Retinal detachment is a serious eye condition that requires immediate surgical intervention. Attempts to do without surgery can lead to complete loss of vision in the shortest possible time. However, even after successful treatment, a number of restrictions remain, some of which must be observed throughout life.
The most important prohibition regarding retinal detachment is that you should never try to cure this disease yourself, using so-called “folk” methods. When the first symptoms appear - spots or sharp flashes before the eyes, sudden deterioration of vision, vibrations of visible objects - you need to consult a doctor. After all the necessary studies have been carried out to clarify the diagnosis, surgery is prescribed.
After operation
- The last step of the operation is to cover your eye with a bandage, protecting it from accidental contamination. The bandage should be removed the next day in the morning and the eyelids should be treated (being careful not to get into the eye) with a sterile swab moistened in an aqueous solution of 0.02% furatsilin or in an aqueous 0.25% solution of chloramphenicol. From the first day following the day of surgery, you should not constantly keep your eye under a tight pressure bandage, because this way it is not able to move and blink freely: for this, a special bandage-curtain made of gauze is used, which does not impede the movement of the eyeball.
- Immediately after surgery, and further in the postoperative period, pain may occur in the eye or periorbital area. It is advisable to relieve the appearance of pain syndrome with Ketanova, Ketorola or Analgin tablets (according to the instructions). Be sure to report any pain to your doctor.
Retinal detachment
- Causes of retinal detachment
- Clinical picture
- Diagnostics
- Treatment
- Complications after surgery
- Prevention
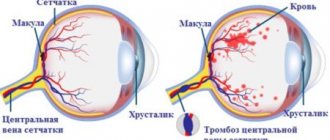
Retinal detachment is the separation of the neurosensory retina layer from the pigment epithelium by a layer of subretinal fluid. Normally, the retina is closely adjacent to the choroid, from which it receives nutrition. Retinal detachment often leads to significant vision loss and blindness.
Most often it occurs with injuries and myopia, as well as with diabetic retinopathy, intraocular tumors, retinal dystrophies, etc. According to the literature, for the occurrence of retinal detachment, not only the presence of a retinal break is important, but also the state of the vitreoretinal interface and the development of proliferative vitreoretinopathy.
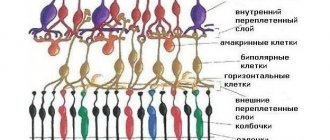
Vitreoretinal relationships include two opposing forces: on the one hand, the state of the choroidal pump - factors that ensure the retina adheres (osmotic pressure of the choroid, hydrostatic pressure in the retinal vessels, active transport of various substances through the pigment epithelium), interphotoreceptor matrix (contact density between the membranes of cones and rods with apex of the pigment epithelium), on the other hand, changes in the vitreous body: liquefaction of the vitreous body (syneresis), posterior detachment (PVD), vitreal traction.
Causes of retinal detachment
There are three types of retinal detachments:
(primary) retinal detachment - associated with the presence of a retinal break
Rhegmatogenous- Traumatic retinal detachment - associated with eye trauma
- Exudative (secondary) retinal detachment is a consequence of eye diseases such as tumors of the retina and choroid, and various inflammatory diseases.
Let's look at the reasons for the development of retinal detachment in more detail:
- Change in the vitreous leading to rupture. The retina does not move from its place if it is sealed (maintains its integrity) and there is no tear in it. If a gap has formed, then through it the fluid from the vitreous body penetrates under the retina and peels it off from the choroid. The main reason for the formation of a retinal tear is the tension of the vitreous body when its normal state changes. This process occurs in this way: normally, the vitreous body resembles a transparent jelly. In some cases, it changes and becomes cloudy with dense strands, i.e. compacted fibers that are connected to the retina. When the eye moves, the cords pull the retina along with them, which can lead to its rupture.
- Dystrophy (thinning) of the retina.
- Large tears often occur with eye injuries.
- Traction (tension) from the modified vitreous body without the formation of retinal breaks (this often happens with diabetic retinopathy).
- Volumetric formations under the retina (tumors, fluid accumulation, etc.).
Clinical picture
Subjective symptoms:
- the appearance of a “veil” before the eye. Patients unsuccessfully try to eliminate it on their own by washing their eyes with tea or instilling drops. In this case, it is important to remember and tell the doctor on which side the “veil” originally appeared, since over time it can increase and occupy the entire field of vision;
- floating black “sights”, “dots” in the field of vision
- flashes in the form of sparks and lightning are also a characteristic feature of ongoing retinal detachment;
- a decrease in visual acuity, distortion of the letters or objects in question, and loss of individual parts of them from the field of view indicates that the detachment has affected the center of the retina.
- vision improves somewhat after sleep. This is explained by the fact that when the body is in a horizontal position, the retina returns to its place, and when a person takes a vertical position, it again moves away from the choroid and vision defects resume.
Retinal detachment cannot be cured with any drops, tablets or injections. The only way to restore vision and save the eye is urgent surgery.
When a retinal detachment occurs, nerve cells, rods and cones die, and the longer the detachment lasts, the more of these cells die and the worse the vision recovery even after successful surgery.
Diagnostics
- visometry (visual acuity test), which will show the condition of the central region of the retina;
- computer perimetry (study of the peripheral and central field of vision) to assess the condition of the retina in its periphery;
- tonometry (measurement of intraocular pressure). With retinal detachment, it may be below normal (normal is 16-25 mm Hg);
- a special electrophysiological study will determine the viability of the nerve cells of the retina and optic nerve;
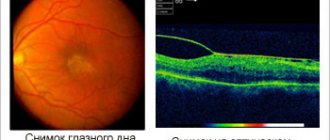
- ophthalmoscopy (examination of the fundus of the eye). This will help to accurately determine the location of retinal breaks and their number, to identify thinned areas that can lead to the emergence of new foci of the disease;
- An ultrasound examination will give an idea of the size of the detached retina and the condition of the vitreous. This study is especially important for opacities of the cornea, lens or vitreous body, when it is impossible to see the retina.
- laser tomography for in-depth examination of the retina and optic nerve using a retinotomograph.
Treatment
In preparation for the operation, a few days before it, you need to do routine blood and urine tests, an electrocardiogram, a chest x-ray, and examinations by a dentist, otolaryngologist and therapist.
On the morning of the operation, drops are instilled into the eye to dilate the pupil. You may also be given a mild sedative to help you relax and not worry.
In the operating room you will be accompanied by a surgeon, his assistant, an operating room nurse, an anesthesiologist and a nurse anesthetist. Surgeries for retinal detachment are performed under general and local anesthesia under an operating microscope.
To restore the tightness of the retina around the rupture, inflammation is caused (exposure to cold (cryopexy) or laser) followed by scarring in this place.
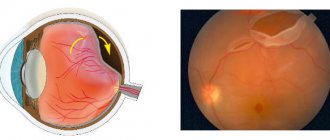
To improve sealing, the membranes of the eyeball are brought together in the following way: a special silicone seal in the form of a cord is sutured to the outside of the eyeball, which presses the wall of the eye and brings the choroid closer to the detached retina.
Depending on the specific type of retinal detachment, the surgeon will choose one of certain surgical methods or a combination of them:
- A seamless technology of circular, sectoral and radial episcleral filling is used using scleral allografts and medical glue, and silicone is also used as a material.
Local filling in the area of retinal rupture, it is carried out in cases where the retina is partially detached;In this case, a thin silicone strip (filling) is attached to the sclera through sutures so that the sclera under the strip is pressed inward, while the sclera and choroid move closer to the retina, the tension of the vitreous fibers is weakened, the retinal tear is blocked, in general, conditions are created for its adhesion. The silicone filling is not visible after surgery and remains in place forever.
Circular filling is used in more severe cases when the retina has completely detached; When the filling is circular and completely covers the eye, anterior-posterior lengthening may occur, which leads to slight myopia.
- Ballooning of the sclera. The essence of the operation is to temporarily suturing a special catheter with a balloon to the sclera in the area of projection of the retinal tear.
When inflating such a balloon, the same effect occurs as when filling the sclera (an indentation shaft is formed). Blocking the rupture with a balloon allows for resorption of subretinal fluid and subsequent laser photocoagulation of the retina. After the formation of adhesions of the retina with the underlying tissues, the balloon is removed. Scleral ballooning is less traumatic than filling, however, the indications for the latter operation are much wider.
- Vitrectomy is a method in which the altered vitreous body is removed from the eye and one of the necessary drugs is injected instead: saline solution, liquid silicone, a perfluorocarbon compound in the form of a liquid or a special gas, which presses the retina from the inside to the choroid;
Vision through silicone oil is very poor, so after a while, if the retina is in place, the silicone oil is replaced with a saline solution.
- Laser photocoagulation to limit the area of rupture and thinned areas of the retina.
The combination of these interventions is selected individually for each patient and depends on how much time has passed since the onset of retinal detachment, how large it is, how many breaks there are, where they are located, etc.
Depending on the specific case, treatment can be carried out in one or several stages.
Complications after surgery
In the early postoperative period
- Infection of the surgical wound and introduction of infection into the orbital tissue surrounding the eyeball (acute orbital cellulitis). To prevent the development of infectious complications in the postoperative period, the patient is prescribed complex (local and general) anti-inflammatory and antibacterial therapy;
- Detachment of the choroid;
- Increased intraocular pressure;
- Imbalance of the extraocular muscles in the early postoperative period, accompanied by a feeling of double vision;
- Drooping of the upper eyelid (ptosis) due to injury and stretching of the muscle that lifts the upper eyelid during surgery and the negative impact of eyelid swelling in the postoperative period.
- When a large filling is located under the extraocular muscle, its function may be impaired—the development of strabismus;
In the late postoperative period
- Exposure of the implant (late complication: occurs several weeks or months after surgery). Treatment involves covering the exposed sponge with conjunctiva. If the implant becomes infected, it is removed;
- Various changes in the central (macular) region - the formation of membranes that cause deformation of this area of the retina, leading to distortion of objects and decreased visual acuity (“cellophane” maculopathy); formation in the macular area of microcysts (microcavities in the thickness of the retina) and foci of degeneration (cystic maculopathy), etc.;
- Change in refraction towards myopia (within several diopters). This occurs more often with circular filling of the sclera due to the fact that the depression shaft artificially increases the pre-posterior axis of the eyeball (see the “refraction” section). With a large radial filling, astigmatism may develop, which is difficult to correct;
- Cataract formation;
Failures of extrascleral retinal detachment surgery
- Lack of retinal detachment in the early postoperative period. The most common reasons: a) incorrect placement of the filling and, as a result, failure to block the retinal tear; b) a situation where during the operation all retinal breaks were not found, or new ones formed.
- Repeated retinal detachment (relapse): the most common cause of recurrent detachment is the development of changes in the vitreous body and on the surface of the retina (the so-called proliferative vitreoretinopathy). In this case, pronounced traction occurs on the retina, which can lead to its deformation, the emergence of new breaks or the unblocking of old ones. Effective treatment of this condition requires endovitreal intervention (see below). Conservative treatment (use of enzyme preparations in the form of tablets or injections) is usually ineffective.
Restoration of visual functions in the postoperative period occurs gradually, over several months. Postoperative visual acuity largely depends on the duration of the detachment and the involvement of the macular area in it.
Prevention
In some cases, retinal detachment can be prevented. If a person has myopia or retinal dystrophy, he should be regularly examined by an ophthalmologist, and if necessary, timely laser coagulation of the retina or, if the optical media is opaque, cryopexy.
If the vitreous changes, surgery may be performed to replace it.
To prevent eye injuries, which is a common cause of retinal detachment, especially in young men, basic precautions and safety rules should be observed both at work and at home.
Rehabilitation period
The recommendations below are general recommendations developed for most patients. If the course of the postoperative period is individual, the doctor will offer an individual treatment regimen, as well as a schedule of examinations of the patient. His recommendations must be clarified at each visit!
- Mode. A specific postoperative regimen can have enormous therapeutic value. Therefore, you should strictly follow the recommendations for compliance on the first postoperative day that you receive from the surgeon. In the future, the features of postoperative behavior should be clarified during regular examinations.
- Hygiene. When washing your face, you should avoid getting soap or water in your eyes. Washing your hair should be done with your head tilted back. If, nevertheless, water gets into the operated eye, rinse it with an aqueous solution of 0.02% furatsilin or an aqueous solution of 0.25% chloramphenicol (sold in a pharmacy).
- Don't miss your doctor's appointment!
- During the first postoperative days, it is recommended to wear a bandage (“blind”) on the operated eye to protect it from dust present in the air and the effects of bright light. This bandage is made of two-layer gauze and is attached in front of the eye to the forehead using an adhesive plaster, like a “curtain”. It does not put pressure on the eyeball.
- Eye drops are recommended in the postoperative period for better healing, as well as to prevent infectious complications. Often, after surgery, the surgeon recommends instilling several drugs: anti-inflammatory drops (Naklof, Indocollir, etc.), disinfectant drops "Ciprofloxacin", "Tobrex", (Floxal, etc.) or combined agents (Maxitrol) , "Tobradex"). Drops, as a rule, are prescribed according to a decreasing scheme: four times a day - the first week, three times a day - the second week, twice a day - the third week, once daily - the fourth week, then they are discontinued.
Late recovery period
One month after the operation, a scheduled visit to the doctor is scheduled. At this time, the ophthalmologist will examine the fundus of the eye and evaluate the dynamics of the retinal disease.
After this, the number of restrictions decreases, but you need to be smart about your health and eyes. Not worth it:
- Stay in the sun for a long time;
- Be in traumatic situations where the operated eye can be damaged;
- Perform serious physical activity;
- Drink alcohol, smoke and expose the body to other intoxications.
Visual acuity, need for glasses
Visual acuity after surgery is restored gradually. This happens in the first 2 or 3 months. In some patients, visual acuity gradually recovers within six months. As a rule, this process occurs more slowly in myopic patients, people with diabetes, and the elderly.
The rehabilitation period can “make” your eyes “different”. Which necessitates the selection of temporary glasses or contact lenses to correct the situation. The final spectacle correction should be done after 2 or 3 months of the recovery period, although these terms are negotiated individually, especially when only one eye has been operated on.
The gradual restoration of vision may cause distortion of visible lines and objects in some patients, and sometimes double vision appears. Typically, it may take several weeks or months of recovery for these symptoms to disappear.
PREVENTION OF RETINAL DETACHMENT
I started with prevention deliberately, because a timely preventive procedure can reduce the risk of detachment by an order of magnitude.
Since previous posts described in detail how this happens, I want to draw your attention to some points.
1. We say that, as a rule, laser coagulation is not a painful procedure, but there is always an adjustment for individual sensitivity. In some cases it can be painful, and in those who are especially impressionable, even very painful. The following factors play a role:
— the volume of coagulation and localization of zones, — the type and model of the laser, — the patient’s position and behavior during it, — the anatomy of the palpebral fissure (“deep-set” eye, large nose, etc.) — the experience of the laser surgeon and the correct choice of contact lens.
Conclusion: if you have a high pain threshold, are afraid or feel uncomfortable during the procedure, be sure to notify the doctor in advance or during it; with the help of medications, we can significantly facilitate the laser coagulation process.
Further care (recommendations)
Gradually, the restrictions imposed during the rehabilitation period will be lifted. Below are some useful tips to help preserve your vision:
- Do not drive until your eye heals.
- Do not rub your eye or put pressure on it.
- Take frequent breaks while watching television or reading.
- If possible, use sunglasses to protect your eyes from UV rays.
- Follow the established schedule of doctor visits.
What restrictions does retinal detachment impose on future life?
Unfortunately, even a successful operation does not guarantee that the retina of the eye will not exfoliate again or that tears will not occur in it. Therefore, observing certain restrictions only during the recovery period may not be enough: some of them will have to be adhered to throughout your life.
Thus, it is extremely undesirable for people with a similar disease to engage in sports, especially those associated with sudden movements, jolts, jumps, and impacts. All martial arts, horse riding, running, and diving are prohibited. However, swimming and morning exercises, consisting of a set of simple exercises, will only be useful.
In some cases, the ban on heavy lifting remains for life. In addition, it is prohibited to perform any work that requires bending, as well as to stay in the hot sun for a long time.
Additional Information
1. When gas is injected into the eye at the final stage of the operation, some peculiarities sometimes arise in the postoperative period. Thus, in the first postoperative days, visual acuity can be extremely low, since light does not penetrate through the gas to the retina. As the gas resolves (up to 2 weeks), the upper part of the visual field will begin to brighten, and the patient will be able to notice a “separation of media,” which will change position following head movements. After 7 or 10 days from the day of surgery, when less than a third of the volume of gas remains in the eye, a single bubble of gas will split into several small bubbles. In some cases, when the gas expands (within three days after surgery), intraocular pressure may increase. As a rule, this process is accompanied by pain and hyperemia of the eye, which requires immediate contact with your doctor! 2. During a surgical intervention that takes place in two stages, after the first operation, so-called “heavy water” is injected into the vitreous cavity, which is necessary to “straighten” the retina and stop bleeding. The second stage of surgical treatment will be possible in 7 or 14 days. Between stages of the operation, it is recommended not to sleep on your stomach, and also not to tilt your head down. 3. If the final stage of the operation is the introduction of liquid silicone into the eye, when selecting glasses you need to remember that while it is present in the eye, visual acuity should be corrected with plus glasses (4.0 - 6.0 D). Silicone will be removed from the vitreous body no earlier than 2 months after the operation. The patient should be aware that the presence of silicone in the eye sometimes leads to rapid clouding of the lens of the eye (the development of cataracts) and provokes an increase in intraocular pressure. What happens, as a rule, in the early stages of the postoperative period. 4. For patients with diabetes. The final stage of the operation, as well as the postoperative period, requires the injection of an anti-inflammatory drug solution (Dexamethasone, Kenalog or Diprospan) into the periorbital area. Despite the small dose (up to 0.5 ml), in some patients with diabetes this causes an increase in blood glucose concentration, which usually occurs in the first two days after the injection. Be sure to take appropriate precautions!
Is it possible to restore vision?
This is the main question that worries people who have experienced retinal detachment. This can only be answered after a thorough ophthalmological diagnosis. If the detachment is minimal, the chances of saving vision are quite high, but mandatory surgery will be required.
Depending on the area of the detachment, the patient's medical history and other factors, the ophthalmic surgeon may offer different types of treatment. During vitrectomy, the vitreous body is removed and replaced with a special composition that allows the retina to be fixed to the choroid.
For extrascleral filling or ballooning, a special balloon is placed in the area behind the eyeball. It blocks tears and ensures proper fit of the retina.
In many cases, laser coagulation helps prevent the problem of detachment, and therefore loss of vision. This is the most effective method of preventing this pathology. Using a laser, you can get rid of small tears and strengthen thinned areas of the retina due to the formation of microadhesions with the choroid.
Laser coagulation is effective for incipient detachment, so to preserve vision it is important to see a doctor at an early stage of the disease. Timely diagnosis significantly increases the effectiveness of treatment.
Rules for applying drops
- Wash your hands with soap and dry them.
- Open the bottle.
- Lie on your back or tilt your head back and look up.
- Bring the inverted bottle to your eye and place it directly above it, without touching the tip to your eye or eyelashes.
- Gently pull the lower eyelid down.
- Move your eyeball up and slowly squeeze the bottle so that the dropped drop can fall into the space created by retracting the eyelid.
- Close your eye.
- Press with your finger (through a napkin) the inner corner of the eye to enhance the effectiveness of the effect, as well as minimize possible systemic side effects of the applied drug.
- When prescribing several eye drops at once, allow at least 5 minutes between drops. The last to be instilled are agents that reduce intraocular pressure.
- Close the bottle tightly and store it according to the attached instructions.
Causes
The causes of a retinal tear are as follows:
- damage due to chronic atrophy;
- retinal tear due to detachment of the posterior hyaloid membrane.
Factors that aggravate and provoke a violation of the integrity of the shell:
- head injuries;
- progressive myopia;
- sudden jump or tilt;
- mechanical damage;
- stress;
- high blood pressure;
- physical exercise.
Violation of the regime in the postoperative period
After laser eye surgery, strict adherence to restrictive measures is required until the recovery period has passed. This applies to any operation. It is extremely undesirable for cosmetics, soaps, and shampoos to come into contact with the mucous membrane. You cannot visit the sauna and swimming pool for two weeks, overload your eyes with reading or working at the computer, drive a car, or play sports. You should definitely moisturize the mucous membrane with drops prescribed by your doctor - under no circumstances choose them yourself! A list of restrictions is given to each patient. Unfortunately, not everyone strictly follows it, ultimately causing harm to eyes that are just healing after surgery. They may begin to water, become very red, hurt when blinking, or itch. In this case, you need to quickly visit a specialist who will check your vision organs.
Classification
There are the following types of retinal tears:
- Perforated - formed on thinned areas of the eye shell, which entails detachment;
- Macular - a complex form, the result is partial or complete blindness. The violation occurs in the central part, surgical intervention is necessary;
- Valvular - retinal rupture is provoked by posterior vitreous detachment.
- Along the dentate line - manifests itself with head injuries, bruises and concussions. The tear occurs along the edge of the vitreous.
All of the above pathologies require surgical treatment.