Retinoschisis is a disease that is accompanied by retinal separation. The retina itself has ten layers that are responsible for the formation of the visual image. If retinoschisis develops, fluid accumulates between the layers of the retina (approximately in the middle), which causes retinal separation and disruption of its function.
There are two types of retinoschisis:
- Senile (degenerative) retinoschisis.
- Hereditary X-linked retinoschisis.
Information about the disease
Retinal degeneration, retinoschisis, is accompanied by cystic degeneration of its tissues, folding, tears, as well as detachment and lesions of the vitreous body. The name pathology was introduced into practice in 1935. The disease develops against the background of malformations of the photosensitive membrane or its dystrophic changes. The pathology is widespread.
The incidence of retinoschisis in Russia ranges from 4 to 12% in the age group of people 40 years and older. In Europe, this figure is approximately 5%, while the disease occurs in the population after 30 years of age. In the case of a genetically determined form of pathology, clinical signs appear already in childhood - up to 10 years. Early diagnosis and timely treatment of retinoschisis are very important, since patients usually have no complaints during its development. Pathology is detected during an ophthalmological examination or after complications occur.
The invention relates to ophthalmology and is intended to determine indications for choosing treatment tactics for retinoschisis depending on the stage of its development.
Retinoschisis is a complex pathological condition of the retina, characterized by its splitting with the accumulation of fluid between the layers of the retina. Until now, the question of methods for treating retinoschisis is the subject of debate and controversy among ophthalmologists (E.S. Libman. Retinal cysts and their treatment. 1971. - P.78-83).
As you know, the number of patients with retinoschisis increases every year. This disease is polyetiological and has polymorphism, because retinoschisis occurs with glaucoma, vascular disorders, often with proliferative diabetic retinopathy, age-related degenerative changes in the retina, trauma, hereditary degenerative diseases, and is also often combined with myopia. The choice of treatment method for retinoschisis is decisive for achieving the maximum positive result of this complex pathological condition of the retina.
There is a known method of treating degenerative retinoschisis using argon laser coagulation for a delimiting barrier procedure. In this case, radiation is used using an apparatus from HM, model PCDO (USA) with a radiation power of 0.2-0.45 W, an exposure of 0.1-0.2 s and a spot diameter of 100 microns to obtain coagulates of 2-3 intensity degrees, which makes it possible to achieve stabilization of the process in 80% of cases (V.K. Potekhin, T.A. Kurbatova, O.V. Stolyarenko. Argon laser coagulation in patients with retinoschisis // Abstracts of the 7th Congress of Ophthalmologists of Russia. - 2000. - Part 1 . - pp. 474-475).
The use of argon laser coagulation can only be used on the periphery of the retina, since it is known that when it is used in the central zone, clearly biomicroscopically visible damage to the inner layers of the retina remains. Subsequently, this leads to the appearance of secondary retinal degeneration and a more dramatic decrease in visual acuity. In addition, when using a diode laser, fluid resorption is achieved in 70.9% of cases with a significant increase in visual acuity. Whereas when using an argon laser, only 57% with some deterioration in visual acuity (L.I. Balashevich. Creation and study of the effectiveness of using argon and diode lasers in pathology of the fundus: Dissertation ... Doctor of Medical Sciences. - St. Petersburg, 1996 ). Therefore, taking into account these features of the effect of the argon laser on the retina, its use in stage II of retinoschisis when it progresses to the macular area and especially in stage III of the process is highly undesirable. Moreover, applying coagulates over the cyst area is impossible (as we do with a diode laser), because this can cause tears in the retina as a result of the burn effect on the inner lining of the retina that the argon laser has.
The closest analogue of the present invention is a method of the same purpose, including argon laser coagulation for flat peripheral retinoschisis. Methods of treating various forms of retinoschisis (N.G. Lukovskaya. VII Congress of Ophthalmologists of Russia: Abstracts of reports. - M., 2000. - Part 1. - P.456-457). For this type of retinoschisis, the author used barrier laser coagulation using a Visulas 532 nm argon laser from Carl Zeiss. The procedure was performed without preliminary preparation of patients with maximum pupil dilation. The radiation energy was selected individually depending on the state of the refractive media, the type of refraction and pigmentation of the fundus with a coagulate diameter of 200-300 microns with an exposure of 0.1 s in an amount of 150-200 per session. The number of sessions was from 1 to 5. For bullous retinoschisis without breaks, coagulates were applied in the form of concentric circles on the border of the healthy retina. If laser coagulation failed, diathermopuncture of the cyst and diathermocoagulation around the dissection zone were performed. The author notes that argon laser coagulation of the retina represents an area of local burn with subsequent formation of scar tissue and chorioretinal fusion at this site. The consequence of this in long-term follow-up as a result of damage to the pigment epithelium is a high probability of the appearance of secondary dystrophies, decreased twilight vision, deterioration of color perception, limited visual field and the occurrence of retinal detachment. This method of treatment is not safe, especially if laser coagulation sessions are performed more than one procedure, or in the case when the laser exposure area is two or more quadrants. If peripheral local retinoschisis is accidentally detected within one quadrant, as the author notes in his works, he prefers to use either watchful waiting or drug treatment. For bullous retinoschisis, the author suggests using the archaic and even more traumatic method of diathermopuncture and dithermocoagulation, which has not been used for more than 30 years as a method of influencing the retina. Since it is known that as a result of a pronounced burn effect, destruction and fibrosis of the vitreous body occurs in the membranes of the eye, which is manifested by a traction effect on the retina, and is also fraught with the development of cataracts. Therefore, the use of such methods for the treatment of retinoschisis is currently unacceptable. In surgical treatment, the author mainly uses a graft made of porous polytetrafluoroethylene (PTFE). The material consists of nodules interconnected by thin fibrils, and has a high porosity of 90%, mobility and strength. The author points out that despite the presence of numerous pores, the filling is impermeable to blood. This statement of the author, in our opinion, is not logical, since a filling consisting of 90% pores will certainly be permeable to any liquids. The filling is a thin sheet, which during surgery is placed under the main porous and monolithic silicone materials on the thinned scleral membrane. PTFE can be used in this capacity if biomaterials are not available. However, this material cannot be used to create a good impression shaft with high widespread retinoschisis with large gaps, as well as for circular filling. The negative qualities of this material include its excessive mobility, because With this property, it is very difficult to fix it with sutures in the desired position. In addition, the author does not provide clear indications for the use of various methods of treating retinoschisis, in particular for its various manifestations. As you know, the outcome of treatment for any disease depends on the choice of treatment method.
The objective of the invention is to develop clear criteria for selecting various methods of treating retinoschisis.
The technical result of the proposed invention is to increase the functional result of treatment and prevent complications in the form of fibrosis of the macular zone and the appearance of secondary retinal degeneration.
The technical result is achieved by determining the clinical stages of retinoschisis and selecting laser and surgical treatment according to the stage.
To date, there are no clear criteria for choosing methods for treating retinoschisis, especially taking into account recent advances in this area.
Based on a large number of observations over 10 years, we have developed a clinical classification of retinoschisis, retrospectively assessed various approaches to the treatment of this pathology in terms of effectiveness and the presence of complications, and developed treatment tactics depending on the stage of retinoschisis.
| At all stages of retinoschisis, we use laser coagulation using long-wave radiation from a diode laser. In stage I - barrier laser coagulation, in stage II - step-by-step progressive or barrier, in stage III - step-by-step progressive laser coagulation of the retina or in combination with extrascleral filling with a porous silicone segment-oval implant. If the pigmentation of the resulting laser coagulates is incomplete, laser coagulation is repeated. The prerequisites for the use of laser coagulation of the retina using long-wave radiation from a diode laser were the obtained clinical results of the impact of long-wave radiation from a diode laser on the retina (V.V. Volkov., L.I. Balashevich. On the choice of a generator for fundus photocoagulation // Ophthalmol. journal. - 1978. - No. 5. - P. 330-333. Brancato R., Pratesi R. Applications of diode lasers ophthalmology. - 1987. - Vol. 1. - No. 3 - P. 129199). Our preference for using a diode laser is based on the ability of long-wave radiation to coagulate the pigment epithelium and choroid without signs of changes in the retinal vessels, because the maximum absorption of energy occurs precisely in the pigment epithelium with a shift in the thermal effect towards the choroid. In addition, long-wavelength laser radiation is weakly absorbed by lipofuscin, so it can pass through the inner layers of the retinal macula without damaging its structure. Based on these characteristics of the effect of a diode laser on the retina, we have previously developed and tested in clinical practice our own method of step-by-step progressive laser coagulation of the retina for the treatment of retinoschisis, including in the area of its macular zone. The positive clinical effect of this method is associated, on the one hand, with the peculiarities of the impact of the diode laser on the retina, and on the other, with the use of step-by-step effects, starting from the macular zone and around the vessels, and also progressively across the entire area of the cyst to the periphery. Laser coagulates applied to healthy areas of the retina and along the vessels prevent the accumulation of intraretinal fluid, and coagulates on the surface of the cyst probably create shunts between the retina and the choroid and promote resorption of intraretinal fluid. When using a diode laser, neither in the immediate nor in the long-term follow-up, there were no signs of secondary retinal degeneration or any other complications (RU 2441631, 02/10/2012). During surgical treatment by extrascleral filling of the retina, which we propose to use in stage III of retinoschisis when it is impossible to completely block it with laser photocoagulants, it is advisable to use modern universal porous silicone segment-oval implants developed by us together with JSC Medsil (RU 61548 dated February 19, 2008). The use of porous segment-oval implants in the surgical treatment of retinal tears simplifies the surgical technique, because allows you to immediately select the required size and its configuration, without requiring modeling. In addition, the use of universal implants makes it possible to reproduce the impression shaft on the retina without stretching or shortening the implant, thanks to its one-sided convex configuration, which is located on the sclera during surgery. When the implant is fixed with interrupted sutures to the scleral membrane, it is more intimately attached to the sclera and the convex surface is applanated towards the retina. In this case, the height of the impression shaft created on the retina will depend on the height of the implant. This is very convenient during surgery, because allows you to immediately select the required height and width of the implant, position it with its convex surface on the sclera and fix it with interrupted sutures in the projection of the retinal tear. In this case, there is no need to calculate the height of the indentation shaft depending on the stretching of the implant; the moment of modeling is eliminated, which eliminates the occurrence of complications in the form of divergence of the conjunctival scar, cutting of sutures and extrusion of the implant, since the implant has a smooth surface on all sides. The use of universal porous segment-oval implants allows one to avoid a more serious complication in the form of compartment syndrome and, as a consequence, loss of function. The method is carried out as follows. The stage of retinoschisis is diagnosed. At the first stage of retinoschisis, characterized by limited splitting of the retina within one quadrant, elevation of blood vessels and the presence of intraretinal fluid, barrier laser coagulation is performed using a diode laser along the borders of the cyst, over its entire area, as well as along the vessels in the area of retinoschisis. At the second stage of the process, characterized by the progression of retinoschisis without a clear boundary between schisis and the intact retina, or the presence of bullous retinoschisis without a line of demarcation, barrier or step-by-step translational laser coagulation of the retina is performed using a diode laser until a limited area of retinoschisis is completely blocked or intraretinal fluid is completely resorption. For bullous retinoschisis - barrier laser coagulation. In the third stage of retinoschisis, characterized by the fact that retinoschisis occupies two quadrants or more with the presence of extensive cavities, ruptures, hemorrhages and the possibility of transition to limited retinal detachment, step-by-step progressive laser coagulation of the retina is performed using a diode laser. If it is impossible to completely block retinoschisis with laser coagulates, extrascleral filling of the segment-oval with a porous silicone implant is additionally performed. In case of incomplete pigmentation of the resulting laser coagulates, laser coagulation is repeated at all stages of retinoschisis. Example 1. Patient A. Came for a consultation. Ophthalmoscopy of the periphery of the fundus revealed stage I retinoschisis in the area of lattice degeneration of one upper quadrant of the retina with a small amount of intraretinal fluid and elevation of blood vessels in the area of the cyst. In all cases of laser coagulation, the domestic diode laser “Milon Lahta” was used with radiation parameters: wavelength - 0.83 microns, radiation power from 350 to 850 mW (depending on the degree of fundus pigmentation), laser exposure - 0.2- 0.3 s, the diameter of the aiming spot in the focal plane of the slit lamp is 150-200 µm. Barrier laser coagulation was performed along the border of retinoschisis, as well as along the area of the cyst using a diode laser. After 3 weeks, good pigmentation of the laser coagulates appeared, and after 6 months, complete resorption of intraretinal fluid was noted. Example 2. Patient P. diagnosed with stage II progressive retinoschisis in the lower inner quadrant of the retina, characterized by the progression of retinoschisis without a clear boundary between schisis and the intact retina. A step-by-step progressive laser coagulation with a diode laser was performed from the macular area along the area of the cyst along the vessels to the periphery. After 5 days the session was repeated. After 3 weeks, almost complete resorption of intraretinal fluid and good pigmentation of laser coagulates were detected. Visual acuity remained the same. In long-term follow-up, an increase in visual acuity of 0.1 was noted without signs of fibrosis and secondary degeneration in the retina. Example 3. Patient B. Stage III retinoschisis, located in the outer, lower part of the retina, reaching the macular zone and partially in the inner with hemorrhages in the lower-outer sector of the retina. The presence of moderate vitreous traction was noted. Four sessions of step-by-step progressive laser coagulation with a diode laser were performed, as a result of which it was possible to completely relocate the cyst from the central zone and delimit retinoschisis in the lower-outer part at the periphery with several rows of pigmented laser coagulates. During follow-up periods of up to three years, an increase in visual acuity of 0.1 was noted without signs of fibrosis and secondary retinal degeneration. Example 4. Patient Z. Diagnosis: Stage III retinoschisis, occupying almost the entire area of the fundus, except for the upper inner part, with 3 breaks in the inner layer of the retina, Artifakia. A step-by-step progressive laser coagulation of the retina was performed to delimit the macular area, as well as along the area of the cyst and along the vessels, around the breaks. As a result, it was possible to reduce the height of retinoschisis and partially (in the outer part) preserve the macular zone. However, it was not possible to completely move the cyst to the periphery and block it with laser coagulants. A surgical operation was performed for applanation filling of the segment-oval with a silicone porous implant without drainage. It can be stated that in the postoperative period conventional drug therapy was carried out. Visual acuity increased from 0.01 to 0.2. No signs of secondary degeneration or fibrosis were detected. Thus, the success of treatment and the absence of retinal damage as a result of laser photocoagulation depend on adequate determination of the stage of retinoschisis and the appropriate stage of treatment. |
Causes of the disease
In accordance with the etiological classification of Madyarov, proposed by him and his co-authors, retinoschisis is divided into the following forms:
Hereditary . It occurs against the background of genetic disorders and can be linked to the X chromosome. The mode of transmission is autosomal dominant or recessive. In some cases, the disease becomes one of the signs of genetic pathologies - Goldman-Favre disease, Wagner disease.
Degenerative . This is an acquired form of the disease that develops due to dystrophic changes in the retina in people over 40 years of age. Two types can be detected - typical, reticular (with a large cystic lesion of the retina).
Secondary . This form is caused by the presence of serious vascular problems in the retina (diabetic retinopathy, retinal vein occlusion or thrombosis). In addition, secondary retinoschisis occurs against the background of inflammatory processes of the eyes (chronic uveitis, iridocyclitis), eye injuries, neoplasms in the choroid, or the toxic effects of certain medications.
The pathogenesis of retinoschisis is caused by impaired blood flow in the central region of the retina or on its periphery. The retinal lesion in this case has the appearance of cystic degeneration. The resulting cysts merge to form large internal cavities, which stratify the retina. In some cases, the zone of dissection remains intact, although often ruptures occur, which cause retinal detachment, which leads to the death of its structures.
Complications of retinoschisis of the retina
Due to retinoschisis of the retina, various complications often arise. If a retinal dissection occurs, its structure is disrupted and it cannot perform its functions. If the retina is severely damaged, the patient complains of difficulties in orientation. As a result of the disease, vision can deteriorate to the point of complete blindness.
The most common complications from retinoschisis of the retina are retinal rupture or detachment, hemorrhage into the eyeball.
Classification of pathology
Clinical classification T.A. Bagdasarova, distinguishes three stages of retinoschisis:
- First. The retinal split is limited to a separate area, there is no vascular elevation, and there is no intraretinal fluid.
- Second. Retinal splitting progresses without a definite boundary between the affected area and the healthy retina. The formation of microcysts is detected in its layers.
- Third. The lesion with extensive cysts is localized in several quadrants of the retina. Their cavities rupture under the retina. There is a risk of transition of the pathological process to a limited detachment.
Classification of retinoschisis of the retina
In practical ophthalmology, retinoschisis of the retina is classified according to Bagdasarova and is divided into three stages:
- The first stage
- the retina begins to slowly split, vascular elevation occurs and intraretinal fluid is formed. - The second stage
- the retina is actively splitting. The affected area does not have a clear boundary. Small cysts begin to form between the layers of the retina. - The third stage
- the lesion occupies a significant part of the retina. The cysts enlarge, causing the retinal cavity to rupture. Pathology can lead to delineation of retinal detachment.
Symptoms and signs of the disease
Hereditary retinoschisis is usually diagnosed in childhood under 10 years of age. The macula area is the first to be affected, which causes complaints of deterioration of central vision (difficulty with reading, writing, etc.). The defeat is two-sided. Pathological changes affect Müller cells, due to which the nerve fibers begin to peel off from the main retinal tissue. Damage to peripheral areas in this disease most often concerns the inferotemporal quadrant. This is the appearance of giant oval cysts, which later become the cause of detachment.
Degenerative retinoschisis, as a rule, has no symptoms during its course. It is detected by chance, usually during an ophthalmological examination. Manifestations of retinoschisis are found in the outer plexiform layer of the retina. Initial changes develop in the peripheral region of the extreme inferotemporal zone. They are revealed as large areas of retinal layers with small cystic dystrophy. If the process spreads to the macular area or retinal detachment occurs, patients note a decrease in acuity and narrowing of the visual field, visible objects are distorted, and flashes of light may appear before the eyes, indicating retinal detachment.
Secondary retinoschisis is a complication of various eye diseases. Its symptom complex is directly related to the underlying disease. Characteristic manifestations of retinoschisis include extensive detachments of sections of the retina, hemorrhages under its tissue, into cystic cavities, and into the vitreous body. The outcome of this form of pathology is directly related to the outcome of the underlying disease.
Symptoms of retinoschisis of the retina
Symptoms of retinoschisis of the retina appear depending on the cause of the disease. For example, with degenerative retinoschisis, the disease proceeds without any special manifestations. Usually the disease is detected by chance after examination by a doctor. The extreme inferotemporal periphery changes and small cysts form. Only when retinal detachment occurs does vision begin to decrease, the boundaries of objects are distorted and flashes appear in the eyes.
Hereditary retinoschisis is most often detected between 7 and 9 years of age. First of all, the macular area is affected, which is why the patient complains of blurred vision. For example, it becomes difficult to read and write. Damage occurs near the Müller cells, causing nerve fibers to detach from the retina. Most often, the disorder is localized in the inferotemporal part. Large oval cysts and retinal detachment appear.
Secondary retinoschisis occurs as a complication of other eye diseases. For example, there is extensive detachment of the retinal area, hemorrhage into different parts of the eye, including under the retina or into the cyst itself.
Diagnostics
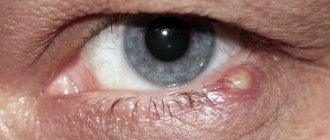
Mandatory examination methods, such as ophthalmoscopy, viziometry, and tonometry, help determine retinoschisis. For ophthalmoscopic examination, a Goldmann lens and a slit lamp are used.
Additional studies - electroretinography (determines residual functions of the retina), ultrasound of the eyes, fluorescein angiography (in case of congenital retinoschisis, detects pathological changes in the macula). Computer perimetry may also be prescribed, the task of which is to determine visual field defects. However, the most informative research method for this pathology is OCT. It makes it possible to most accurately determine existing lesions in the macular area, identify cysts, as well as possible detachments in the peripheral area.
Differential diagnosis is necessary with Stadtgard dystrophy, detachment and retinal vasculitis.
Causes of development and forms of retinoschisis
It is customary to distinguish 3 main forms of retinoschisis:
- degenerative - an acquired disease that occurs after 40 years of age due to degenerative changes, has two forms (typical and reticular);
- hereditary - a consequence of genetic disorders, sometimes accompanied by other pathologies;
- secondary - noted in vascular pathologies of the eyes (for example, diabetic retinopathy), injuries, treatment with certain drugs.
According to experts, retinoschisis develops when the blood circulation of the retina (both the central region and the periphery) is impaired. The consequence of such disorders is the formation of cysts and the formation of cavities, which lead to retinal separation and subsequent death of retinal structures.
There are 3 stages of pathology:
- Stage I – local retinal splitting;
- Stage II – the process of retinal clefting progresses, microcysts are formed, there is no clear boundary between the zone of retinoschisis and the normal retina;
- Stage III – the appearance of a large zone of retinoschisis, extensive cysts, ruptures, limited retinal detachment.
Treatment
Depending on the severity of the case, the following can be used to treat retinoschisis: conservative methods, laser treatment, surgery.
The goal of conservative therapy is to improve microcirculation in the retinal tissue and restore its metabolic processes. This is to prevent relapse of the disease. Therapeutic measures include: the use of complexes of special vitamins, antioxidants, nootropics. The administration of medications is carried out by injection - intramuscularly, intravenously. Treatment is carried out on an outpatient basis, in courses - twice a year.
The goal of laser treatment is to stop the already progressing retinoschisis. For this purpose, laser coagulation of the retina is prescribed - progressive, barrier techniques. Laser exposure is carried out along the border with healthy areas of the retina - circles.
Surgical treatment of retinoschisis - scleral filling, is prescribed in case of detection of retinal detachment. The operation can be performed by a number of methods.
Classification
Retinal separation in retinoschisis occurs in several stages:
- Stage I. Limited retinal dissection, fluid formation around altered vessels.
- Stage II. The dissection progresses, there is no clear boundary between the healthy and altered membrane; small cystic degeneration occurs.
- Stage III. Large cysts and cavities form in the layers, leading to rupture and detachment of the retina. The lesion covers a wide area.
Additionally, watch the video from an ophthalmologist about retinoschisis:
Prognosis and prevention
With retinoschisis of a hereditary form, the prognosis for visual functions is always unfavorable, with a degenerative form it is doubtful. In the case of secondary retinoschisis, its prognosis is directly related to the outcome of the underlying disease.
The best prevention of this pathology is regular ophthalmological examinations, especially for people over 40 years of age. If a person is diagnosed with high myopia, it is worth refraining from serious physical activity and learning to deal with stressful situations at home and at work.
In the case of open-angle glaucoma, be sure to regularly instill prescribed medications and monitor intraocular pressure with an ophthalmologist once every 3 months. Injury to the head and eyes should be avoided. Take tablets for high blood pressure if present. Be sure to visit an ophthalmologist for regular examinations, strictly follow his instructions, which will reduce the risk of possible complications of the disease and stabilize the progression of retinoschisis for a long time.
The specialists of our clinic have accumulated extensive experience in the treatment of degenerative lesions of the retina, including retinoschisis. You can contact us at any stage and with any form of the disease. The best equipment for diagnosis and treatment guarantees our patients early detection of the disease and its adequate treatment, including laser and surgical methods.
Diagnosis of retinoschisis of the retina
After the patient complains, the diagnosis of retinoschisis begins.
To make a diagnosis, the following is usually done:
- Visometry:
determine residual visual acuity. - Perimetry:
assess the boundaries of the visual field. - Tonometry:
IOP is measured. - Ophthalmoscopy:
examine the fundus of the eye using an ophthalmoscope.
There are also additional examination methods, these include:
- Ultrasound of the eyeball if retinoschisis is suspected.
- Electroretinography.
- FAG – fluorescein angiography of retinal vessels.
- OCT – optical coherence tomography.
- Molecular genetic test.
Additional ways to identify the disease help make an accurate diagnosis and get a complete picture of eye disorders. Thanks to the examination, the doctor can determine the size of the cyst and retinal detachment. If a person is diagnosed with any other diseases, he is sent to the appropriate specialist.