Age-related macular degeneration (AMD) is the most common cause of vision loss in older adults in developed countries and accounts for ⅓ one-third of cases of blindness.
AMD is a painless, irreversible, degenerative eye condition associated with damage to the photoreceptors.
This is a degenerative disease of the central part of the retina. It is characterized by loss of visual acuity as a result of degeneration of the choriocapillaris layer and retinal pigment epithelium.
Prevalence is high in Western countries. Detection among persons over 55 years of age is 1.6% and increases to approximately 13% in persons over 84 years of age.
Causes
AMD is a disorder of the back part of the eye called the macula (the central part of the retina—the “film” that lines the inside of the eye). AMD is multifactorial and involves an interaction of genetic, environmental, metabolic and functional factors, including:
- aging;
- family history;
- smoking;
- high blood pressure;
- obesity;
- hypercholesterolemia;
- arteriosclerosis.
Deterioration of the macula leads to the loss of only central vision, while peripheral vision remains intact. Central vision is needed to identify letters, numbers, facial features, boundary surfaces, angles, and colors; reading, driving, watching TV and many other activities, high clarity vision.
Symptoms of the disorder
Since the disease is accompanied by damage to the central zone of the retina - the macula, which is responsible for central vision, the first symptom of the disease is deterioration of central vision. This manifests itself as problems when writing, reading, watching TV, looking at people's faces, etc.
In addition, the disease can be identified by the presence of the following symptoms:
- Two eyes see the same object, but not the same size.
- Straight lines are perceived by the eyes in a distorted form.
- Blurred vision in the central part of the eye.
- Distorted perception of colors.
Often the initial stage of the disease does not manifest itself with any symptoms and is detected only during an ophthalmological examination. Sometimes patients, for some time after the development of the pathology, do not notice a decrease in vision in one eye and do not attach importance to minor changes associated with the perception of colors and images.
Kinds
There are two forms of AMD:
- Dry (non-exudative). Caused by small yellow deposits called drusen that form between Bruch's inner collagen layer and the basement membrane of the retinal pigment epithelium. These are extracellular deposits that grow in size and stop the flow of nutrients into the retina. Drusen cause cell death, causing blurred vision.
- Wet (exudative). With this form of the disease, capillary growth changes. They grow through Bruch's membrane into the space between the pigment epithelium and the retina. Blood vessels are fragile, break, and lead to detachment.
Age-related macular degeneration: dry form
The macula, or macula, is the central part of the retina, consisting of several layers: photoreceptors, pigment epithelium and Bruch's membrane, which acts as a partition between the upper layers and blood vessels (choriocapillaris). Over time, metabolic processes in the human body slow down. This leads to the accumulation of cell waste products in the macula. As a result, special compactions are formed in the layers of the macula - drusen. The presence of many such small formations is a sign of the early dry form of AMD. At this stage, there is practically no deterioration in vision, especially if the pathology is localized on one side. This is due to the fact that a healthy eye compensates for the work of the visual system due to more intense functioning. Over time, age-related macular degeneration (dry form) progresses to an advanced stage. At the same time, an increase in the size of drusen and their number is observed. In addition, destructive processes begin to occur in light-sensitive cells and tissues surrounding the macula. This leads to a significant decrease in visual acuity and contrast sensitivity of the eyes. Also, in many patients, first a blurry and then a dark spot appears in the center of the visual field. In this regard, straight lines are perceived as partially broken, and the picture is greatly distorted, for example, a straight doorway may appear skewed. In addition, in the advanced stage of dry AMD, there may be increased eye sensitivity to light, impaired spatial vision, and difficulty distinguishing colors. All of the above symptoms impose restrictions on the performance of any work that requires good visibility near and far. If left untreated, the dry form of AMD rapidly progresses and becomes wet.
Dry form of AMD: stages
Early stage. It is often asymptomatic and does not cause a decrease in visual acuity. At this stage, compactions (drusen) form in the structural layers of the macula.
Developed stage. Characterized by an increase in the size and number of drusen. At this stage, blurred vision and a sharp decrease in visual acuity, as well as other uncomfortable symptoms, are observed.
Progressive stage. It is characterized by the transformation of pathology into a wet form.
Symptoms
In the early stages of macular degeneration, signs may go undetected. Among the first symptoms are the following:
- distortion of the shape of objects;
- deterioration of color vision;
- impaired perception of distances;
- the appearance of dark spots in the central field of vision;
- the need for a higher level of lighting;
- decreased visual acuity.
If any of the above symptoms occur, consult your doctor immediately for a comprehensive eye examination.
The main factors in the development of age-related macular degeneration:
- Age: The likelihood of developing the disease increases with increasing age.
- Race: More common in whites, but generally found in all races.
- Skin pigmentation: Macular degeneration is more common in less pigmented people.
- Iris color: People with lighter skin have a greater risk of developing macular degeneration.
- Gender: Women are at greater risk.
- Smoking is an established risk factor for both forms of macular degeneration.
- Obesity, syndrome X or metabolic syndrome.
- Sleep apnea (holding your breath during sleep reduces the amount of oxygen taken in by 25%)
- Sun exposure: Those who spend a lot of time outdoors throughout their lives, as well as those who live near the equator and at high altitudes, are at greater risk.
- Medications: Some medications may predispose you to macular degeneration.
- High degree of myopia.
- Genes are perhaps the most important risk factor besides age.
Diagnostics
In the early stages of AMD, there are no symptoms, but in some cases, patients may complain of acute vision loss, metamorphopsia, blurred vision, scotomas, or chronic visual distortions.
Since the onset of the disease often goes undetected for a long time, a thorough examination is recommended. The diagnosis is usually made by an ophthalmologist.
About 13% of patients with AMD have Charles Bonnet syndrome, in which mentally healthy patients experience vision loss and complex visual hallucinations.
Various tests are used to establish a diagnosis. This:
- visometry;
- extended ophthalmoscopy;
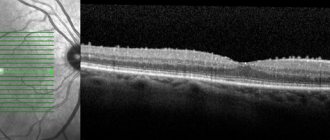
- optical coherence tomography;
- fluorescein angiography;
- fundus autofluorescence and ultrasound.
The Amsler test is also required. He will check for problems in the macula. It is made of straight horizontal and vertical lines. In AMD, straight grid lines appear broken or wavy.
Forms of AMD
Intense metabolic processes in the retina of the eye lead to the formation of reactive oxygen species, including free radicals, which contribute to the development of degenerative phenomena in tissues in case of insufficient functioning of the antioxidant system (AOS). This leads to the formation in the macular and paramacular areas of the retina of non-cleavable polymer structures - drusen, the basis of which is lipofuscin.
When drusen are deposited, atrophy occurs in the adjacent layers of the retina, and the growth of newly formed pathological vessels in its pigment epithelium is also noted. Then there are scarring processes, which are accompanied by the loss of retinal photoreceptors.
In ophthalmology, it is customary to distinguish between two forms of AMD – dry (non-exudative, atrophic) and wet (exudative, neovascular).
The dry form of AMD is much more widespread than the wet form and is found in 85% of cases. With it, yellowish spots - drusen - are revealed in the macular area. The gradual loss of central vision significantly limits the ability of patients to recognize small details, however, this form of the disease is not as severe as the wet form. The dry form of AMD can gradually progress over several years to the stage of late geographic atrophy (GA), with slow degradation of retinal cells and lead to vision loss.
There is no radical treatment for dry AMD, although some drugs are already in clinical trials. Scientific research shows that certain nutrients, such as vitamins A, C and E, can, if not prevent, then significantly slow down the progression of the disease. Regular intake of certain nutritional supplements - eye vitamins - reduces the risk of developing AMD by almost 25%. Protecting your eyes from UV rays with sunglasses will help reduce the risk of developing AMD or slow its progression in the dry form of the disease.
The wet form of AMD is diagnosed in approximately 15% of cases of age-related macular degeneration. The disease progresses rapidly, leading to significant loss of central vision. In the wet form of macular degeneration, rapid neovascularization occurs with the growth of new blood vessels. These vessels are defective and have fragile walls that allow blood cells and lymph to pass through, which flow out and accumulate under the retina. This condition causes damage to the photoreceptors in the retina, which die, forming blind spots (scotomas) in central vision.
The process of growth of newly formed vessels in wet AMD is called choroidal neovascularization (CNV). Moreover, abnormal vascular growth is a mistake by the body in an attempt to create a new network of blood vessels to provide nutrients and oxygen to the retina. Instead, scars form in place of the ruptured vessels, leading to loss of central vision.
Treatment
In dry macular degeneration, the macular tissue gradually becomes thin and stops working normally. There is no cure for this form of the disease, and loss of the central visual field cannot be restored.
Scientists and doctors believe there is a link between diet and the progression of dry age-related macular degeneration. Changes in diet and taking additional vitamin supplements will help slow down the deterioration of vision.
Wet macular degeneration occurs when fluid leaks from newly formed blood vessels under the macula. This leads to blurred vision.
If the wet form of the pathological condition is detected early, treatment is carried out using a laser. The beam of light seals the damaged blood vessels that damage the macula.
Vascular endothelial growth factor inhibitors are the standard treatment. Medicines stop the growth of new blood vessels and prevent them from rupturing. They are delivered by injection into the eye, administered by an ophthalmologist. During insertion, the patient will feel a slight pressure. First, local anesthesia is given to reduce discomfort.
The frequency of drug administration is determined by the doctor. The ophthalmologist is based on the chosen medicine. This treatment will not completely eliminate AMD, but it will minimize the risk of vision impairment.
Photodynamic therapy (PDT) is used occasionally. A laser beam with photosensitive dye destroys unhealthy new blood vessels. Several treatments may be needed as directed by your doctor.
Reasons for development
Often the cause of the formation of AMD is a hereditary predisposition.
According to statistics, this disease most often occurs in patients whose parents also suffered from AMD.
Therefore, those who have older relatives with this disease, after 40 years of age, need to undergo routine examinations with an ophthalmologist every year.
In addition, the disease can develop due to the following provoking factors:
- Smoking - this harmful habit harms not only the heart, blood vessels, lungs, etc., but also the visual organs. Tobacco products contain more than 400 thousand toxic compounds that disrupt the function of the vascular system of the eyes, cause cataracts and various degenerative processes.
- An unbalanced diet leads to a deficiency in the body of nutrients important for its normal functioning. In particular, a lack of vitamins A, C, E, B, lutein, and beta-carotene can lead to deterioration of vision and the formation of degenerative processes in the eyes.
- Pathologies of the circulatory system of the retina - impaired blood supply to the organs of vision and vascular diseases of the eyes are one of the main causes of IOP. The progression of this pathology can also be caused by diseases that cause disruption of the blood vessels and heart - diabetes, hypertension, high cholesterol.
- Exposure to UV rays - the eyes are the organs most sensitive to the negative effects of sunlight. It is especially harmful to be in the sun for a long time from 10 to 15 hours of the day. Reflection of the sun's rays from large surfaces of snow or water also leads to damage to the retina and macula. The sun in the equatorial zone, as well as prolonged stay at high altitudes above sea level, have a negative effect on the eyes.
- A sedentary lifestyle causes circulatory problems in the body and organs of vision.
Treatment of macular degeneration of the retina
If the disease begins to progress, then it becomes impossible to completely get rid of it. With timely treatment of macular degeneration of the retina, vision loss can be stopped.
Drug treatment of macular degeneration is possible only at the initial stage of development of the pathology. There are many medications on the pharmaceutical market that are administered for macular degeneration of the retina. In each specific case, treatment is selected individually for the patient.
Laser treatment
When newly formed vessels are localized outside the center of the macula, experts recommend timely laser coagulation, which helps to obtain a high functional result. The main goal of this therapy is to block the blood vessels that grow under the retina and provoke its detachment.
The disadvantage of using laser coagulation is that such treatment is aimed directly at eliminating the consequences of AMD, and not at the root causes of its occurrence. Therefore, it is not possible to improve vision or stabilize it with the help of laser surgery, but only to stop the progression for a while.
Photodynamic therapy
The method is relatively new. Photodynamic therapy is based on the photochemical effect on formed vessels. The essence of this treatment is that a special medication is administered intravenously to a person and after that the fundus of the eye is irradiated.
As a result of this treatment, the abnormal blood vessels become blocked and the retinal edema resolves. This method, compared to laser treatment, has the most gentle effect on the retina and does not provoke the formation of atrophy of the fundus membranes.
Intraocular injections
The method is considered the most common in the treatment of wet forms of macular degeneration. Thanks to special injections, swelling in the retina is eliminated and the growth of pathological blood vessels is prevented.
Regardless of the method of treating macular degeneration, a lot of strength and patience is required from a person. If the first signs of macular degeneration of the eye occur, seek qualified help as soon as possible. Before symptoms appear, it is recommended to give preference to a healthy diet, give up bad habits and regularly visit an ophthalmologist.