According to medical statistics, children suffer from infectious and inflammatory eye diseases much more often than adults. The reasons are quite simple and obvious: infantility and instability of the immune system, lack of strong and automated sanitary and hygienic skills, overcrowding of preschool and school groups, where any infection spreads at the speed of a local epidemic. Therefore, probably any person has encountered a disease such as barley (even if he himself was not sick in childhood, he treated the child). At the same time, there is another disease, similar in some manifestations to barley, but different in essence, clinical picture and prognosis. We are talking about an internal nodular formation in the upper or lower eyelid, which is designated by the Greek term “chalazion” (nodule, hailstone).
The same all-knowing statistics claim that chalazion, unlike barley, is more common in adults - i.e. children, in theory, “shouldn’t” get sick from it. However, they do get sick, and if they have certain predispositions, they get sick quite often and, unfortunately, repeatedly.
Chalazion differs from “regular” stye in its greater density, the absence of purulent discharge (if secondary infection does not occur), less pain or its complete absence, but a significantly longer existence on the eyelid - if the stye, in children most often caused by a staphylococcal bacterial infection, even without treatment can be suppressed by the immune reaction in a few days, then the resorption of the chalazion is sometimes delayed for many months or does not occur at all without medical intervention. Therefore, if you see that the child’s “stye” is not particularly bothered, but does not disappear (or slowly increases) within 1-2 weeks, then it is not a stye, it is most likely a chalazion, and consultation with an ophthalmologist is necessary.
What is a chalazion
The eyelid has a huge number of glands that secrete fluid. Moisture prevents the mucous membrane from drying out when the volume of secreted tear fluid is not enough. Exposure to internal and external factors leads to blockage of the gland, which due to this significantly increases in size.
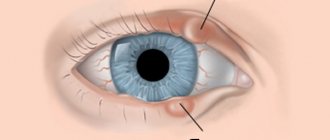
Chalazion of the upper/lower eyelid in a child
Liquid accumulates and becomes cloudy. Its consistency becomes viscous and eventually hardens. The size of the swelling stops increasing when moisture is no longer supplied. The tumor is easily palpable and visualized. Thus, the chalazion appears in the soft tissues of the eyelid in the form of a hard ball.
The swelling has clear boundaries. It does not harm human health. This defect may persist for many years. The patient himself decides whether to remove the accumulation or not.
It's another matter when liquid continues to flow to the node. In this case, the tumor continues to grow, taking on enormous dimensions. This process is accompanied by severe pain and blurred vision. Chalazion in this form requires immediate intervention from a specialist.
Symptoms
At the initial stage, a chalazion can easily be confused with a stye. Distinctive signs become noticeable as the disease progresses. The clinical picture is as follows:
- A small, round and movable seal - a neoplasm located in the cartilage tissue is not fused to the skin in any way, due to which it “rolls” during palpation.
- Absence of pain symptoms - the affected tissues on the inside of the eyelid become red and itchy, causing profuse lacrimation and irritation of the cornea, but no pain syndrome is observed.
- Diameter up to 6 mm - the formation grows very slowly, but as it increases, swelling of the surrounding tissues is noted.
Important! A neglected chalazion degenerates into a cyst. This significantly increases the risk of developing a purulent process, and subsequently the occurrence of a fistula. Spontaneous release of purulent masses is often accompanied by severe pain, a sharp deterioration in health and an increase in temperature.
Signs of pathology
A chalazion of the lower eyelid develops gradually in a child. Symptoms appear after a while. In order not to start the disease, it is recommended to consult an ophthalmologist at the first signs.
Symptoms that appear with chalazion:
- Swelling.
- Redness around the eyelid.
- A yellow, dense nodule, similar to a stye, on the eyelid.
- Increased secretion of tear fluid.
It is important to listen to the child's complaints. Children can say for themselves that they have a burning sensation in their eyes, their skin is constantly itching, or they often have a headache.
Clinical course of blepharitis in children
One of the main symptoms of blepharitis is severe itching in the eyelid area. Parents may notice that the child constantly scratches his eyes, despite repeated requests from adults not to do so. Objectively, you can notice redness and swelling of the edges of the eyelids, as well as constant lacrimation. The child will constantly complain of severe itching or say that there is a speck in his eye.
With scaly blepharitis, small scales may appear in the eyelash growth area. The skin underneath will show signs of inflammation.
The ulcerative form of the disease is characterized by the formation of purulent crusts on the eyelids. If a child tries to scratch them off, he will remove the scales along with the eyelashes, and in the place where the crust was, a small ulcer will appear that may bleed.
In addition to local symptoms, the child may have signs of general malaise. If he is not provided with qualified assistance in a timely manner, then in the future the disease may become chronic and have a negative impact on the baby’s vision. Also, the inflammatory process can spread to neighboring organic structures and provoke the occurrence of more serious ophthalmic pathologies.
Causes of chalazion in a child
Chalazion of the lower eyelid in a child begins due to blockage of the sebaceous glands in the tissues of the eyelid. The inflammatory process begins to actively develop under the accumulation of secretion.
Most often, the pathology is observed in children 5-10 years old. Another reason for the appearance of the disease is infection. Harmful bacteria and other microorganisms penetrate the mucous membrane of the eye through dirty hands, stale towels or bed linen. The disease can be caused by bacteria such as streptococci and staphylococci.
Factors leading to chalazion in a child:
- Increased production of sebaceous secretions.
- Chronic inflammation of the eyelid margin.
- Diabetes.
- Vitamin deficiency.
- Diseases of the stomach and intestines.
- Decreased functioning of the immune system.
- Recent flu or acute respiratory viral infection.
The constant occurrence of chalazion makes you think about your health status. The disease becomes chronic due to pathological processes in the body. Therefore, the return of the disease in a child is a reason to conduct a full examination.
Doctor Komarovsky's opinion on the etiology of the disease
Komarovsky E. O. does not differentiate the causative factors of chalazion pathology into adults or children. Diseases of dirty hands, hormonal disorders, lack of treatment for diseases of the mucous membrane are common to people of any age.
Among the common etiological factors it is worth highlighting:
- disruption of the intestinal microflora and general immunity with the provocation of dysbacteriosis, local skin phenomena, which can increase the risk of developing chalazion;
- hypothermia of the body, draft;
- violation of the acid-base balance of facial skin;
- skin type with increased oily content in adolescence with excess sebum production and lack of personal hygiene;
- hormonal disorders in the body (thyroid pathology, diabetes mellitus);
- frequent respiratory diseases;
- hypovitaminosis, lack of a balanced diet;
- violation of the basal metabolism;
- chronic diseases of the gastrointestinal system;
- lack of preventive examinations by a pediatrician or ophthalmologist, irregularity of treatment;
- tendency to allergic reactions.
Komarovsky notes that the incidence in children aged 5-8 years due to the lack of the concept of personal hygiene, visiting children's groups, and the development of immunity in children.
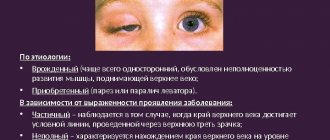
Types and stages of the disease
Chalazion, depending on its location, is divided into 2 types: upper and lower. The first type is characterized by the formation of nodes on the edge of the upper eyelid. When it forms, the patient feels severe discomfort and itching. It always feels like something is in my eye. The disease on the upper eyelid goes away on its own in 2-3 days.
A chalazion of the lower eyelid in a child is very similar in appearance to a stye. The tumor appears near the eyelash line. Requires treatment that can be done at home. Therapy for a node that appears more deeply takes much longer. This requires 2 weeks.
The stages of chalazion development are conventionally divided into:
- The occurrence of discomfort and redness around the affected area. At this stage, the disease is no different in appearance from barley.
- Formation of a hard knot that causes severe pain. Over time it grows to a huge lump. This stage requires immediate intervention. Most often, it is enough to use improvised means for treatment.
- Cone growth. This takes a long time, from 2 weeks. The process can be stopped by taking special medications.
- Advanced disease, prolonged enlargement of the lump, or infection in the affected soft tissue require more serious measures. To get rid of a chalazion, they resort to surgery, which is performed on an outpatient basis. After removal, no traces remain on the eyelid.
Why should you see a doctor?
A chalazion is a capsule containing purulent exudate with a colony of pathogenic microorganisms. If it opens, the liquid comes out partially. Dry residue, bacteria and hardened sebum will remain inside the capsule. As a result, the wound will not heal until the purulent canal is completely cleaned. In the worst case, a number of complications will arise:
- secondary infection;
- conjunctivitis;
- blepharitis;
- damage to the lacrimal sac;
- deterioration of visual acuity, clouding of the transparent media of the eye;
- relapse of pathology.
IMPORTANT. If pus and bacteria get on the cornea, they can cause clouding, leading to partial or complete loss of vision.
Therefore, it is necessary to consult a doctor to completely clean the wound and prescribe antibiotics. If the chalazion continues to grow, the large tumor cannot be cured with drug therapy. Surgical intervention will be required, in which the presence of specialists is required.
Possible consequences of a burst lump on the eye
In most cases, in the absence of timely treatment, chalazion leads to the following complications:
- Development of an abscess inside the capsule. In this situation, purulent exudate does not come out and continues to accumulate in the subcutaneous fatty tissue of the eyelid. It has a toxic effect on soft tissues, leads to an ischemic process, and increases the risk of necrosis.
- Corneal phlegmon. Occurs when purulent contents enter the eyeball or mucous membranes. The pathology requires immediate medical intervention due to the high risk of septic shock.
- Frequent relapses. Various types of microorganisms penetrate into the ruptured chalazion. The disease is chronic. Large colonies of bacteria do not respond to antibacterial therapy, so they continue to multiply and clog the lumen of the sebaceous gland. As a result, new formations appear in its place that need to be cleaned.
Features of the upper and lower chalazion in a child
The causes of nodules on the upper and lower eyelids are the same. The difference between the two types lies only in the manifestation of pathology. The upper chalazion becomes noticeable almost immediately, and a thickening appears quite quickly. It develops much faster than with the lower form of the disease.
This feature helps to quickly get rid of defects on the upper eyelid.
At the bottom, only an experienced specialist can quickly determine the onset of tumor formation after a complete diagnosis. During the first few days, the onset of the disease does not show itself at all. Chalazion of the lower eyelid requires immediate initiation of a therapeutic course. It takes longer to mature and resolves on its own in rare cases.
Diagnostics
An ophthalmologist with high qualifications and extensive experience is able to determine the presence of the disease after examining the patient. The beginning of the development of the disease in the child’s eye is indicated by the appearance of a dense point and a change in the shape of the eyelid. These symptoms help diagnose chalazion without the use of special tools and equipment.
In special cases, laboratory tests are used. This approach is most necessary for chronic manifestations of the disease. The test results allow us to exclude the possibility of a malignant tumor.
Chalazion of the upper eyelid in a child can be detected using the following studies:
- Immunogram.
- Examination of eyelashes for the presence of demodicosis.
- Blood, urine and stool analysis.
The possibility of a chalazion reappearing becomes small if the cause has been identified and eliminated correctly.
Treatment
At the beginning of the development of nodes, the disease can be effectively combated using folk recipes. This approach does not work for chalazion in the progressive stage. The advanced form of the disease can only be treated surgically. Timely therapy and correct diagnosis will avoid surgery.
Medicines, gels, ointments, eye drops
Conservative treatment is effective only until a hard capsule forms. In other cases, only surgery can save you. Ophthalmologists prescribe ointments and drops for chalazion in a child. The most commonly used are Levomekol, corticosteroid ointment or hydrocortisone.
In addition, a course of antibacterial therapy is prescribed. The product is aimed at relieving inflammation and swelling, getting rid of suppuration and normalizing the functioning of the sebaceous glands of the eyelid. The use of the drug in this form is difficult. It is extremely difficult to put ointment under the eyelid of young children. It is very difficult for them to endure such an event.
The problem can be solved by the correct psychological attitude of the child, which the parents must create.
As for the drops, the antibiotic drug is dripped into the child’s eyes. Depending on the situation, the doctor prescribes the use of combination therapy, which consists of using an antibacterial agent with corticosteroids. This approach allows you to remove swelling of the eyelid, redness of the skin and relieve pain.
Which drops are effective in treating the disease:
- Tsipromed. Has anti-inflammatory and antiseptic effects.
- Normax. It is aimed at combating bacteria and has a wide spectrum of action.
- Phloxal. Gives good results in getting rid of harmful microorganisms. I take it in a course, the maximum duration of which is exactly 14 days.
- Maxidex. Has anti-allergic and anti-inflammatory effects.
- Tobrex. Has a powerful disinfectant effect. Allowed to take for no more than 7 days.
It takes 7 to 14 days to completely get rid of the disease. If no improvement is observed during this time, then the chosen treatment method is ineffective. It is important not to let the disease progress and to change the approach as early as possible. Typically, a specialist recommends taking stronger medications or corticosteroid injections into the resulting lump.
Intracavitary drug injections
Having confirmed the diagnosis of chalazion in a child after a careful examination of the eye and ordering general tests, the doctor decides on therapeutic methods. In special cases, a course of injections into the soft tissues of the eyelid is used.
The injection course technology is performed as follows:
- For the procedure, a room is prepared where the medicine will be injected under the skin.
- The use of the drug for eyelid anesthesia during injection is not intended.
- The specialist thoroughly disinfects the lower and upper eyelids with an antibacterial agent.
- The drug is injected into the cavity of the formed node using an insulin syringe. The needle should be so thin that the child will not feel pain.
- After the injection, there should be no traces of the procedure left on the surface of the skin.
Finally, the ophthalmologist gives the patient basic recommendations for caring for the treated eye. Parents should strictly follow the doctor's advice.
Chalacion injection therapy in children produces a positive effect in half of the cases. Advanced forms with complications cannot be cured by introducing a hormonal agent into the source of inflammation. Cases where injections do not give the desired effect are subject to surgery.
Operative measures to treat the disease
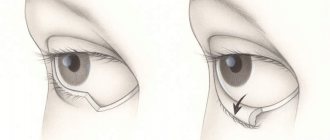
If all tried methods of treating the disease have failed, you have to resort to surgical removal of the formed node. The operation is not serious; it is performed using local anesthesia of the eyelid. The duration of the manipulations is only 20 minutes.
During the process, the specialist makes an incision in the skin of the inner side of the eyelid. After pumping out the accumulated fluid and the resulting pus, 1 to 2 stitches are placed. Finally, apply a bandage tightly. After surgery, there is no need to go to the hospital to monitor tissue recovery. The node is removed on an outpatient basis.
The patient goes home a few hours after the procedure. Before the stitches heal, you need to apply anti-inflammatory ointment to the area and drop drops into the eye. The first time after surgery, the eyelid will be red and slightly swollen. After 2-7 days, the eye will return to its normal appearance. Due to its size, the seam will be almost invisible.
Treatment with folk remedies
Home recipes, proven over the years, can cure chalazion in children only at the initial stage. You can use traditional medicine after consultation with a specialist. Parents note several remedies that give good results in the fight against the disease.
At the initial stage, you can get rid of the symptoms of chalazion with the help of:
- Aloe juice in drops. It is diluted in equal proportions with water. Drops of natural origin should be taken 5-6 times a day.
- Cabbage compress. Separate the egg white from the yolk and mix it with finely chopped cabbage. For the base of the compress, take gauze or any fabric folded several times. Mixed products are wrapped in the prepared material. The liquid should not ooze through the rag, but only slightly saturate it. The compress is applied to the sore eye so that the cabbage juice touches the inflamed eyelid.
- Dried dill seeds in a compress. The raw materials are brewed, pour 2 tbsp. l. water. The mixture is sent to the fire and brought to a boil. The result is a homogeneous mass. It needs to be cooled and placed in a cloth. The compress is applied to the affected area.
How to cure diseases using Dr. Komarovsky’s method?
According to the popular pediatrician, Dr. Komarovsky, a chalazion that appears in a child is not as serious a disease as ophthalmologists say it is. The use of complex therapy is required in only 3 out of 4 cases of the disease. According to statistics, 25% of inflammatory processes go away on their own.
In some cases, a course of massage of the glands is sufficient for uncorking. But at the same time, the small patient should still be observed by a pediatrician. The condition may worsen and then urgently require drug treatment.
Evgeniy Olegovich has a negative attitude towards the use of traditional medicine recipes. He believes they are only effective in reassuring parents. The doctor advises using reciniol emulsion or yellow mercury ointment for treatment. This therapy is aimed at getting rid of harmful microorganisms that cause inflammation and the formation of lumps in the tissues of the eyelid.
Physiotherapeutic treatments
Chalazion in a child in its early stages can be treated with physical therapy. This therapeutic approach allows you to reduce a small tumor on the upper eyelid, get rid of pus and cure the disease completely.
Physiotherapy methods used for treatment are presented in the table:
| Name | Peculiarities |
| UHF | The therapy is based on the effect of an ultrasonic frequency electric field on the affected area of the eye. This leads to heat generation inside the tissues. The method is often used in combination with massage. The procedure has contraindications. It cannot be performed for chalazion in an advanced stage and severe inflammatory processes. |
| Magnetotherapy | The method involves exposing the diseased eye to a low frequency magnetic field. |
| Electrophoresis | The procedure uses an electric field in combination with drug therapy. |
| Phonophoresis | This type of physiotherapeutic therapy is characterized by the parallel use of ultrasound and medications. Its main advantage is that vibrations of ultrasonic waves contribute to better absorption of medications applied to the inflamed eyelid. At the same time, the rest of the skin surface remains untouched. |
How to treat blepharitis in children?
Modern methods that are most effective are used to treat the disease. Treatment tactics are always determined only by an ophthalmologist. To do this, it is necessary to accurately establish the causes and form of the disease.
It must be remembered that treatment of blepharitis should not be limited to the initial relief of symptoms. You cannot stop taking medications without permission without first consulting an ophthalmologist, so as not to provoke the development of relapses and the transition of the disease to a chronic form.
During therapy, the doctor may raise the question of the advisability of using not only local antibacterial agents, but also general antibiotic therapy. This is usually associated with the appearance of abscesses (fibrous capsule with purulent exudate). In this case, the following drugs may be prescribed: oxacillin, ampicillin, sulbactam, amoxicillin and others. It may also be necessary to surgically open the abscess.
In case of a protracted course of the disease, tetracycline tablets are prescribed orally, the course of treatment is usually 1-1.5 months. In addition to the main therapeutic effect - the destruction of the infectious pathogen, one can also note its effect on the secretory activity of the meibomian glands. Any antibacterial agents are used strictly on the recommendation of a doctor after preliminary identification of the source of the pathogen, so self-medication with antibiotics “blindly” will most likely not bring the desired result.
Local medications that contain corticosteroids are not used in long courses to avoid side effects.
Nonsteroidal anti-inflammatory drugs are used if there are signs of chronic blepharoconjunctivitis of a non-infectious nature. The drugs most often prescribed in this situation are indocollir or diclofenac.
The well-known pediatrician Komarovsky in Russia dedicated one of his programs to this topic.
What to do if the chalazion ruptures?
A neoplasm with a chalazion can burst at any time. Therefore, if you get sick, it is important to know what to do in this case. The first thing you need to do is treat the abscess with an antiseptic. This will protect against the spread of infection and pathological microorganisms found in the pus. For antibacterial treatment of the resulting wound, tetracycline ointment and Chlorhexidine are used.
In case of a serious inflammatory process, it is recommended to instill Albucid or Tsipromed into the eye.
Drugs that are used for ruptured seals on the eyelid:
- Dexamethasone. Makes the appearance of the skin of the eyelid normal, relieving puffiness.
- Diclofenac in the form of eye drops. Stops the inflammatory process and relieves pain.
- Levomekol in the form of an ointment. The accumulated pus is drawn out from the wound and has a powerful antimicrobial effect. The ointment is used for compresses, which are applied to the formed abscess. It is kept overnight.
- Boric acid solution 2%. Kills bacteria harmful to the body. The product is applied to the problem area of the skin 3 times a day.
- Floxan ointment. Reduces the risk of secondary infection by destroying pathogenic microorganisms. The drug is placed under the eyelid 2 times a day. The duration of treatment is 2 weeks.
To alleviate the child's condition, some parents use folk recipes. They especially note the effectiveness of the infusion of marshmallow rhizome and aloe pulp applied to the damaged area.
Causes
Eyelid sores can be divided into two categories: those that appear on the outer part of the eyelid (top and bottom) and those that appear on the inner side.
Allergic reactions
Allergic reactions occur when the body's immune system reacts to substances in the environment that are harmless to most people. These substances are called allergens, and they include certain foods and medications, insect bites, cosmetics and more. When they are ingested, inhaled, injected, or come into contact with the skin, the body may react by developing small bumps filled with fluid. After some time, itching or swelling occurs, which can leave painful bumps or sores on the eyelids.
Barley
A stye is a tiny, painful lesion on the inside or outside of the eyelids filled with pus. Appears along the edges of the eyelids, which have been infected with bacteria (staphylococcus).
Because this infection occurs inside the eyelids, it clogs the eye's oil glands, resulting in pus-filled lumps. After the pus drains, an open wound remains on the eyelid.
Prevention of chronicity of the process
Chalazion in a child can lead to serious consequences. Therefore, it is recommended to pay special attention to preventive measures. This must be approached responsibly, because the frequency of relapse of the disease in children is much more common than in adults. The task of parents is to teach their children simple rules of prevention.
Following them will help not only protect the child from chalazion, but also prevent the development of many eye diseases.
Washing hands with soap
What parents should know for prevention:
- Wash your hands and face with soap. It is important to carry out this procedure after interacting with other children, walking and going to the toilet, as well as before eating.
- Eat a balanced diet. The diet should be complete and contain the required amount of vitamins and minerals.
- Vitamin supplements. In addition to vegetables and fruits, the child should take a vitamin complex. This will help the body receive the required amount of nutrients. It is best to use multivitamin preparations. They do the job well and are inexpensive.
- Good for treating colds. The child should not become hypothermic. It is important to treat all diseases to the end. The remaining symptoms can transform the disease into a chronic form. This has a detrimental effect on the immune system, the weakening of which will not be able to protect against chalazion.
The small size of chalazion nodes in a child does not mean that the disease is harmless. Inflammation of the upper or lower eyelid can cause serious consequences and lead to the development of severe complications. The problem can be solved by consulting a doctor and a thorough examination, which will help you choose the right treatment tactics.
What methods can be harmful in childhood?
To effectively treat chalazion in a child, it is important to follow the rules of personal hygiene and doctor’s recommendations so as not to harm the baby:
- observe the frequency and dosage of eye drops and ointments recommended by the doctor - reduced concentration of the drug for children;
- do not self-medicate, using alternative medicine methods and warming with compresses;
- do not try to open the capsule yourself - this may cause a secondary layer of pathogenic microflora with subsequent suppuration;
- self-administer medications.
Komarovsky advises that in order to prevent negative reactions, consequences, and complications from the visual apparatus, it is necessary to seek medical help. The doctor will help you choose the optimal treatment regimen to eliminate the chalazion in a short time.