessels (for example, blood stagnation). In any case, it will never develop from scratch.
In general, chemosis can be called one of the main serious signs of the development of a number of pathologies and complications, including it can signal problems with the condition of the brain, the development of endocrine pathologies, and neoplasms. It definitely requires timely and most effective treatment, which will be selected by the doctor after visiting the clinic.
Attention! If chemosis is the result of the development of serious pathologies of the body as a whole, then the inflammatory processes may be protracted, and treatment will not give a full effect. But with allergies, chemosis goes away quickly, but also develops at a gigantic speed, literally in a matter of minutes.
Chemosis in allergies
Common causes of conjunctival swelling are various allergic reactions. In these cases, chemosis develops quite quickly, sometimes severe inflammation, which prevents you from closing your eyes, occurs literally in minutes. At the same time, it can subside just as quickly - it is enough for a person to take an antihistamine or eliminate contact with the allergen.
The most dangerous thing about this kind of swelling is that the eye begins to itch very much, and a person can damage the inflamed cornea. And the injury will lead to other complications, in particular, infection.
Swelling of the eye occurs both in contact allergies (when a substance gets directly into the eye) and among other symptoms in a general allergic reaction. In the second case, chemosis necessarily affects both eyes, and the person also experiences:
- Severe lacrimation.
- Allergic rhinitis.
- Sneezing.
Swelling of the mucous membranes of the respiratory tract, sometimes with noticeable difficulty breathing. These symptoms can lead to:
- Plant pollen.
- Dust.
- Household chemicals.
- Washing powder.
- Animal fur.
- Food.
- Perfumery.
Contact allergies may only affect one eye. Among the allergens that cause a local reaction, the most common are medications (eye drops and gels) and cosmetics.
Edema of the conjunctiva: causes
The mucous membrane of the eyes or conjunctiva is constantly exposed to external factors.
If the inflammatory process is not diagnosed in time, swelling may begin, impairing the functionality of the visual system. Swelling of the conjunctiva of the eyeball or chemosis - can most often be observed with eyelid stye (acute purulent inflammation), panophthalmitis (purulent inflammation of all tissues of the eyeball), malignant exophthalmos (“protrusion” forward of the eyeball) and other tumors, allergic reactions to medications. It may be limited or completely cover the conjunctiva of the eyeball. The causes of conjunctival edema can be acute and local. Among the most common causes are: acute inflammation of the adnexal apparatus and membranes of the eye, insect bites, the appearance of barley on the eye, orbital cellulitis (inflammation of the eye tissue behind the orbital septum), gonorrheal conjunctivitis (a vision-threatening pathology that develops with gonorrhea), microcirculation disorders or blood congestion, which may be caused by the impact or pressure on the eye from tumors in the orbital areas (the area around the eyeball). Often, with swelling of the conjunctiva, anemia (anemia), nephritis (inflammation that leads to changes in paired organs), and urticaria (skin disease, mainly of allergic origin) are diagnosed.
The causes of the disease may be eye pathologies, traumatic brain injuries, or uncontrolled use of medications.
Diagnosis of chemosis
Since there are many reasons for the development of the disease, if chemosis is suspected, the doctor should not only examine the eyes, but also interview the patient to find out what specific factor could provoke the pathology, when it appeared and how it developed.
In addition to visual examination and oral questioning, the following diagnostic methods are used:
- biomicroscopy;
- ophthalmoscopy;
- Ultrasound, CT;
- X-ray;
- visometry;
- scraping of mucous membranes, blood tests and other laboratory methods.
Also, if necessary, tonometry is performed - a method by which intraocular pressure is determined. During the diagnostic process, it is necessary to exclude the presence of an abscess, tumors, and skin tuberculosis.
Diagnostics
The subconjunctival layer in newborns is not sufficiently developed. Its complete formation ends by the end of the first year of life. The loose layer of connective tissue contains a large number of lymphatic formations. The tarsal conjunctiva has folds, when cut, glandular formations can be detected.
Stratified columnar epithelium also contains goblet cells, which can grow against the background of various pathological conditions.
If microcirculation is disrupted in the conjunctival area, the pathological process leads to some significant transformations. Swelling, hyperemia, and hemorrhages occur, indicating a local and systemic disease.
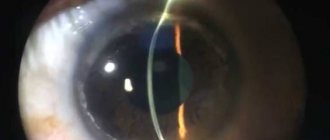
Typically, swelling occurs in the area of the transitional fold and conjunctiva. Chemosis of the latter is sometimes so pronounced that it first covers the cornea and then begins to protrude from the palpebral fissure.
Conjunctival dystrophy
Pinguecula (wen)
Pinguecula is a limited thickening of the conjunctiva that appears in the area of the inner edge of the cornea.
It occurs in older people as a result of eye irritation by external factors. The pathology may look like a small cosmetic defect. Removed in rare cases, at the request of the patient.
Pterygium
Pterygium (or pterygoid pleura) is an analogue of the mucous membrane of the eyeball, has a triangular shape and grows into the surface of the cornea from the side of the nose. The reason is mechanical, chemical irritants, long exposure to the sun without dark glasses.
The non-progressive form of pterygium does not require surgical treatment.
The progressive form of the pterygoid pleura begins to grow towards the center of the eye. Due to this growth, the following symptoms appear: redness and irritation of the eye, watery eyes, decreased vision due to astigmatism. In such a situation, surgery is necessary.
1 Diagnosis and treatment of conjunctivitis
2 Diagnosis and treatment of conjunctivitis
3 Treatment of conjunctivitis
Dry eye syndrome
Dry eye syndrome is a violation of the wetting of the surface of the eye due to changes in the quantity and quality of tear fluid, as well as rapid evaporation of the tear film.
Our eye is protected by an ultra-thin, three-layer tear film. The top oily layer allows the upper eyelid to glide over the surface of the eye and prevents the other two layers from drying out.
The middle layer (aqueous, with electrolytes) supplies the cornea with nutrients, protects the eye and flushes foreign bodies out of it.
The third mucin layer ensures the smooth surface of the cornea and maintains clear vision. Violation of the stability of the tear film leads to dryness of the surface of the conjunctiva and cornea and the appearance of dry eye syndrome.
This pathology is called the “disease of civilization”, since long hours of work at the computer, unhumidified air from air conditioners and prolonged wearing of contact lenses greatly contribute to the appearance of the disease.
Other causes of dry eye syndrome can be: endocrine disorders, pathology of the visual organs, connective tissue diseases, vitamin deficiency, and the use of certain medications.
Symptoms of dry eye syndrome:
The following signs of dry eye syndrome can be identified:
- feeling of sand in the eyes, dryness and pain (may increase at the end of the day);
- redness of the eyes;
- blurred vision that disappears when blinking;
- eye discomfort after reading or working at the computer.
Therapy
The method of therapy is selected depending on what specific factor caused the disease. Moderate and mild degrees of chemosis are treated at home, using medications and traditional medicine. In severe situations requiring surgical intervention, the patient is hospitalized and then undergoes surgery.
Drug treatment
Antibiotics, antivirals, antihistamines or vasoconstrictors are used as conservative agents:
- Antibiotics - eye drops containing antibacterial components are most often used - Oksamycin, Gentamicin, Tobrex, Floxal. If necessary, as a supplement to the drops, the doctor may prescribe antibiotic tablets.
- Antiviral - used if the disease was caused by viruses. Poludan, Indoxuridine, Acyclovir are used as such drugs.
- Antihistamine and vasoconstrictor drops help eliminate symptoms that occur due to allergies.
Surgical
The operation is prescribed if chemosis was caused by a tumor process in the eye, internal barley, or an abscess of the eyelid. In addition, surgery may be required for exophthalmos and other pathologies.
ethnoscience
Traditional recipes can only be used as an adjunct to drug treatment.
It must be remembered that the use of “grandmother’s” recipes without medications and medical supervision can lead to the development of severe complications and serious impairment of the function of the visual organs.
Among folk remedies, the most effective are:
- Eye lotions made from marshmallow roots. An infusion is prepared from the roots of this plant (200 ml of water and 3 tablespoons of crushed raw materials), cotton pads are soaked in the resulting mixture and applied to the eye sockets.
- Lotions from rosehip decoction prepared from 200 ml of water and 2 teaspoons of chopped berries. After boiling for 5 minutes, the broth must be left for 30 minutes and then strained.
- Honey-based eye drops - prepared from 300 ml of water and 1 teaspoon of natural honey. Fresh drops must be prepared every day. When diluting honey in water, do not use boiling water.
- Fresh cherry juice - used both for washing the eyes and as a lotion for the eye sockets. It is also useful for patients with chemosis to consume at least a glass of cherries daily.
- Lotions made from chamomile infusion. The infusion is prepared from 200 ml of water and 1 tbsp. spoons of plant flowers.
Diseases
Depending on the cause that caused the development of the pathological process, the disease can take the following forms:
- Allergic. The pathology is caused by various types of allergens (pollen, pets, smoke). In this case, inflammation is observed not only of the organ of vision, but also of the nearby soft tissues. It is a consequence of the body’s reaction to the allergen in the form of the release of histamines.
- Bacterial. The causative agents are harmful bacteria. Among the key symptoms include increased formation of purulent discharge.
- Viral. Formed against the background of the development of a viral infection.
Conjunctivitis
Conjunctivitis comprises a whole group of eye diseases characterized by inflammation of the outer mucous membrane of the eye (i.e., conjunctiva) and the inner surface of the eyelids.
As with any disease, conjunctivitis has acute and chronic forms .
In the acute form of the disease, inflammation (with pain, burning and mucopurulent discharge) appears first in one eye, and a week later in the second. The average duration of the disease is 4 weeks.
In the chronic form of conjunctivitis, the inflammatory process lasts quite a long time, more than a month.
Symptoms of conjunctivitis
Naturally, the signs of the disease depend on the cause that caused this pathology. However, we can name the general symptoms of conjunctivitis:
- swelling and redness of the mucous membrane of the eye (red eye color is a typical sign of this disease);
- purulent or mucous discharge from the eyes;
- burning and itching in the eyes;
- poor tolerance to bright light;
- sensation of a foreign body or sand in the eye.
Types of conjunctivitis
There are the following types of conjunctivitis: viral , bacterial , allergic .
Viral conjunctivitis (in most cases - adenoviral conjunctivitis) often occurs with colds. The impetus for its appearance can be catarrhal rhinitis, accompanied by a sore throat and elevated body temperature. The disease begins in one eye and then moves to the other. Symptoms of this disease: severe lacrimation, itching, discharge of non-purulent mucus.
Bacterial conjunctivitis can be recognized by the following characteristic symptoms:
- viscous and cloudy discharge from the eye, usually gray or yellow, causing the eyelids to stick together after sleep;
- dryness of the conjunctiva and skin around the affected eye;
- inflammation of only one eye (but then the second eye may also become inflamed);
- pain and sensation of a foreign object.
With allergic conjunctivitis, both eyes become inflamed at once. The disease may appear as a result of allergies to flowering plants, food, inappropriate cosmetics, or as a reaction to certain medications.
In addition to such “classic” symptoms of conjunctivitis as redness of the eye, itching and lacrimation, with this type of disease there is a slight swelling of the conjunctiva and eyelids.
1 Diagnosis and treatment of conjunctivitis
2 Diagnosis and treatment of conjunctivitis
3 Treatment of conjunctivitis
Conjunctivitis that occurs when exposed to chemicals or toxic substances . With this type of disease there is no itching or discharge from the eyes, but there is pain and irritation in the eye.
Viral and bacterial conjunctivitis are contagious and can be transmitted through airborne droplets or dirty hands!
Causes of conjunctivitis:
- allergic reactions to fluff, pet hair, dust and flowering plants, as well as household chemicals;
- thermal, chemical burns and other eye injuries;
- viral infections: herpes, influenza, measles, rubella, adenovirus, molluscum contagiosum;
- autoimmune diseases: Reiter's syndrome, psoriasis, gout, sarcoidosis;
- bacterial infections caused by chlamydia, pneumococci, gonococci, diphtheria bacillus, etc.;
- fungal infections of the eyes: coccidiosis, candidiasis, actinomycosis, etc.
Predisposing factors for the development of the disease are:
- hypothermia of the body;
- incorrect wearing of contact lenses;
- failure to comply with personal hygiene rules;
- avitaminosis;
- work associated with prolonged tension of the visual apparatus;
- frequent chronic diseases;
- farsightedness, nearsightedness and astigmatism;
- prolonged exposure to ultraviolet rays.
Diagnosis of conjunctivitis
The disease is detected during an examination by an ophthalmologist; to clarify its cause, the following methods can be used:
- general blood analysis;
- microscopy of eye discharge - detects the causative agent of conjunctivitis;
- bacteriological culture - helps to determine the sensitivity of the pathogen to various drugs;
- biomicroscopy (examination of the affected eye under a microscope) shows all changes in the conjunctiva and cornea.
Treatment of conjunctivitis
Treatment of conjunctivitis is carried out according to a special scheme, which depends on the type of pathology. As a rule, eye drops are prescribed to relieve itching, swelling, and inflammation.
For allergic conjunctivitis, antihistamines are selected, as well as eye drops and ointments that block the development of infection.
For bacterial or viral diseases, interferon and drops (ointments) including antibiotics are prescribed.
Therapy of the disease is based not only on eliminating the infection, but also restoring the human immune system.
When treating conjunctivitis, it is not recommended to take medications not prescribed by a doctor! If purulent (gonococcal) conjunctivitis is not treated correctly, it can lead to serious damage to the cornea and even complete blindness!
Only an ophthalmologist, after identifying the cause of the disease, can recommend adequate treatment.
Possible complications
Chemosis is a serious disease, the danger of which is a high risk of developing blindness or a significant decrease in vision, which in most cases is irreversible. If the disease is not treated in a timely or competent manner, the inflammatory process can spread to the cornea and lead to the development of keratitis.
Conjunctival tissues, unlike the cornea, have good regenerative abilities, so proper and timely treatment, as a rule, allows you to quickly get rid of the disease.
Forecast
The prognosis of chemosis depends on the underlying disease. Depending on it, recovery can occur quickly, within a few days (for example, with allergic conjunctivitis after eliminating contact with the allergen).
But the pathology can have serious consequences and even lead to loss of vision, in particular with keratitis, gonoblenorrhea or a malignant tumor in the orbit. In any case, the prognosis of chemosis should be considered serious until diagnosis is made.
Possible complications
Chemosis itself is a complication of ocular or systemic diseases. Untreated disease or inadequate treatment can lead to keratitis, characterized by ulceration and clouding of the cornea, and decreased visual acuity. In the worst case, the matter can end in a thorn and complete blindness.
Treatment options
After conducting a detailed diagnosis and identifying the cause of the disease, the doctor selects the optimal course of therapy.
Medicines
When prescribing medications, the doctor is based on the etiology of the anomaly:
- Antibiotics. The drugs are prescribed when the conjunctiva is damaged by harmful bacteria. The medication is used for several days six to eight times a day. After the symptoms subside, the frequency of use is reduced. Most often, doctors prescribe drugs such as Tobramycin, Floxal, Okamicin;
- If the cause of the disease is hidden in infection by pathogenic viruses, then doctors select antiviral medications (Acyclovir, Poludan, Indoxuridine). The greatest effectiveness of taking the drugs is observed on the first day of therapy;
- If the symptoms are caused by an allergic reaction, antihistamines and vasoconstrictors are used. The result of taking them will only be if contact with the irritant has been previously eliminated.
Any medications are prescribed by a doctor after a detailed diagnosis. Return to contents
Surgical methods
The advanced form of chemosis cannot always be cured with medications. In this case, doctors recommend surgical intervention. It is prescribed if additional diseases develop against the background of swelling:
- Bug-eyed;
- The appearance of stye on the inside of the eyelid;
- Abscess;
- Orbital neoplasms.
During the operation, damaged areas are excised and repaired. If there is no threat of complications, then the disease is treated at home using conservative methods.
Folk remedies
At the same time as taking medications, you can try “grandmother’s recipes.” Doctors also recommend resorting to their help at the rehabilitation stage. The following remedies are most effective:
- Compresses based on marshmallow. Combine two hundred grams of boiled water, cooled to room temperature, with three tablespoons of the plant. Leave for eight hours. Soak cotton pads or gauze in the prepared broth. Apply to the damaged eye four times a day;
- Take any honey and dilute it in a liter of boiled or bottled water. Use the prepared composition as eye drops twice a day;
- Boil a couple of teaspoons of dried rose hips in water (two hundred grams) for five minutes. Leave for half an hour for the solution to cool. Use three times a day as compresses;
- Pour a tablespoon of dried chamomile (you can buy it at the pharmacy) with a glass of boiling water. Place in a water bath for seven minutes. The solution is used as a lotion. Soak gauze in the infusion and place it on the affected eye. Use three to five times a day. Leave the compress on for seven minutes.
| The treatment of chemosis must be approached comprehensively. Traditional medicine alone cannot get rid of severe pathology. Any “grandmother’s recipe” is allowed to be used after prior consultation with a doctor. |
Prevention
To prevent the development of chemosis it is necessary:
- Promptly treat eye inflammation, which can cause the development of chemosis.
- Protect your visual organs from excessive stress: give your eyes a rest when working on a computer for a long time, reading, driving a car, etc.
- Provide the body with a good night's rest, which will allow the eye tissues to fully recover overnight.
- If necessary, periodically take complex vitamins designed to restore the eyes.
- Include in your diet foods that help strengthen the conjunctival membrane - greens, fresh carrots, dark chocolate, blueberries, spinach.
If severe suppuration, swelling, redness and pain in the eyes occur, you should immediately consult an ophthalmologist. Ignoring symptoms that may indicate the development of chemosis can lead to loss of visual acuity and the development of serious complications.
Article Rating
Causes and possible diseases
Chemosis can be caused by severe irritation or inflammation of the conjunctiva or adjacent structures. The reasons for this can be completely different, for example, allergies (to pollen, pet dander, cosmetics) or infections.
In addition, orbital tumors can cause chemosis due to the accumulation of vessels in the conjunctiva. In contact lens wearers, swelling of the conjunctiva may be associated with incompatible lens care products. In addition, burns, trauma, and ultraviolet radiation can irritate the conjunctiva to such an extent that chemosis occurs.
Infectious conjunctivitis
It happens that the conjunctiva becomes inflamed without environmental influence. All external signs - swelling, redness, itching - indicate the occurrence of the disease. We can safely say that the nature of the onset of the disease is infection. It affects the eye due to the ingress of certain microorganisms. With infectious conjunctivitis, it may be painful for a person to move their eyes. The patient is bothered by a burning sensation and increased lacrimation, and possible discharge of purulent fluid from the conjunctiva. Symptoms may appear in different ways. In some cases, it is difficult for a person to even open his eyes.
What to do if you are worried about infectious conjunctivitis? Treatment usually involves local therapy. These are drugs against infections and microbes, eye drops. Preventive measures include careful adherence to hygiene rules, minimal use of cosmetics, especially for the visual organs, and the use of personal hygiene products.
Complications after the procedure
Like any surgical procedure, including similar ones, blepharoplasty may be associated with certain risks. Moreover, not only the patient’s face suffers, but also his moral state. After all, if an additional procedure is required, then this is already an inflated expense.
There are several reasons for the unsuccessful operation. First of all, this is the lack of qualifications and experience of the surgeon. At the same time, responsibility falls not only on the shoulders of doctors - a lot also depends on the patient himself. And if he does not follow the recommendations prescribed to him by a specialist, one should not be surprised at the rapid development of conjunctival chemosis.
This should also include the individual structural features of the patient’s eyelids.
What is conjunctival chemosis?
The conjunctival membrane covers the inside of the eyelids, as well as the eyeball. The part of the conjunctiva that covers the eye is called the bulbar. It consists of several layers, between which moisture accumulates during inflammation. Because of this, swelling is formed, which is pronounced and in some cases prevents the eyelids from completely closing. This symptom is accompanied by hemorrhages and redness of the conjunctiva. It often results from allergies, injury, or hormonal imbalances. However, there are other causes of this ophthalmological disease.
What is ocular chemosis?
While protecting the cornea, the conjunctiva itself is vulnerable to internal and external pathogenic factors. Inflammatory processes that arise under the influence of the latter sometimes cause swelling, which is called conjunctival chemosis.
The conjunctiva consists of two layers. The inner layer contains small vessels that supply the cornea with all the substances necessary for functioning. Under the influence of unfavorable factors or trauma, vascular permeability increases, and fluid enters the space between the layers of the conjunctiva, causing chemos. The swelling can be so severe that it begins to prevent the eyelids from closing completely.
Chemosis is not an independent disease. This is a symptom that accompanies many eye pathologies. It can be bilateral (affecting both eyes) or unilateral (affecting only one eye). Chemosis of the eye is not contagious. Both adults and children are susceptible to it. It can be one-time or periodic (chronic).
Chemosis in the moderate and severe stages causes a person great discomfort. Accompanied by irritation, itching, burning, and sometimes, with great development, the inability to close the eyes. The process can go so far that the swelling completely covers the cornea and protrudes from the palpebral fissure. In the worst case scenario, chemosis can lead to blindness. Therefore, at the first suspicion of it, you must consult a doctor for a detailed examination.
Diagnosis of the disease
The most important thing to do if you have any problems with your eyes is to consult a doctor and undergo appropriate diagnostics. This is the only way to accurately determine the type of pathology and begin treatment. And given that many eye diseases have similar symptoms, self-diagnosis and, moreover, self-medication are strictly prohibited.
The worst consequence that awaits those who like to experiment with their health and refuse qualified medical help is loss of vision and a deterioration in the quality of life many times over.
When diagnosing chemosis, it is important for the doctor to understand the reasons that caused it. Edema will never appear out of nowhere, and by eliminating what caused it, you can defeat the disease itself. So, to determine what caused the development of chemosis, the doctor will be helped by:
- ophthalmoscopy – examination of the fundus of the eye;
- biomicroscopy is one of the examination methods that involves studying the tissues and optical media of the eye, which is based on the contrast between unlit and illuminated areas;
- visometry – determination of the quality of vision and its acuity;
- measuring pressure inside the eyes.
Ophthalmoscopy Also, the patient should be referred for various laboratory tests. Based on the obtained indicators, the doctor will be able to judge the overall state of health, because it is very important to exclude other serious pathologies that could provoke chemosis.
Corneal edema
In addition to the inner shell of the eye, damage can also occur on the outside. This indicates the presence of serious eye pathologies. Damage to the cornea can significantly impair vision, so in no case should you delay going to the doctor if you have this symptom.
The cornea can become inflamed by viruses, bacteria or fungi. Regardless of the cause of the pathology, the external signs are similar to each other. The patient experiences unpleasant pain, is worried about the fear of light, and may experience watery eyes and itching of the eyes. In more advanced cases, difficulties arise in opening the eyes, sharp pain occurs when blinking, and the photo shows how the cornea swells greatly.
If the deep tissues of the cornea are damaged, first of all, visual acuity suffers. A person suddenly loses the clarity of images, everything around may become blurry. Small objects are also not visible, and fog often appears before the eyes.
Edema of the conjunctiva
The tarsal conjunctiva is characterized by a tight fit to the base, while the bulbar conjunctiva is loosely attached to it, therefore, if necessary, it is easily raised. The epithelium of the conjunctiva has a transition to the epithelium of the cornea; they are embryologically close. In newborns, subconjunctival tissue is not yet developed and develops later - during the first year of life. At the same time, lymphatic elements appear in loose connective tissue. The tarsal conjunctiva is slightly folded; when cut transversely, certain formations that appear to be glands are visible. Columnar stratified epithelium contains goblet cells. Under pathological conditions, the number of goblet cells can increase significantly. Circulatory disorders lead to obvious changes in the conjunctiva. And its swelling, redness or hemorrhages often serve as symptoms of local or general diseases.
Edema is characterized by manifestation mainly in the area of the conjunctiva of the eyeball or transitional fold. Sometimes the area of swelling of the conjunctiva of the eyeball, called chemosis, is so large that the conjunctival tissue completely covers the cornea and protrudes from the eye slit. The causes of conjunctival edema can be general and local pathological conditions. Often it is of an allergic or endocrine nature.
The causes of swelling of the conjunctiva of local localization include inflammation and congestion in the conjunctiva itself or its surroundings. Significant swelling, as a rule, occurs with severe conjunctivitis (for example, gonoblenorea), as well as inflammatory processes occurring in the areas surrounding the conjunctiva (for example, eyelid stye, orbital phlegmon, panophthalmitis), retrobulbar tumors. Instillation of any drugs into the conjunctival sac can cause chemosis. Chemosis of the conjunctiva is often accompanied by swelling of the eyelids.
Swelling of the conjunctiva may be limited or cover the conjunctiva of the eyeball completely. Under the edematous tissues with conjunctivitis, bacterial microflora and pus often accumulate, which contributes to ulceration of the cornea. Particularly common causes of conjunctival edema are panophthalmitis and retrobulbar tumor. Significant congestion and strangulation can lead to congestion in the conjunctival vessels. Conjunctival edema can also occur due to malignant exophthalmos.
In connection with all of the above problems, advice should be given to spend more time outdoors. Due to this, the organ of vision rests and the body strengthens. This is a very good prevention of all systemic pathologies. You can also try traditional eye care methods, including lotions and drops. At the same time, you should carefully monitor your health. At the first symptoms of eye color change, you should immediately make an appointment with a specialist and have an examination.
In the medical department, everyone can undergo examination using the most modern diagnostic equipment, and based on the results, receive advice from a highly qualified specialist. The clinic provides consultations to children from 4 years old. We are open seven days a week and work daily from 9 a.m. to 9 p.m. Our specialists will help identify the cause of vision loss and provide competent treatment for identified pathologies.
You can find out the cost of a particular procedure or make an appointment at the Moscow Eye Clinic by calling 8 and 8 (daily from 9:00 to 21:00) or using the online registration form.
Yakovleva Yulia Valerievna
Chemosis of the conjunctiva - causes and treatment
The tarsal conjunctiva is tightly attached to the base, and the bulbar conjunctiva is loosely attached to it, so it is easily raised if necessary. The epithelium of the conjunctiva smoothly passes into the epithelium of the cornea; embryologically they are close. As for the subconjunctival tissue, it is not yet developed in newborns and develops during the first year of life. At the same time, lymphatic elements appear in loose connective tissues. The tarsal conjunctiva shows some folding, and a transverse section reveals formations that appear to be glands. Stratified columnar epithelium contains goblet cells. Under pathological conditions, their number can increase significantly. With circulatory disorders, obvious changes appear on the conjunctiva. Hyperemia, hemorrhages and swelling can be signs of both local and general diseases.
Chemosis is swelling of the conjunctiva, which manifests itself mainly in the conjunctival region of the eyeball, as well as in the transitional fold. Sometimes chemosis reaches such a size that the conjunctival tissue covering the cornea protrudes from the palpebral fissure.
Chemosis can be caused by general and local factors. Chemosis can also be of an allergic or endocrine nature.
Local causes of chemosis include inflammation of the conjunctiva or surrounding tissues and congestive conditions. Significantly pronounced chemosis can develop with severe conjunctivitis, for example, with gonoblenorrhea; with inflammatory processes in the tissues surrounding the conjunctiva, for example, with styes, orbital phlegmon, panophthalmitis, with retrobulbar tumors.
Chemosis is often caused by instillation of certain drugs into the conjunctival sac. Edema of the eyelids is often accompanied by chemosis of the conjunctiva. In terms of prevalence, chemosis is limited or covers the entire conjunctiva of the eye. With conjunctivitis, the swollen conjunctiva becomes a reservoir of infection; bacteria and pus can accumulate under it, which contribute to ulceration of the cornea. Particularly common causes of chemosis are panophthalmitis and retrobulbar tumor. The result of significant stagnation and strangulation is congestion in the vessels of the conjunctiva. The onset of chemosis can provoke malignant exophthalmos.
In the medical department, everyone can undergo examination using the most modern diagnostic equipment, and based on the results, receive advice from a highly qualified specialist. The clinic is open seven days a week and operates daily from 9 a.m. to 9 p.m. Our specialists will help identify the cause of vision loss and provide competent treatment for identified pathologies.
You can make an appointment at the Moscow Eye Clinic by calling 8 8 (499) 322-36-36 (daily from 9:00 to 21:00) or using the online registration form.
Take care of your eyesight, it is very easy to lose and very difficult to restore! Fomenko Natalia Ivanovna
Treatment
The effectiveness of the course of treatment largely depends on the diagnosis performed. Only a high-quality and comprehensive examination of the visual organs will allow us to identify the causes of the pathology and prescribe one or another method of therapy. Chemosis can be overcome using two main methods - drug therapy or surgery.
If the disease is of moderate or mild complexity, then therapy can be carried out at home under the strict supervision of a doctor. However, if complications develop, which, however, is extremely rare, the patient is admitted to hospital.
As mentioned above, conjunctival chemosis is not a disease that can be ignored. In any case, if any discomfort in the eyes occurs, it is better to immediately contact an ophthalmologist - it would be better if this was an extra precaution. It is especially necessary to visit a doctor if there is a sharp decrease in vision, swelling and purulent discharge.
Diagnosis and treatment of chemosis
The treatment method depends on the nature of the disease. For allergic reactions, vasoconstrictors and antihistamines are used, viral chemosis is treated with antiviral drugs, antibiotics are prescribed in case of damage to the mucous membrane of the eyes by fungal pathogens. The dosage and combination of medications is determined by the attending physician after a thorough examination. In severe forms of the disease, for example, orbital tumors, exophthalmos, surgery may be required.
If the swelling of the conjunctiva is not eliminated in time, then purulent and inflammatory processes can spread to the cornea of the eye, which does not have external protection and does not have regenerative mechanisms. This can lead to inflammation of the cornea or keratitis, up to complete loss of vision.
Even with mild swelling of the mucous membrane, pain in the eye, pain, burning, we recommend that you consult your doctor as soon as possible for examination and treatment.
To diagnose the disease, a comprehensive ophthalmological examination is prescribed, which at the Eye Clinic of Dr. Belikova is carried out by experienced doctors of the highest and first category, Ph.D., as well as personally by Ph.D., Professor Elena Ivanovna Belikova. Health is in your hands, come and we will diagnose and help solve the problem.
Traditional medicine
Swelling can also be reduced with some traditional medicine. However, this cannot be called an independent treatment and therefore it is recommended to use them in combination as part of the main therapy. Proven recipes that our grandmothers used with success:
- Marshmallow root. For a glass of water (200 ml) take 3 tbsp. l. raw materials. Cooking time – 8 hours.
- Rosehip berries. Here, a glass of water requires 2 tsp. – boil for 5 minutes, then let it brew for half an hour. Make lotions.
- Cherries. This is a natural medicine against conjunctival chemosis, with which you can remove the inflammatory process. You can take it orally, make lotions from fresh berries, and rinse your eyes with diluted juice.
- Honey drops. Add 1 tsp to 0.5 liters of distilled water. this useful product in every sense. Place one drop in your eyes twice a day.
- Chamomile. A lotion is also made from this plant - 1 tbsp. l. raw materials are poured into a glass of boiling water. Prepare the composition in a water bath until it boils. After this, let it brew and use it for its intended purpose.
Traditional methods and various recipes work well against many diseases, including eye diseases. However, despite the obvious benefits, before using the recipes listed above, it is recommended to consult a specialist.
The fact is that even the most harmless products may contain allergens, which will further aggravate the situation.
Why does conjunctival chemosis occur?
Its most common causes are allergies and mechanical injuries. Also, swelling of the conjunctival membrane is caused by thermal and chemical burns of the eye, contact with a foreign object on the conjunctiva, and prolonged exposure to ultraviolet radiation on the organs of vision. Chemosis can be a sign or complication of certain eye diseases, including:
- conjunctivitis - an inflammatory process on the conjunctiva, provoked by an infection or fungus;
- blepharitis - inflammation of the edges of the eyelids caused by viruses, bacteria, fungi;
- meibomitis is an abscess on the eyelid that occurs due to inflammation of the sebaceous glands;
- eyelid abscess - purulent inflammation in a small area of the eyelid;
- exophthalmos - forward displacement of the eye;
- swelling in the orbital area;
- vascular diseases.
Main types of conjunctival edema
There is a classification of chemosis into: allergic, infectious
and
inflammatory
.
The allergic form of the disease can occur through self-medication, uncontrolled use of eye drops, or exposure to chemicals in the eye. It manifests itself as an acute condition, inflammation of the bulbar conjunctiva (the front surface of the eye), located on the eyeball. If treatment is not started in time, the disease can spread to the conjunctiva of the eyelids and affect both eyes. In this case, burning, itching, pain, stinging, lacrimation, sensation of a foreign body appear. It is difficult for the patient to close his eyes or blink.
Infectious purulent inflammation occurs when an abscess forms in different parts of the eyelid, for example, barley, as well as inflammation of the edges of the eyelids. The cause of inflammatory chemosis can also be damage to the sebaceous glands by mites of the genus Demodex.
Inflammation of the conjunctiva can accompany a systematic or acute disease. Chemosis is diagnosed in pathologies of the brain, blood vessels, venous stagnation of blood, endocrine diseases, tumors, displacement of the eyeball, exophthalmos, and skin tuberculosis. For diagnosis and treatment, we recommend that you contact a therapist or neurologist as soon as possible, who will prescribe a consultation with an ophthalmologist, who will decide on the choice of treatment methods.