The retina is the tissue of the fundus of the eye, evolutionarily specialized to perform one single function: to receive an image focused by the optics of the eye and transmit it to the optic nerve, which, in turn, is a conductor to the analytical centers of the occipital cortex. The visual image we are accustomed to is built there. As is known, the image arrives on the retina inverted by 180° and, moreover, monoscopic, flat; to recreate a binocular three-dimensional image from signals received simultaneously from two eyes is the task of the central nervous system.
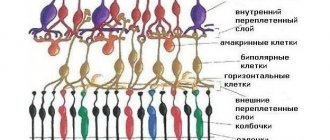
The retinal (retinal) neuroepithelium consists of several microscopic layers of special cells - cones and rods - containing light-sensitive pigment and especially densely concentrated in the central or macular region of the retina (the “macula” area). Like other highly specialized tissues, the retinal layer is very vulnerable to any negative influences; any damage or unfavorable operating conditions automatically result in a serious problem for the visual system as a whole. The life support of the retina, that is, nutrition and oxygenation, is carried out with the flow of blood, which enters through the choroid associated with the retina. The term “retinal detachment,” familiar to many, means a violation of its organic connection with the choroid, separation from the nutritional system - which leads to the most detrimental consequences, including loss of vision as such.
Causes of retinal detachment
The main cause of retinal detachment is retinal breaks. Such damage can be caused by:
- Prolonged inflammation of the iris or choroid.
- Severe myopia.
- Atrophic changes in the fundus of the eye.
- Injuries to the visual organ.
- Physical activity - jumping from heights or lifting weights.
- Other systemic diseases - diabetes mellitus, hemorrhages and various neoplasms in the eye.
Retinal detachment is not always diagnosed in a timely manner, since at first the symptoms may not be very pronounced. You should be wary of:
- Deterioration in the quality of vision.
- Deterioration of lateral vision.
- Flashing spots, flies and veils before the eyes.
- Fluctuation of objects around and their blurriness.
In many cases, patients note that their vision improves after waking up. This happens because the retina in a horizontal position fits in the right place, and when it takes a vertical position, it moves away again and all the symptoms appear again.
Retinal ruptures occur during retinal dystrophy. Large ruptures are observed with serious eye injuries.
How to understand that detachment has begun?
The following symptoms may indicate retinal detachment:
- Dark areas, cobwebs. Their location in front of the eyes is a projection of the detachment zones.
- Flickering, lightning before the eyes.
- Ring-shaped opacities.
- Distorted perception of the shape and size of visible objects.
- Deterioration of visual acuity.
- Fog or white veil before the eyes.
- Sudden loss or deterioration of lateral visibility.
Detachment is an insidious pathology because it is painless. Because of this, patients often consult a doctor at a late stage, when it is much more difficult to save their vision. Therefore, it is very important to be attentive to any ophthalmic symptoms. And if you notice at least one of the above, be sure to consult a doctor. Remember that the likelihood of avoiding blindness is much higher for those who start treatment on time.
Indications for surgery
It must be remembered that it is impossible to cure retinal detachment with drops, injections or physiotherapeutic procedures. In this case, only surgery can help. Moreover, the sooner it is done, the greater the chance a person has of maintaining his vision.
Only an ophthalmologist can make a correct diagnosis. This requires a series of examinations. The visual field is determined, the fundus and internal structures of the eyeball are examined. In addition, optical coherence tomography of the retina is performed.
Indications for surgical intervention are all characteristic symptoms of detachment, as well as a confirmed diagnosis during the examination. If a pregnant woman experiences retinal detachment, spontaneous childbirth is impossible.
Scleral filling
When sealing the sclera, manipulations are performed extrascleral. In this case, the retinal layers are brought closer together due to external indentation. In the area of the retinal tear, a special filling is placed and sewn onto the sclera, which is a strip of silicone with specified parameters.
As a result, the sclera itself, the choroid, and other tissues located under the filling descend closer to the fundus of the eye. The forming shaft blocks the gap. The liquid located under the detachment area resolves over time.
Seals can be placed in sectors, circles or radii. The specific location depends on the shape and location of the retinal break.
Sometimes the doctor applies a so-called cerclage. In this case, the sclera is pressed along the equator of the eyeball using braid or thread. If a lot of fluid has accumulated between the layers of the retina, you can remove it with a needle through a puncture.
Types of operations
Treatment for retinal detachment can be surgery or laser. The latter type of treatment is more preferable, as it is less traumatic. Laser treatment in most cases does not require hospitalization of the patient. The patient spends no more than 2-3 hours in the clinic.
Laser coagulation
During laser treatment, the areas treated with a laser beam are soldered to the vascular film. This is due to the high temperature at which the tissues coagulate. This treatment is completely bloodless, the patient feels only a light touch to the mucous membrane and observes glare. The operation is carried out in several successive stages:
- An anesthetic drug is dripped into the patient's eye, this prevents discomfort.
- A special lens is installed on the visual organ, which helps localize the laser beams.
- Coagulants are applied to the retina of the eye, and adhesions are then formed in their place.
The entire course of the operation is controlled by a microsurgeon through a special microscope. Typically, surgery on one eye lasts no more than 20 minutes. All manipulations are performed with the patient sitting.
Laser surgery is well tolerated by children. Unpleasant sensations after surgery disappear in just a day.
Extrascleral filling
Even during the diagnostic process, the location, size and shape of the problem area of the retina are determined. Taking this data into account, a specific filling is made from spongy silicone. The doctor cuts the conjunctiva, through this incision the filling is placed on the sclera and secured with sutures. To correctly place such a filling, sometimes an expanding gas or air is injected into the eye.
If there is an accumulation of intraocular fluid in the eye, then at the final stage of the operation it is removed. Only after this the conjunctiva is sutured.
After such an operation, vision is not restored immediately, but after a couple of months. For some patients, the recovery period lasts up to six months. And if the detachment was caused by myopia, then the process of complete recovery is even more delayed.
The effectiveness of such treatment is partial, since complete restoration of vision after surgery is not observed.
Vitrectomy
This is a surgical procedure that is used to treat a number of ophthalmological diseases. During the operation, scars, blood and pathologically altered tissues are removed from the vitreous. The vacated space is replaced with a saline solution or special polymers. These substances expand, due to which the retina is pressed tightly against the choroid from the inside.
Most often, the operation is performed under local anesthesia and general anesthesia. Hospitalization is not required, the operation lasts about an hour, the patient does not experience any discomfort.
Ballooning of the sclera
This operation is indicated for uncomplicated retinal detachment. Ballooning is performed on the surface of the sclera. The goal of such treatment is to ensure a tight fit of the retina to the choroid.
The operation consists of inserting a special balloon with a catheter behind the eye. As the pressure in the balloon gradually increases, it increases in size and puts pressure on the sclera.
After the balloon is in place, it is strengthened using a laser beam. The canister is removed approximately a week after laser treatment. This operation is considered low-traumatic and effective; it lasts no more than an hour.
With timely ballooning of the sclera, the effectiveness of treatment reaches 98%.
Possibilities of endovitreal surgery
As one of the newest high-tech areas of eye surgery, endovitreal surgery appeared in the middle of the last century. It involves performing a vitrectomy - removing the pathologically altered vitreous body and the resulting scar tissue from the surface of the retina. This allows you to eliminate its tension and subsequent detachment.
The following can be used as an artificial analogue of the vitreous body:
- saline solutions (do not require replacement, because over time they are replaced by intraocular fluid);
- or polymers (will require replacement within a certain time).
Depending on the severity and duration of the disease, the operation can last 30 minutes or more.
Contraindications to surgery and risk groups
Each type of surgical intervention has a number of contraindications. Vitrectomy cannot be done in the following cases:
- If there is clouding of the cornea.
- If there are pronounced pathological changes in the tissues of the visual organ.
The filling operation can also not be performed in all cases. It is not done if there is clouding of the vitreous body or protrusion of the sclera.
There are also a number of contraindications to laser treatment. Laser operations cannot be performed in the following cases:
- If the retina is detached over a large area.
- If certain tissues of the eye are opaque.
- If pathologies of the iris vessels are diagnosed.
Any types of surgical interventions are contraindicated if a person is intolerant to painkillers or does not tolerate anesthesia well. It is unacceptable to perform operations for infectious and inflammatory diseases of any etiology in the acute stage.
Before choosing a treatment method and surgery, the doctor carefully studies the patient’s medical record and conducts a detailed examination.
Complications and consequences
Complications after surgery are rare, but they do occur. This is mainly due to a violation of the technique of the operation. The most common consequences include:
- Deterioration in the transparency of the cornea due to its drying out.
- Burns of the cornea and iris.
- Perforation or rupture of the membranes of the eye.
- Hemorrhages in the tissue of the eye. This is observed when the vorticose vein is damaged or when large vessels in the optic organ are damaged.
- Entry of filling material under the retina or under the conjunctiva.
- Strabismus or ptosis is observed when the tissue is stitched incorrectly.
- Cutting seams when applying a filling. Most often this is due to the sutures being placed very close to the place of filling.
- Poor blood circulation in the tissues of the eye. This leads to loss of light perception. Basically, this condition is short-term.
Some time after the operation there may be a relapse. This is due to incorrect surgical technique or incorrect suturing. After surgery, patients are registered with an ophthalmologist and are examined every 2-3 months.
What not to do after surgery
After surgery, it is important to follow the recommendations of your doctor. This will help avoid relapse. In the first month after treatment, the patient should follow these tips:
- Avoid excessive physical activity. Do not play sports or go to the gym.
- Don't lean forward.
- Avoid respiratory and infectious diseases.
- Avoid any procedures that involve sudden temperature changes. You should refrain from visiting baths and saunas.
- Take medications prescribed by your doctor.
- In sunny weather, wear sunglasses.
In addition, a patient who has undergone surgery for retinal detachment should avoid excessive physical activity and intoxication of the body for a long time. Any situations in which visual injury may occur should be avoided.
Walking and swimming are not contraindicated. It is advisable to walk in the shade, and do not strain too much when swimming. During the postoperative period, it is recommended to sleep on your back.
Types of retinal detachment
The types of retinal detachment depend on the cause of the disease. Rhegmatogenous disease is caused by ruptures, which can be caused by trauma, degenerative lesions, myopia, Stickler and Marfan syndromes. Detachment can also occur as a result of cataract surgery.
The traction type of the disease is associated with traction from scars on the surface of the retina. The reasons for their formation can be retinopathy, penetrating eye injury.
With exudative detachment, fluid accumulates in the subretinal space. This can occur in the presence of an inflammatory process, with high blood pressure and vascular diseases, maculopathy, and congenital disorders.
The types of pathology also differ in the degree of damage:
- local – detachment within one quarter of the entire retinal area;
- subtotal – separation and detachment from the fundus occurs;
- total – the entire area of the retina is covered.
The signs of the disease depend on the severity and type of detachment.