The macula is the central area of the retina. It provides clear vision of objects located directly in front of the eyes, and also allows you to distinguish colors, read and write. Degenerative changes in the central part of the retina pose a serious danger because they significantly impair vision. The likelihood of developing this pathology increases with age. In people over 55 years of age, macular degeneration is one of the most common causes of vision loss.
Causes of the disease
Macular degeneration develops as a result of metabolic disorders in the central part of the retina. Age-related macular degeneration is to some extent always due to a general age-related slowdown in metabolism. In addition, past injuries and chronic diseases can have a significant impact. It was revealed that the likelihood of developing this pathology is slightly higher under the following conditions:
- age over 50 years;
- Caucasian race;
- light iris;
- the presence of retinal diseases in close relatives.
The following can also have a negative effect: smoking, abuse of fatty foods, lack of vitamins, vascular diseases and endocrine disorders, frequent exposure to the open sun without protective glasses.
Causes of pathology of the macula of the eye
There are many reasons why pathological processes in the macula can occur. Here are the main ones:
- Age-related changes. Over time, the amount of pigment decreases, resulting in less protection for that area of the eye. Also, some age-related diseases lead to visual impairment.
- Inflammatory processes in the eyeball area. They can be caused by various factors.
- Eye infections. These include tuberculosis, some sexually transmitted diseases and others.
- Eye injuries, penetrating injuries as a result of a blow or foreign body entering the eye.
- Some endocrine diseases, diabetes and hypertension.
- Diseases of the blood vessels in the eyeball, their blockage or rupture.
The pathological process can lead to changes in the structure of the eyeball, as well as cause changes in the macula, which will disrupt the ability of this part of the organ to perform its functions.
Types of age-related macular degeneration
There are two types of macular degeneration. The clinical picture of one type or another may indicate the stage of development of the pathology.
The dry form is characteristic of initial dystrophic processes. In 90 percent of cases, patients come to the ophthalmologist at this stage because they notice a decrease in central vision. Already at this stage, it will not be difficult for an ophthalmologist to identify AMD when examining the fundus.
The wet form of macular degeneration develops if treatment is not started in the initial stages. This form is characterized by the appearance and destruction of new fragile vessels. In their place, drusen form - yellowish accumulations of hemorrhage products. The development of dystrophic and degenerative processes at the stage of wet macular degeneration occurs faster than in the dry form of the pathology.
What is macular degeneration of the retina?
Macular degeneration of the retina is a disease that affects the central region of the retina and leads to weakened vision. First of all, the lumen of the vessels of the membrane that feeds the retina decreases. As a result, tissues begin to lack essential substances and oxygen. Malfunction of the macula provokes deterioration of vision or its complete loss. Such cases occur especially often among patients over 50 years of age. Macular degeneration is called age-related.
Thus, the main factor in the development of the disease is the aging process. The likelihood of developing macular degeneration increases with age. Women are more susceptible to it, due to the fact that their life expectancy is higher than that of men. People with a hereditary predisposition to it are also more likely to develop macular degeneration. Therefore, patients whose close relatives suffer from this disease should take greater care to preserve their vision. It is believed that Europeans have a high predisposition to macular degeneration. The risk of vision impairment in African Americans is significantly lower for this reason.
Macular degeneration can be dry or wet. The first type of disease is more common and is characterized by progressive macular atrophy. In this case, vision loss occurs slowly. The cause of wet macular degeneration is the formation of too fragile and permeable vessels. They participate in the restoration of the macula, but at the same time lead to bleeding and cause tissue swelling. With wet macular degeneration, the quality of vision decreases much faster, so if left untreated, the disease quickly leads to its complete loss.
Symptoms of macular degeneration
If dystrophy develops in the central parts of the retina, it does not go unnoticed. Vision undergoes significant changes. Images of objects lose clarity. Straight lines may appear curved. Pain is not typical for this disease, but increased photosensitivity may occur. Later, a persistent black spot appears in the central part of the visual field and the ability to distinguish colors is lost. The quality of life is significantly reduced due to the inability to read and write, drive a car and control the accuracy of movements.
Macular diseases
Among all the pathologies affecting the macula, several of the most common disorders are distinguished:
- Age-related macular degeneration.
- Macular hole.
- Macular edema.
These diseases cause disturbances in central vision and the development of scotomas.
Age-related macular degeneration
It represents senile degenerative changes that affect the choriocapillaris layer of the choroid of the organ of vision, the pigment layer of the retina and Bruch's membrane. According to its course, the disease occurs in two forms:
- Dry chorioretinal dystrophy: is the initial form of the pathology. It is accompanied by atrophic changes in the pigment epithelium and occurs with a gradual deterioration of vision.
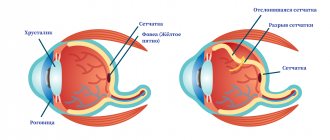
- Wet chorioretinal dystrophy: is an advanced, non-exudative form. In its course, it is more severe and is complicated by detachment of the pigment and neuroepithelium of the retina, as well as the appearance of hemorrhages and cicatricial deformation.
Pathology can develop due to many reasons. The causes of the disease are:
- primary involutional disorders of the macula and Bruch's membrane;
- atherosclerotic changes;
- microcirculation disorder in the choroid;
- the damaging effect of ultraviolet radiation on the pigment epithelium;
- metabolic disease.
The risk zone for AMD includes the following categories of people:
- women whose age has exceeded 50 years and who have light pigmentation of the iris;
- with pathology of the immune, endocrine system, arterial hypertension;
- smoking abusers;
- undergoing cataract surgery.
The main symptom of any disorder of the macular zone is a disturbance in central vision. Most often, patients complain that something appears before their eyes, blocking the image in the central part. Depending on the form of macular degeneration, the symptoms of the disease vary.
Video: Age-related macular degeneration and its treatment
Non-exudative type of pathology
In its course, the dry form slowly progresses. At an early stage, the patient does not notice any disturbances. Visual acuity remains normal for a long time. A sick person is characterized by metamorphopsia. There is a distortion of vision, in which objects are visualized in an incorrect shape, size and spatial location.
The dry form of the disease is accompanied by the formation of retinal drusen, pigment redistribution, the appearance of defects and atrophic changes in the pigment epithelium of the choriocapillaris layer. Due to these changes, a central scotoma is formed: a limited zone appears in the field of vision in which vision is significantly weakened or completely absent. There is a violation of color vision: a person’s brightness, saturation and contrast of the image decrease. The patient may complain of double vision.
Exudative form
The disease occurs in several stages. When the pigment epithelium exfoliates, visual acuity changes slightly. Signs of farsightedness and astigmatism may occur. A translucent spot appears in the field of view, photopsia. A detachment zone is formed in the macular zone, which has clear boundaries.
At the next stage, detachment of the neuroepithelium occurs. The patient notices that his vision is greatly deteriorating. At the stage of neovascularization, vision drops to 0.1 or lower. The patient is unable to read or write. Hemorrhages with the development of hemophthalmos are possible.
Treatment of macular retinal degeneration
In the dry form, patients are advised to take biologically active food supplements. They contain antioxidants, vitamins, lutein and zinc, which prevents the progression of the disease. For this purpose, ophthalmologists prescribe Okuvite-Lutein, Lutein-complex, Vitrum Vision or Complevit Oftalmo. As a complex therapy, drugs that improve regional blood flow are indicated - Vinpocetine, Pentoxifylline.
In the wet form, the ophthalmologist may recommend the introduction of angiogenesis inhibitors into the vitreous cavity. To reduce swelling, subconjunctival injections of glucocorticoids are prescribed. Good results in complex therapy are shown by the polypeptides of the retina of the livestock eye - Retinalamin.
Introduction of angiogenesis inhibitors into the vitreous cavity
Surgical treatment involves removal of the subretinal neovascular membrane during vitrectomy using a standard technique. The intervention reduces the manifestations of metamorphopsia and subjectively improves vision. However, it does not improve visual acuity: most often after surgery it does not exceed 0.1.
Diagnosis of the disease
Macular degeneration is detected and confirmed by the following diagnostic methods:
- Visometry. This is a standard procedure when visiting an ophthalmologist, where central visual acuity is assessed using a table with letters.
- Ophthalmoscopy. This study is aimed at assessing the condition of the retina and its blood supply.
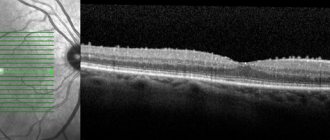
- Optical coherence tomography (OCT). An effective technique that allows you to study the state of optical media and elements of the visual system.
- Amsler test. Analysis of visual images formed on the retina. During diagnosis, a special mesh is used, the distortions of which indicate a probable pathology.
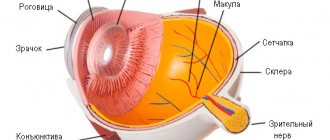
Where does the macula live?
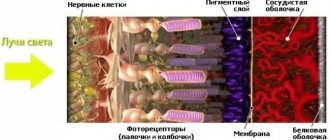
Where light is collected into a beam on the retina of the posterior pole of the eye, there is a yellow spot a little more than 5 millimeters in size. This spot allows each of us to see the surrounding and colorful world as it is. This is the very center of the eye and the center of a person’s worldview; the macula cannot be replaced by the rest of the retina, because the macula is responsible for everything we see.
Yellow because it is colored by the same bright pigments as yellow vegetables - lutein and zeaxanthin. It is painted not at all for the sake of beauty, but to protect against blue light that is aggressive for the eye, to which the cones of the retina react negatively. Cones fill the macula and are responsible for the perception of color and the clarity of vision of objects. Next to the macula, the retina is filled with rods that are also very necessary for us, providing peripheral vision.
There are no vessels in the macula - nothing prevents a person from seeing the world.
Treatment of macular degeneration
Cure and complete restoration of vision with macular degeneration is impossible. However, there are effective methods that can significantly reduce the risk of complications (retinal tears and detachment), as well as reduce the rate of degenerative changes in tissues. The following types of treatment give the best results:
- Laser therapy. The goal of this treatment is to remove pathologically growing vessels and, if necessary, restore the integrity and tight fit of the retina to the vitreous body.
- Photodynamic laser therapy. Laser therapy method combined with the use of photoactive substances. A special composition is injected into the patient’s blood before laser exposure. The photoreagent, deposited in the circulatory system of the eye, destroys pathological vessels under the influence of the beam.
- Inhibitors of agiogenesis factors (VEGF) - Lucentis, Avastin, Aylia. The latest technology that allows you to block the appearance and growth of new blood vessels. As a rule, drugs are administered intravitreally (into the vitreous body of the eye)
With all the variety of treatment methods, it is worth recognizing that patients with age-related macular degeneration cannot do without glasses. In a more modern version, these can be contact lenses and even special electronic devices for the eyes, but the purpose of their use remains unchanged - compensation for lost visual acuity and maintaining an acceptable quality of life. It is also worth remembering regular preventive examinations with an ophthalmologist even after successful treatment, since the risk of relapses and complications remains for life.
Treatment with folk remedies
Alternative medicine recipes are considered as auxiliary methods of therapy. They should never be used as self-medication. It is recommended to use various decoctions and eye drops as folk remedies.
- Oatmeal broth
To prepare the product, you need to rinse 0.5 liters of whole grain. After this, it is soaked for four hours. After time, the water is drained and the grain is poured into a container. Pour 3 liters of water and cook over medium heat, bringing to a boil. The product is boiled for another 30 minutes and filtered through cheesecloth. Take the medicine warm, up to 5 glasses per day. For taste, you can add a teaspoon of honey.
- Calendula infusion
Pour 200 ml of boiling water over 1 tablespoon of the plant’s flowers and let it brew for 15 minutes. The product is cooled, filtered, after which it should be drunk three times a day, ¼ cup. At the same time, 2 drops of calendula infusion should be instilled into each eye. The course of therapy is 6 months.
- Infusion of aloe and mumiyo
50 g of mumiyo are dissolved in 100 ml of aloe juice. The medicine should be taken 10 ml twice a day and 1 drop should be instilled into each eye. The duration of treatment is 10 days.
- Cumin drops
1 tablespoon of cumin is poured into 200 ml of boiling water. Place the product on low heat and cook for no more than 5 minutes. Add 1 tsp. cornflower and mix the ingredients. After this, let it brew for 5 minutes. Instill the resulting medicine 1 drop 2 times a day.
- Celandine drops
1 teaspoon of finely chopped plant is poured into 100 ml of water. Place the product on low heat and keep it for just a few seconds. Infuse and strain the medicine, then put it in the refrigerator. Instill drops three times a day, 3 drops for 30 days.
- Goat milk drops
Mix an equal volume of milk and chilled boiled water. Instill the resulting medicine 1 drop into each eye. After this, the patient puts on a dark bandage and rests for 15 minutes. The duration of treatment is 1 week.
Disease prevention
Prevention of macular degeneration, as a rule, begins when it has already been identified. The purpose of these measures is to reduce the risk of complications and slow down the progression of the disease. It is advisable for persons with a family history to take preventive measures even before the first signs of the disease appear. In any case, it is worth remembering and taking into account factors that can cause the onset and development of degenerative processes in the retinal tissue and follow the following simple rules:
- It is recommended to undergo a preventive examination by an ophthalmologist annually;
- It is necessary to protect your eyes from direct sunlight;
- smoking increases the risk of developing retinal dystrophy because it impairs capillary circulation;
- for an active and harmonious metabolism, a balanced diet is necessary, excluding spicy and fatty foods (fish, nuts, vegetables and fruits are especially useful for vision);
- It is recommended to undergo a course of vitamin therapy twice a year (special vitamin and mineral complexes for the eyes are prescribed);
- It is necessary to lead an active lifestyle, be attentive to endocrine and vascular disorders, and undergo timely treatment for systemic diseases.