The World Health Organization (WHO) recognizes that ophthalmology, in particular ophthalmic surgery, occupies a leading position among other branches of medicine in terms of such indicators as the degree of restoration of lost functions, minimally invasiveness, safety in terms of complications and side effects, reduction in the duration of intervention and terms rehabilitation. This high position has been achieved largely due to the use of laser technologies. Today, without a microsurgical or therapeutic laser, it is impossible to imagine a specialized ophthalmological center, or even a clinic office of a district ophthalmologist.
Laser techniques are successfully used to correct vision, stimulate visual functions, and treat various diseases of the visual organs, including such serious pathologies as glaucoma or chronically increased intraocular pressure syndrome.
The possibility of the finest, bloodless and seamless manipulation of the laser “needle” allows you to correct even quite gross defects and anomalies in the development of the drainage (fluid removal) system, without compromising the integrity of the walls of the eyeball. It is not surprising, therefore, that in world ophthalmological practice, laser therapy has long become one of the most effective, painless and preferred methods of treating glaucoma.
The first reports of the use of a coherent laser beam as part of complex therapy for glaucoma date back to the 70s of the last century. Today, models of argon, diode and solid-state Nd:YAG lasers specially developed for ophthalmology are used. In any case, however, a laser scalpel is used to correct the conditions of circulation of intraocular fluids - disturbances in their outflow are the direct cause of increased pressure inside the eye.
Both independent methods of laser therapy for glaucoma and auxiliary ones used in combination with drug and/or microsurgical treatment have been developed.
The use of a laser in this case has a number of significant advantages over other, earlier methods:
- the possibility of reconstructing the natural drainage tract without creating artificial, forced drainage of intraocular fluid;
- no need for general anesthesia - powerful local drip anesthesia provides reliable pain relief;
- no need for hospitalization: laser procedures are performed on an outpatient basis, “in one day”;
- reducing the cost of medical services;
- minimal invasiveness and trauma, which, in turn, minimizes the risks of side effects and complications typical for “conventional” surgery;
- significant reduction in the period of postoperative rehabilitation.
According to the nature of the effect, optical generators used in the treatment of glaucoma can be divided into coagulator lasers (instant cauterization, “fusion” of a local area) and destructor lasers (micro-explosion in excess tissue with the aim of destroying it with a shock wave and restoring the natural anatomy of the eye structures).
Of the numerous methods and techniques of laser surgical intervention developed at different times, laser iridectomy (iridotomy) and laser trabeculoplasty have received primary practical implementation.
Important information about glaucoma
Translated from Greek, “glaucoma” is translated as “green color of the sea.” People usually start talking about glaucoma if a person experiences a persistent increase in intraocular pressure. This is due to stagnation of intraocular fluid, which can lead to destruction of the optic nerve.
Impaired outflow of aqueous fluid from the eyeball causes congestion and increased pressure in the eye. As a result, this leads not only to decreased vision, but often to its complete loss.
Ophthalmologists consider such visual pathology to be insidious: the symptoms of the disease can appear quite late. Typically, at an early stage, glaucoma has no symptoms at all.
Most often, patients begin to turn to ophthalmologists only when their vision begins to seriously suffer.
Symptoms
The key symptoms of glaucoma are:
- blurred vision;
- the appearance of rainbow circles near light sources (light bulbs, headlights, candles, etc.)
When the patient begins to notice redness of the eyes and attacks of eye pain, this indicates that the pathology has entered the terminal or final stage, when it is no longer possible to cure.
Although you can get glaucoma at any age, this pathology is more common in older people.
The main symptom of glaucoma is increased intraocular pressure (or pressure with a difference in both eyes above 5 mmHg)
However, in addition to this feature, in patients with glaucoma, the boundaries of the visual field are disrupted and the fibers of the optic nerve are damaged. Therefore, with the development of this pathology, specialists also identify organic disorders in the structure of the eye (optic disc atrophy, disorders of ocular hydrodynamics, etc.)
The concept of “glaucoma” includes about 60 diseases that have a number of features such as:
- increased intraocular pressure;
- glaucomatous optic neuropathy (damage to the optic nerve) with its subsequent atrophy;
- visual impairment.
The main risk factors for the development of glaucoma are situations with:
- aggravated heredity;
- old age (over 65 years);
- anatomical features of the eyes.
Diagnosis of glaucoma
Moderate intraocular hypertension is quite difficult to notice. To determine the increase in pressure, special tonometry devices are used. Pressure can be measured by contact or non-contact using pneumotonometers.
When the fibers of the optic nerve are damaged, a gradual narrowing of the boundaries of the visual field occurs. Such changes can be determined by perimetry, which is mandatory for all patients with suspected glaucoma. Sometimes patients can independently notice impairment of peripheral vision, but this is rare and usually occurs with significant changes in advanced disease.
With biomicroscopy of the anterior chamber of the eyeball, the doctor can detect changes characteristic of glaucoma. To visualize the anterior chamber angle, gonioscopy must be performed. In this case, you can quite clearly assess its condition, shape and other parameters.
During ophthalmoscopy, the doctor assesses the condition of the fundus structures (vessels, retina, optic nerve). This study is performed by the contact method using a special lens attached to the cornea, or non-contactly, when the image is formed using magnifying lenses and an ophthalmoscope.
Modern ophthalmologists have a large number of high-tech techniques that can be used to diagnose glaucoma. These include Heidelberg retinal tomography and optical coherence tomography. These methods accurately determine the thickness of nerve fibers in the optic nerve head, excavation and other indicators. These data are very important in diagnosing glaucoma, and are also used to assess the dynamics of the condition during treatment.
Ultrasound biomicroscopy helps to identify changes in the structures of the eye and evaluate the outflow pathways of intraocular fluid. It is important to pay attention to the size and ratio of the main intraocular structures, which are not accessible to conventional ophthalmoscopy.
MORE ABOUT DIAGNOSTIC METHODS >>>
Forms and types
Glaucoma is called primary if it occurs independently, or secondary if the pathology appears as the consequences of various disorders that change the condition of the vessels and the movement of blood in them.
Diseases in a patient such as:
- myopia;
- cardiovascular pathologies;
- persistent hypertension or hypotension;
- migraine;
- diabetes mellitus
The main forms of glaucoma are:
- Open angle. The most common form, in which the function of the drainage system of the eyes is disrupted and eye pressure increases. It is often asymptomatic and quickly leads to blindness.
- Closed angle. A less common form in which intraocular fluid cannot enter the drainage system. This form has more pronounced manifestations in the form of pain, redness of the eyes and severe visual disturbances.
Laser iridectomy (iridotomy)
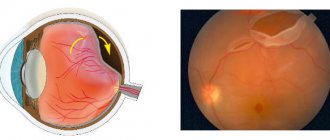
The essence of the method is to create a small duct in the peripheral zone of the iris, due to which the angle of the anterior chamber of the eye opens and the pressure in the posterior and anterior ocular chambers is equalized.
The main indications for laser iridectomy are:
- narrow- and closed-angle forms of glaucoma (both primary and secondary) with a functional block of the pupil;
- the need to prevent acute glaucomatous attacks with positive stress tests;
- irregular (flat) shape of the surface of the iris;
- iridovitreal block.
The danger of glaucoma
Glaucoma can occur with more or less pronounced manifestations, but is always accompanied by a periodic or constant increase in intraocular pressure.
During an attack, the pupil dilates, loses mobility and acquires a greenish color (which is why this disease is also called “green cataract”).
The disease, if left untreated, results in complete loss of vision. It is in the rapid progression that the insidiousness of glaucoma lies.
Blindness due to glaucoma is associated with the destruction of retinal cells caused by high blood pressure, a disorder of the circulation of intraocular fluid and atrophy of the optic nerve. The damaged optic nerve stops transmitting visual signals to the brain normally. In a person with this condition, central and peripheral vision suffers, and the visual area gradually decreases.
Glaucoma Treatment Methods
Treatment of glaucoma is long and difficult. The choice of treatment method is determined by the doctor depending on the type of glaucoma, its course, and the patient’s health condition. The main ways to eliminate this eye pathology are treatment methods:
- conservative (medication);
- surgical;
- laser
- Drug treatment consists of instilling drops that reduce intraocular pressure. You have to use drops for life; in patients, instilling drops becomes as common a procedure as brushing your teeth. However, the drugs have many contraindications and are not always suitable for patients with serious concomitant diseases such as asthma or vascular pathologies.
- Surgery is used as a last resort when other methods are ineffective. Modern surgical techniques prefer gentle intervention, without perforation of the eyeball (non-penetrating sclerectomy). The surgical method is especially effective in the early stages of the pathology, as it stops its development, preventing the occurrence of atrophy of the optic nerve fibers. There are several methods of such operations. The most popular EX-PRESS technique uses a special valve made of medical steel to drain intraocular fluid. This treatment is well accepted by the patient’s body, and already on the day of surgery, most of them are already discharged home.
- Laser therapy for glaucoma has been used since the 70s of the last century and is excellent for those patients for whom the use of medications is not enough. We will analyze the essence of the laser method of treating glaucoma in detail.
Glaucoma
Glaucoma is a fairly common disease. It mainly affects people over 40 years of age. But this disease can affect young people and even newborns. Today, ophthalmology knows only one way to prevent blindness from glaucoma - timely recognition and proper treatment. MORE DETAILS
Thanks to modern treatment methods, most patients manage to maintain their vision and joy in perceiving the world around them.
DIAGNOSIS OF GLAUCOMA
Heredity plays an important role in the occurrence of glaucoma. If your relatives have had glaucoma, you need to be especially vigilant and regularly be examined by an ophthalmologist. Please note that people suffering from diabetes, hypertension and atherosclerosis are more likely to suffer from glaucoma. Therefore, in addition to regularly visiting a therapist or endocrinologist, they should be examined by an ophthalmologist at least twice a year.
Remember! Every person needs to be examined by an ophthalmologist at least once a year.
TREATMENT
With glaucoma, patients need systematic and long-term treatment, always under the supervision of a doctor. As a rule, treatment begins with the use of medications: drops are instilled into the eyes to reduce intraocular pressure; take tablets that improve nutrition of the optic nerve and retina. In some, unfortunately, rare cases, with this treatment, intraocular pressure becomes normal, and the condition of the optic nerve does not worsen. In such a situation, drug treatment is sufficient, although the drugs will have to be used for life.
Therefore, specialists have developed qualitatively new methods for treating glaucoma: effective, safe and low-traumatic. These include laser surgery and surgery.
In the first case, the laser beam, freely penetrating the eye, affects the drainage system and improves the outflow of intraocular fluid. Laser treatment is painless, short in duration, and performed on an outpatient basis. Its significant advantage is that the eyeball is not subjected to surgery.
Unfortunately, not all glaucoma patients can benefit from a laser beam. Such treatment can be effective only in the initial stages of the disease, when intraocular pressure is slightly increased, as well as during attacks of glaucoma, described earlier. For the vast majority of people suffering from this disease, the most effective treatment is surgery.
According to experts, glaucoma should be diagnosed and treated surgically much earlier than is currently the case. It has been proven that the use of traditional medicines often not only does not help, but also has a negative effect on the eye. The most common drugs that lower intraocular pressure reduce the production of intraocular fluid. This leads to disruption of nutrition of all eye structures and increases dystrophic changes in the optic nerve and retina. Surgery to create a new outflow pathway for intraocular fluid, performed as early as possible, will preserve vision in patients with glaucoma.
This operation is called “non-penetrating deep sclerectomy.” It can be successfully used for any form of open-angle glaucoma. The most important advantage of the operation is that it is performed without opening the eyeball. This eliminates the possibility of infection and significantly reduces the risk of complications during surgery.
Non-penetrating deep sclerectomy is performed under local anesthesia, instillation of drops with the obligatory participation of anesthesiologists who will prepare you for surgery and help relieve nervous tension. To carry it out, an excimer laser and special microsurgical instruments with blades made of diamond, sapphire and other high-strength materials are used. The duration of the operation is on average 15-20 minutes.
| The operation is performed for various types of primary, congenital and secondary glaucoma in eyes with preserved visual functions (presence of visual fields) | The total treatment time for one eye is 10 days (preoperative examination 2-3 days, surgery on the 4th day). |
In addition to non-penetrating deep sclerectomy, according to indications, other types of antiglaucomatous operations are used, developed in the leading ophthalmological clinics of the world and widely used in the Eye Microsurgery International Scientific and Technical Center.
If, in addition to glaucoma, you are also diagnosed with cataracts, then you need surgical treatment, which consists of performing a non-penetrating deep sclerectomy and removing the cataract and replacing the clouded lens with an artificial, reliable and perfect one. Depending on the indications, interventions are performed alternately or simultaneously.
After surgery, you will need to take anti-inflammatory drops, so you need to purchase them in advance, following your doctor's recommendations.
After 9–14 days, if the instructions are followed correctly, the redness of the operated eye will disappear. You will be able to calmly look at the light, lacrimation and the sensation of a foreign body in the eye will not bother you.
If the operation is performed in a timely manner, it normalizes intraocular pressure and preserves vision.
In the future, we recommend that you regularly, 2-3 times a year, visit an ophthalmologist to check visual acuity and control intraocular pressure, since the progression of disorders in the vascular and drainage systems of the eye, as well as excessive scarring in the area of the anti-glaucomatous surgery, can again lead to an increase in IOP in a small percentage of cases (1.5-2.2%). An ophthalmologist can determine the reason for the lack of effectiveness of the operation and carry out the necessary treatment.
A number of new treatment methods have been developed, also aimed at preserving the vision of patients with glaucoma. These include: magnetic and laser stimulation of the optic nerve, which improves vision especially with advanced glaucoma, as well as vasoreconstructive surgery. This operation is performed strictly according to indications for patients with impaired blood supply to the eye, which, unfortunately, often occurs even with normal intraocular pressure. As a result of a simple surgical intervention, more blood carrying nutrients will flow to the eye.
Laser treatment of glaucoma
The widespread use of lasers to combat glaucoma began in the 70s of the last century. Currently, laser treatment of glaucoma has rightfully established itself throughout the world as the most effective and safe method. In this case, treatment of glaucoma with a laser can be performed as an independent method of treating glaucoma, or in combination with microsurgical anti-glaucoma surgery.
Benefits of laser treatment for glaucoma:
- restoration of the outflow of intraocular fluid from the eye through natural pathways;
- high efficiency in reducing intraocular pressure;
- minimal risk of complications;
- laser interventions are painless and are performed under local anesthesia by instilling anesthetic drops;
- laser treatment is short-term and performed on an outpatient basis;
- short, short period of recovery (rehabilitation).
Laser treatment of glaucoma is most effective in the early stages of the disease.
Depending on the type of glaucoma - open-angle or closed-angle, the nature of changes in the drainage apparatus of the eye, various types of laser interventions (surgeries) are used. Laser treatment is carried out using the most modern original technologies developed at the Eye Microsurgery MNTK and advanced, innovative techniques used in world practice. Our specialists use the most modern equipment, the latest laser installations, allowing us to carry out a wide range of laser interventions for the effective treatment of glaucoma.
Specialists at the Eye Microsurgery Center will select the optimal glaucoma treatment method for you, which will allow you to preserve your vision and restore the joy of life.
Patient Reminder
Your doctors
Laser surgery for glaucoma
The laser is most effective at the beginning of the development of pathology, and this method is least effective in the advanced stage of glaucoma.
Laser treatment for glaucoma can be carried out by several types of laser units with different characteristics and parameters. For this purpose, technologies of this type of treatment are used in the form of:
- The technique of laser iridectomy and goniotomy, which involves artificially creating a hole for the outflow of intraocular fluid in the iris. A through hole in the iris leads to pressure equalization between the anterior and posterior chambers of the eye.
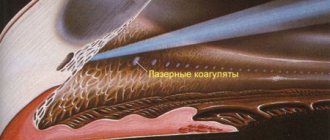
- Laser trabeculoplasty, used for open-angle glaucoma to restore the movement of intraocular fluid. With this technique, tiny burns are applied to the diaphragm, which leads to the expansion of the narrowed canal and improved outflow of intraocular fluid.
- Laser gonioplasty, which involves coagulation of the iris using an argon laser.
- Laser trabeculopuncture, the essence of which is to create slits in the scleral flap for the operation of the anterior chamber, used for complicated glaucoma.
- Laser descemengoniopuncture, used in the treatment of uncompensated glaucoma, allowing to supplement or replace the constant use of medications.
A variety of laser techniques allows the ophthalmic surgeon to select the most suitable treatment method for a given type of glaucoma. Laser correction can serve as an independent type of treatment, or be part of complex therapy and performed before microsurgical intervention.
Often, laser surgery alone is not enough to restore the outflow of intraocular fluid. Lack of retinal nutrition leads to atrophy of its light-receiving cells, even if intraocular pressure has been normalized. Therefore, to restore vision and prevent its deterioration, methods are used to improve the blood supply to the retina. The following methods can be used to improve blood circulation:
- laser stimulation;
- vacuum massage;
- magnetic therapy;
- ultrasound therapy;
- electrical stimulation.
Sometimes conservative methods are not enough, and to fully save vision, vasoreconstructive operations are used to redistribute blood flow and increase blood supply.
Types of surgeries for the treatment of glaucoma
The price of surgery for the treatment of glaucoma depends on the method of its implementation. Modern surgical ophthalmology has a wide range of techniques to treat this disease. In accordance with the objectives of the conduct, they are divided into four groups:
| Group | Indications for use | Methods used |
| Operations aimed at providing optimal conditions for the circulation of intraocular fluid | Primary/secondary angle-closure glaucoma. |
|
| Operations aimed at creating new pathways for the outflow of intraocular fluid from the anterior chamber - fistulizing operations |
| Trabeculectomy - requires an incision of the conjunctiva, partial separation of the fibrous plate in order to create a path for the outflow of EVs into the subconjunctival space, where it can be absorbed into the vessels. |
| Non-penetrating fistulizing surgeries that do not require opening the anterior chamber |
| Non-perforating deep sclerectomy involves excision of the outer wall and ensuring the outflow of EVs into the subconjunctival space or capillaries of the ciliary body. The operation can be penetrating or non-penetrating. |
| Cyclodestructive operations |
| Cyclocryodestruction and cyclocryocoagulation, which are aimed at damage and atrophy of parts of the ciliary muscle in order to reduce the production of intraocular fluid. |
Indications for laser therapy for glaucoma
The main indications for the use of laser therapy for glaucoma are situations related to:
- contraindications of drugs to reduce intraocular pressure;
- the impossibility of systematic drug treatment for this disease;
- the need to use a large number of medications to reduce intraocular pressure;
- ineffectiveness of long-term conservative treatment;
- a sharp decrease in vision or narrowing of the field of view;
- prevention of acute attacks of glaucoma.
Glaucoma surgery
The operation is effective – and vital! – a way to reduce intraocular pressure, if it was not possible to cope with this task in any other way. When inviting the patient to take this step, the doctor takes into account not only the level of intraocular pressure, but also the progression of glaucoma (the condition of the retina and optic nerve) from the moment of diagnosis. Surgeries are prescribed only in case of negative dynamics of the eye condition (even if the patient does not yet complain about the level of visual functions!).
There are a number of different surgeries for glaucoma. All of them involve the creation of drainages to drain excess intraocular fluid from the eye. Thanks to this, it is possible to quickly and, as a rule, permanently reduce intraocular pressure. Excess eye fluid has a negative effect on the optic nerve and retina. By getting rid of it, we rid the eye of this negative factor.
In many cases, after surgery, the patient no longer needs to instill drops for a long time. Or the number of drugs needed can be reduced.
Benefits of laser treatment
The laser is especially useful to use at the initial stage of the onset of this disease. Laser techniques make it possible to ensure normal outflow of intraocular fluid in a short time.
However, in advanced stages of the disease, laser treatment may be ineffective. However, there are situations where even advanced stages of glaucoma have been successfully treated with laser.
The benefits of laser treatment for glaucoma are associated with:
- minimal trauma to eye tissue during treatment;
- low cost;
- the ability to carry out treatment on both eyes in one day on an outpatient basis;
- minimum postoperative complications;
- the possibility of repeated laser procedures;
- painlessness;
- minimal rehabilitation period;
- carrying out treatment without the need to open the eye cavity and damage the eye membranes.
All laser techniques involve creating an artificial tunnel for the exit of intraocular fluid, as well as its thinning or expansion. An effectively selected technique allows you to stabilize intraocular pressure and eliminate the need for constant use of medications.
Laser treatment cannot restore vision, but this method can prevent the progression of the disease.
Laser selective trabeculoplasty
This type of operation is successfully used in patients with open-angle glaucoma, when conservative therapy is ineffective, and the point of the operation is the selective effect of the laser on the entire trabecular area. This is one of the latest modifications of argon laser surgery.
Its advantage lies in the expanded area of influence, because argon laser technology involves only the projection zone of Schlemm’s canal, while selective trabeculoplasty covers the entire area of the trabecula.
Selective trabeculoplasty is also performed on an outpatient basis under local anesthesia. A three-mirror goniolens is installed on the affected eye, which focuses the laser beams in the required area.
Laser beams selectively apply a series of burns to the trabecular area. As a result, reactive shortening and tension of the trabecular diaphragm occurs where burns form on the tissue; the trabecular slits located between the burns are thus stretched, and this phenomenon leads to improved outflow of intraocular fluid.
Another advantage of selective trabeculoplasty over argon laser technology is the absence of thermal damage to trabecular tissue and coagulation necrosis of cells and collagen fibers in this area, since the impact of the pulse is very short-term.
Pigment-free cells of the trabecular zone remain intact due to the selective action of the laser only on cells containing melanin. Trabecular cells are not exposed to burn damage, and intraocular pressure is effectively reduced.
Like laser iridectomy, selective trabeculoplasty is sometimes complemented by surgical treatment, and in other cases is acceptable as an independent method of treating glaucoma. Indications for the latter:
- glaucoma in the initial and advanced stages with subcompensation of intraocular pressure, if the trabecular zone of the anterior chamber angle is moderately or severely pigmented;
- pre-conducted argon laser therapy did not give the result that was expected from it;
- the feasibility of laser treatment of patients with pigmentary and pseudoexfoliative glaucoma.
Restoration of the normal outflow of intraocular fluid, and as a consequence, a decrease in intraocular pressure, occurs by the end of the first day after selective trabeculoplasty.
This operation is recognized as the most effective and at the same time gentle compared to the argon laser method, provides a more pronounced and lasting hypotensive effect, and also gives a positive result in cases where argon laser surgery was ineffective.
However, the patient should also be familiar with the disadvantages of laser treatment for glaucoma, which should not be forgotten:
- Possibility of formation of scar adhesions in the area of laser exposure.
- Risk of concomitant damage to corneal endothelial cells, iris vessels or lens capsule.
- The possibility of the formation of a reactive syndrome, expressed in increased intraocular pressure and, subsequently, an inflammatory process.
- Low effectiveness of treatment in advanced cases of the disease.
The above should be summarized in words that can be both a conclusion and a reminder: it is necessary to begin treatment for glaucoma as soon as possible after diagnosis.
Trust your health to the doctors of the medical center named after. Svyatoslav Fedorov, and your vision will thank you!
Flaws
Like any treatment method, the use of laser has disadvantages. The main one is the frequent fragility of the effect of laser correction and the need to re-use this technique. To maintain the effect of laser use, patients often have to use a number of medications.
Other disadvantages of laser treatment are related to:
- instability of the therapeutic effect and its ability to fade over time;
- the possibility of inflammation;
- sharp jumps in intraocular pressure in the first days after the intervention;
- constant lacrimation;
- in some cases, the possibility of damage to the lens of the eye or the walls of blood vessels;
- postoperative fusions at the site of laser exposure.
In some cases, laser treatment of glaucoma becomes ineffective, and then surgery has to be resorted to.
How to prepare for glaucoma surgery?
In order to eliminate contraindications and perform surgery to treat glaucoma successfully, the attending physician prescribes a comprehensive diagnostic test for the patient, which includes the following:
| Techniques | What is it for? |
| Daily tonometry | Determination of intraocular pressure during the day. |
| B-scanning with a sufficient level of transparency of optical media | Ultrasound examination to identify affected ocular structures |
| Gonioscopy | Study of the structure of the angle of the anterior ocular chamber and the trabecular meshwork to determine surgical tactics. |
| Direct ophthalmoscopy | Determination of the integrity of the retina and optic nerve head. |
| Biomicroscopy | Determination of the condition of the cornea, identification of its dystrophic changes. |
| Electronic tonography | Auxiliary measurement of intraocular pressure and determination of the circulation of aqueous humor in the eye. |
| OCT | It is performed when there is insufficient transparency of the cornea or vitreous body, which makes it difficult to use other diagnostic techniques. |
| Laboratory tests of blood and urine | To determine the general condition of the patient. |
In order to exclude the presence of inflammatory and infectious processes, before surgery you need to visit the following specialists:
- ENT;
- dentist;
- therapist.
Contraindications to laser treatment
Laser treatment may not be suitable for all patients with glaucoma. Laser therapy should not be used in the following situations:
- under 18 years of age;
- complete loss of vision in one eye;
- glaucoma in closed-angle form;
- pregnancy or breastfeeding;
- viral eye diseases;
- autoimmune diseases;
- high degree of corneal opacification.
Advantages of glaucoma treatment at the Sfera clinic
Specialists at Professor Eskina’s clinic have been studying, diagnosing and treating visual impairments in adults and children for more than twenty years. Therefore, by contacting us, you are in the safe hands of experienced ophthalmologists who have been certified and work in accordance with international standards.
We have a wide range of diagnostic equipment and modern laser systems for glaucoma treatment. The selection of the surgical technique is carried out individually, based on the patient’s indications. You can find out the cost of surgery for the treatment of glaucoma in the corresponding section of our official website or by calling us by phone.
Preoperative preparation
It is important to comply with a number of conditions.
- Laser treatment is painless; you may feel a slight tingling sensation or light “clicks” in the eye area. The session lasts, depending on the surgical technique, from 5 to 60 minutes.
- Drinking alcohol is prohibited 2 days before treatment. It is also advisable to stop smoking on the day of surgery.
- On the day before the intervention, it is recommended to wash your hair and face and avoid the use of cosmetics (perfumes, deodorants, etc.)
- It is important to have identification documents with you (passport, insurance policy, medical card, research results).
- It is better to dress before surgery in a cotton T-shirt, blouse or wide-neck shirt. It is also important to have replacement shoes.
- A light breakfast is allowed on the day of surgery. You should also bring sunglasses with you.
Typically, medications are used before and after surgery: non-steroidal anti-inflammatory drugs, local painkillers, drugs to reduce intraocular pressure.
In case of severe pain syndrome in patients, local anesthesia (retrobulbar) can be used.
Cost of laser correction
Laser correction for glaucoma is performed in many clinics or medical centers. Most often, for this type of treatment, patients prefer to go to Fedorov’s clinic or its branches, located in 12 cities of Russia.
How much does laser treatment for glaucoma cost? The cost of the intervention depends on the level of the clinic, the city, the patient’s health condition, the chosen laser correction technique, and the complexity of the diagnosis.
The average cost of laser correction in Moscow is:
- from 12,500 to 17,500 rubles for keratectomy;
- from 12,000 rubles for laser iridectomy;
- from 13,000 rubles for laser trabeculoplasty;
- from 22,500 to 45,500 rubles for different types of LASIK surgery;
- from 65,500 rubles for combined treatment of glaucoma and cataracts.
Additionally, patients often have to pay for diagnostic tests or the use of medications during therapy, which will increase the overall cost of treatment.
Postoperative period
The recovery time after surgery depends on how it was performed. As already mentioned, laser techniques are more gentle, and therefore the recovery period is shorter. In any case, after surgery it is necessary:
- stay in bed for one or two days;
- follow your doctor’s recommendations regarding the use of anti-inflammatory and antibacterial drops;
- wear bandages;
- limit fluid intake to one liter per day;
- take measures to prevent constipation;
- eliminate the consumption of alcoholic beverages, strong coffee and tea;
- Avoid prolonged exposure to poor lighting conditions.
Reviews
Lilia, 62 years old
I was diagnosed with glaucoma and was offered to treat it with a laser. To my surprise, the effect of the operation on one eye was 100%. I am also going to treat the second eye.
Igor, 48 years old
Suddenly I was diagnosed with glaucoma. I was advised not to waste time on eye drops, but to undergo laser treatment. The effect of this treatment is simply excellent, and recovery takes place in the shortest possible time.
Irina, 41 years old
After laser treatment, my eyes stopped bothering me at all, and my vision became better than in my youth.
Glaucoma is a very insidious pathology prone to progression. The advanced stage of this disease often leads to blindness. The many advantages of laser correction prove the right of this method of therapy to exist and the need for further development.
However, one cannot fail to take into account that the best results are obtained by laser treatment in the initial stage of the pathology. Therefore, it is unacceptable to ignore any problems in eye health, as well as skip annual preventive examinations with an ophthalmologist.
Sources used:
- Primary glaucoma in patients with myopia and hypertension / Elena Baudova. - M.: LAP Lambert Academic Publishing, 2011.
- Diagnostic reference book for an ophthalmologist / P.A. Bezdetko, S.F. Zubarev, N.V. Panchenko. - M.: Phoenix, 2006.
- Ophthalmoscopy / Yu.S. Astakhov, N.Yu. Dahl. - M.: N-L, 2011.
- IU School of Medicine Department of Ophthalmology
Transscleral laser cyclocoagulation
In this case, laser treatment of glaucoma consists of thermal destruction of part of the ciliary body in order to reduce the production of aqueous humor and intraocular pressure.
Indications for this laser treatment method:
- primary glaucoma in an advanced stage, not amenable to traditional treatment methods,
- terminal glaucoma with pain syndrome that cannot be controlled by traditional methods of treatment,
- vascular ophthalmic hypertension and glaucoma, regardless of the stage of the process (post-thrombotic after acute obstruction of the central retinal vein, neovascular after acute occlusion of the central retinal artery, hemorrhagic after recurrent hemophthalmos),
- diabetic neovascular degenerative glaucoma,
- post-traumatic glaucoma and ophthalmic hypertension (including post-burn).