Despite the rapid methodological and technological development of ophthalmology in recent decades, the problem of childhood myopia (myopia) still does not lose its severity and relevance. As a critical period, which accounts for the largest number of requests on this matter, some sources indicate the age interval from 5 to 12 years, others associate it with the beginning of pubertal processes and refer it to the stage of 8-15 years. However, most experts agree that the proportion of children with myopic refractive error is unacceptably high, and estimate the incidence at an average level of 35-40%.
These age intervals are especially dangerous because, against the background of rapid growth and incipient hormonal changes, myopia tends to rapidly progress, which, in turn, is fraught with the development of organic changes and severe complications in the visual system, up to complete loss of vision.
There are a number of methods for correcting myopic vision in childhood, ranging from optical to surgical. Scleroplasty surgery allows you to stop the progression of myopia without, however, restoring normal visual acuity. This limitation of the predicted result is one of the main, but not the only reason for the ambiguous attitude of specialists towards this technique; In general, scleroplasty in pediatric ophthalmic surgery is a controversial method.
Why is severe myopia dangerous?
Myopia progresses mainly due to a violation of the structural and biochemical properties of the sclera, and a defect in its biomechanics develops. This determines the pathogenetic orientation of operations to strengthen the sclera with severe myopia.
Sclera-strengthening operations have been studied and improved for more than 80 years, but the problem of treating progressive myopia has not yet been solved. Statistics indicate this: the stabilization effect after surgery is maintained in 32-100% of cases, which is a very wide limit.
With severe myopia in children, traditional scleral strengthening operations are often useless, so medicine is working on an optimal and simple technique.
Axial myopia provokes stretching of the equatorial region of the sclera, although changes in one of the four quadrants of the eyeball are possible.
Finding out the quadrants where scleral stretching predominates is necessary in order to determine the zones of influence during scleroplasty. Most often, an increase in the anteroposterior size of the apple is combined with increased tensile stress in the meridional direction along the Y axis and compressive stress in the equatorial direction along the X axis.
The change in the direction of stretching in patients with myopia is due to a violation of the structure of the scleral tissue. Loosening of collagen fibrils occurs, the spatial structure of proteoglycan components in intercellular substances is disrupted, and insufficient intermolecular bonds are formed in the connective tissue.
Myopia is based on a violation of the density of collagen fibers; the structure, composition and method of interconnection of connective tissue components (intercellular matrices) changes. These changes reduce the biomechanical stability of the sclera.
Progressive myopia is the main reason for limiting professional choice; it poses a serious danger, as it is fraught with serious complications. Often myopia ends in complete blindness.
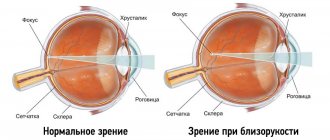
How vision problems develop
Myopia is an eye disease in which objects located at close distances are clearly visible. If they are further away, the image becomes blurry. This happens due to the elongation of the eyeball. Rays of light that come from objects normally converge on the retina. With myopia, they join in front of it. A blurred image of the object appears on the retina. Another name for the disease is myopia. Among the reasons that influence the development of myopia are hereditary factors, weakening of scleral tissue, muscles, eye strain from unfavorable living conditions.
Features of scleroplasty
The term “scleroplasty” unites a group of operations that help stop the development of myopia. In the CIS countries, this method is considered one of the best for severe myopia. The operation involves strengthening the back of the eye and improving blood supply.
Scleroplasty is an ophthalmic procedure that helps strengthen the outer layer of the eye, the sclera. Modern ophthalmology is developing this area of medicine, so there are different modifications of scleroplasty. They differ in the type of tissue that is subjected to surgery and in the technique.
In general, each modification of scleroplasty implies a slowdown in the progression of myopia in patients who are already at risk. The operation does not improve vision, but only stabilizes myopia to prevent complications.
Scleroplasty in children is performed with rapid progression of myopia, which is caused by severe changes in the shape and size of the eyeball. Medicine considers rapid progression to be a deterioration in visual function of one or more diopters per year. This determines the fact that the operation is often performed on children and adolescents: their eyeballs are constantly growing, their shape changes to elliptical.
Most often, surgery is prescribed for patients with moderate and high myopia, that is, with visual acuity indicators of -4, -6 and above. Doctors recommend the operation be performed between seven and sixteen years of age.
When choosing a specific technique, the doctor is based on the patient’s age and the degree of myopia. It is recommended to start with minimally invasive operations. If a positive effect is not achieved, more complex technology is required.
Scleroplasty is not an alternative in the treatment of myopia in adults and children. Conservative and hardware treatment are the basis of therapy for myopia, while surgery is a prevention of deterioration of the eyeball.
The operation will not help the child see better; it will only stop the progression of myopia. Therefore, conservative treatment is indicated after scleroplasty. The operation is widely used only in the CIS countries, since the technique has been poorly studied in Europe.
Postoperative period
After scleroplasty, you need to be at rest for two to three hours, then the eyes are examined by a surgeon. If there is no inflammation, the patient is discharged home. The rehabilitation period ranges from 15 to 30 days (depending on the type of scleroplasty). For the first few days, it is recommended to use a protective blindfold, which must be changed every day. After it is removed, you need to carry out a two-week course using antibacterial and anti-inflammatory drops. After completing the recovery period, you must see a doctor. He will examine your eyes to make sure they have healed well and there are no additional problems.
Operation efficiency
When studying the effectiveness of scleroplasty, the immediate and long-term results of the operation were analyzed in 125 children aged 8-16 years. The patients had progressive myopia from 3 to 9 diopters.
Scleroplant-M was used as a biomaterial; operations were performed in Russia. Patients were divided into groups according to the length of the anteroposterior axis of the eyeball (the deformation that occurs with myopia).
The study showed that children easily tolerate scleroplasty, complications are extremely rare (swelling of the conjunctiva, hyperemia).
There was no noticeable improvement in vision after surgery. On average, the indicator could increase by 0.05 units. It was found that scleroplasty improves the functionality of the accommodative apparatus by increasing the reserve of relative accommodation.
When examined one year after surgery, it was revealed that in patients with an eyeball size of up to 25 mm, myopia stabilized in 96.2% of cases. In children with an anteroposterior eye size of 25-26 mm, the disease stopped in 93.5% of cases, and in patients with an anteroposterior eye size of 25-26 mm, an effective result was observed in 75%.
After 2.5 years, children with an eyeball of 25-26 mm showed no changes in refraction. The indicator increased only in patients with an eye larger than 26 mm.
2.5 years after surgery, myopia stabilized in 80.8% of cases in patients with 25 mm of the eyeball and in 77.4% in children with 25-26 mm.
Examination before surgery
An ophthalmological examination is carried out before scleroplasty and after surgery. The patient's condition must also be monitored for three years.
Diagnostic methods:
- Visometry. Selection of correction using a sign projector.
- Biomicroscopy. The study reveals inflammation in the eye. Inspection can be carried out in several ways: direct focusing, reflected light, indirect illumination, reflective zones.
- Refractometry (skiascopy). The refractive power of the eye (refraction) is examined in the first half of the day. Before the procedure, you need to instill an atropine solution for three days. Refraction can be analyzed using an autorefractor; when the pupil is dilated, the fundus of the eye is examined with an ophthalmoscope. Changes are recorded in each eye separately.
- Echobiometry. The test allows you to measure the anteroposterior size of the eyeball, the depth of the anterior chamber, and the thickness of the lens. A fivefold measurement is required, the fifth being considered true.
Execution method
Scleroplasty involves mechanical strengthening of the eye frame and revascularization (restoration of blood vessels) of the sclera. The operation allows you to normalize metabolism in the choroid and retina, and slow down changes in myopia.
Indications for scleroplasty:
- Progressive myopia: an increase in the anteroposterior axis of the eyeball (with an eye length of 24 mm or more), vision deterioration by 0.71-1 diopter per year (with myopia of 3 diopters or more).
- Stable myopia: visual impairment with worsening chorioretinal dystrophy.
- Slow myopia: an increase in the anteroposterior axis, a deterioration in visual acuity by 0.5-0.75 diopters per year.
Contraindications:
- Chronic eye infections (acute stage).
- Acute inflammation.
- Severe thinning of the sclera.
- Scarring of the conjunctiva or Tenon's capsule after injury or burn.
- Age up to 8 years (relative contraindication).
During scleroplasty, a special graft is used, which is represented by sclero-strengthening material. It is obtained from biological tissues or prepared synthetically. The material must be processed and cleaned.
Scleroplasty is performed under local anesthesia on an outpatient basis. Often both eyes are operated on at once. The operation involves inserting flaps of material onto the back wall of the eye to strengthen the sclera. This material will fuse to the outer shell, strengthening the back wall of the sclera, accordingly, preventing changes in the shape of the eyeball.
After the operation, the graft is replaced or grows with connective tissue, forming a single system of sclera and material. This system increases biomechanical stability by stabilizing the ocular membranes and strengthening the shape of the eyeball.
The entire operation takes 20-40 minutes. Over time, the scleral reinforcement flap fills with blood vessels, which improves blood circulation in the eye. Scleroplasty is often supplemented with laser vision correction.
After scleroplasty, the child should be under the supervision of an ophthalmologist. Monitoring the condition of the eyes and timely prevention of complications and relapse are required.
Surgical technique
Under general or local anesthesia, after careful preparation of the surgical field, several incisions are made in the outer membranes of the eye - the conjunctiva and Tenon's membrane. Scleral-strengthening flaps are inserted into the resulting pockets and secured.
Allosclera, dura mater, tendon, and synthetic materials such as hemostatic sponge, silicone, and mersilene mesh can be used as flaps.
Photo: https://pixabay.com/photos/medicine-treatment-human-3262293/
Subsequently, these flaps, as a result of aseptic inflammation, practically grow into the eyeball, preventing its stretching, blood vessels grow to them and the nutrition of the eye improves. Continuous or interrupted sutures are placed on the conjunctiva in the area of the pockets, which subsequently dissolve on their own or are removed by the surgeon after 7-10 days.
Types of scleroplasty
In modern ophthalmology, various modifications of scleroplasty are used. They may differ in the type of scleral tissue being operated on, in the method of introducing the graft, and in the type of fastening.
Scleral strengthening operations can be divided into groups:
- Banding, tunnel.
- Free (collagenoplasty, meridional surgery, sclera-strengthening injection).
Based on the degree of invasiveness, a distinction is made between minimally invasive (small) and bandaging (large). There are also simplified operations. Today, simple free techniques are most often used that do not fix the graft very rigidly.
The simplest technology is collagenoplasty: through a small incision in the sclera, liquid gel-like collagen is injected under the Tennon's capsule (the posterior part of the eyeball).
Types of scleroplasty based on complexity:
- Simple operation. Incisions are made in the eye shell through which a natural or polymer composition is injected into the back of the eye. This compound can be developed in a laboratory or extracted from a patient's cartilage or blood. The composite hardens, limiting deformation of the eye shape. The procedure does not harm the muscles or any other elements of the eyeball.
- The operation is of medium complexity. It involves inserting strips of polymer material behind the back wall of the eye. The material can be synthetic (silicone, metal-plastic) or natural (part of the brain membrane, fascia, donor sclera). The flaps should go around the eye like a bandage and prevent the eyeball from growing.
- Complex. The operation involves the use of many connecting elements. It requires cutting the muscles that rotate the eye to place the material in the desired location. After fixing the strips, the muscles are sutured.
The technology of scleroplasty is considered simple, but the outcome of the operation will depend on the stage of myopia, the experience and qualifications of the doctor, and the individual characteristics of each patient.
Distraction scleroplasty
It is precisely such disturbances in the outer equatorial region of the sclera, such as a decrease in tensile stress along the equator of the eyeball, that led to the development of a new method for treating myopia.
Distraction scleroplasty allows you to change the direction of tension in the equatorial part of the sclera with progressive myopia. The operation improves blood circulation in the tissues of the eyeball without the formation of stagnation.
When comparing the sclera of the eye after distraction scleroplasty and conventional surgery, a pronounced sclero-strengthening effect of the new technique is noted.
Advantages of distraction scleroplasty:
- improved fixation of the graft on the surface of the sclera;
- decompression of the outer equatorial region, ensuring tissue regeneration after inflammation;
- stimulation of fibrillogenesis.
Distraction scleroplasty combines the advantages of traditional techniques and provides the best effect. The operation improves the condition of the membranes and the functionality of the eye in case of myopia.
Scleroplasty according to Snyder-Thompson
This is a complex surgical procedure that makes it possible to strengthen the back wall of the eyeball. One strip of the implant is passed through the projection of the macula (the center of the retina), near the optic nerve head. The end of the strip is sutured to the sclera on the other side. It turns out that the graft passes from top to bottom under the muscles, covering the place where the macular area is projected onto the sclera.
Scleroplasty according to Snyder-Thompson provides 70-85% of the stabilizing effect.
However, this operation is much more dangerous than other techniques. This is due to the fact that the graft is carried out to the posterior pole of the eye near important vessels and the optic nerve. Subsequent tension may well injure the neurovascular bundle. When the graft is displaced, pressure occurs on the eye muscles, impairing their functionality.
Scleroplasty according to Pivovarov
The Pivovarov operation involves the use of several grafts. They are inserted in four quadrants under Tenon's membrane, further along the sclera to the back wall of the eye. Where the graft touches the sclera, aseptic inflammation occurs, during which connective tissue is formed. It strengthens the eye, increasing its elasticity and improving blood circulation.
The Pivovarov operation mostly strengthens the equatorial zones of the eye, with less effect on the posterior regions. With progressive myopia, 50-60% of the stabilizing effect is provided.
Most often, after surgery, an allergic reaction to sclera-strengthening material develops. Tenonitis (inflammation of Tenon's bursa) and episcleritis (inflammation of the episcleral tissue) are also sometimes observed.
Methods of performing surgery in children
Scleroplasty is an operation performed under local anesthesia or general anesthesia. The patient is sent home within a couple of hours after it is completed. The duration of the operation to stop myopia depends on the method of its implementation and can range from half an hour to 50 minutes.
Methods for performing eye surgery differ in the technique used, the material used and its quantity. Based on these features, we distinguish:
- Simplified scleroplasty. During its implementation, up to 6 micro-incisions are made in the sclera and sterile biogel is injected using a syringe;
- Synthetic or natural. When the gel hardens, it prevents the growth of the eye wall and its pathological growth.
- Scleroplasty using the Pivovarov method. 4 incisions are made through which microflaps made of reinforcing material are inserted - metal-plastic, silicone or donor sclera; the operation is completed by suturing. After some time, the transplant fuses with the outer shell, its posterior part is strengthened and the growth of the eye along the long axis slows down.
- Snyder-Thompson method. 5-7 incisions are made and a fairly large amount of a strengthening substance is introduced, and during it a temporary dissection of the oculomotor muscles is made to introduce the material. At the final stage, sutures are applied to the conjunctiva.
- Complex scleroplasty. This is a major ophthalmic intervention: a plate is placed near the macula and optic nerve.
What can be the complications after scleroplasty?
Any surgical procedure can be dangerous for the patient. Scleroplasty was no exception. The operation has risks and possible complications, although it is a low-traumatic procedure.
Complications after scleroplasty occur very rarely. One of the most common is an allergy to scleral strengthening material. The reaction to foreign material can be stopped.
Sometimes after scleroplasty, the flap is displaced when its fixation is not strong enough. A sign of this complication will be swelling on the conjunctiva. To correct the defect, the operation is repeated, the flap is replaced or the old one is strengthened.
Risks and complications
The scleroplasty procedure is a low-traumatic operation, but large-scale and may be accompanied by certain risks and complications. These include:
- Transplant displacement. This occurs due to weak fixation of the reinforcing plates to the posterior wall of the eyeball. The condition is accompanied by redness, pain in the eye, and a feeling of a foreign body inside. The situation is corrected by repeated corrective surgery.
- Allergic reaction. It can occur in 2-5% of cases of scleroplasty operations, despite the fact that the transplanted material is made of hypoallergenic inert materials. To stop the process, anti-inflammatory and antihistamine drugs are prescribed. If the therapeutic effect is insufficient, the material is promptly replaced.
- Transplant rejection. Happens in 3% of all scleroplasty operations. The situation necessarily requires a repeat operation during which the surgeon replaces the existing graft with a substance of a different origin.
Rehabilitation for myopia
After scleroplasty, a woman can give birth naturally. Compensating for myopia becomes a reason not to have a cesarean section if your vision is poor.
The operation to strengthen the sclera does not limit the patient in everyday life. Children can return to school 10 days after the procedure. Visiting the pool is allowed a month after scleroplasty, and sports after 14 days.
The patient is prohibited from putting stress on his eyes for 2 years after surgery. Moderate and heavy physical labor should be avoided. This way you can avoid complications.
Indications and contraindications
Scleroplasty is recommended for children aged 8 to 16 years, since it is during this period that active growth of the eyeball occurs. The main indications for the operation are:
- Progressive myopia, in which vision loss is no more than 1 diopter per year. As a rule, surgery is recommended for patients who have a moderate to high degree of disease (-4 - -6 D).
- When the eyeball grows in the anteroposterior direction.
In some situations, eye scleroplasty may be recommended for women who have a high degree of myopia when planning pregnancy or before giving birth naturally. This operation helps strengthen the sclera and reduces the risk of retinal detachment during delivery.
Contraindications include the following:
- The operation should not be performed on children under 8 years of age due to the risk of re-development of myopia due to the active growth of the eyeball.
- The formation of scar tissue on the surface of the eyeball can make it difficult to apply the strengthening material evenly.
- Exacerbation of chronic diseases caused by deterioration of the patient's condition during surgery.
- An inflammatory process in the internal environments of the eye, which can lead to large-scale damage to internal structures - endophthalmitis.
- Viral or bacterial infections, which are accompanied by a decrease in general immunity. This factor can aggravate recovery during the postoperative period.
After a viral or bacterial infection, scleroplasty can be performed 7-10 days after the clinical picture disappears and the patient’s condition stabilizes. If sensitization to certain materials used during scleroplasty is detected in a child, the issue of further surgical intervention is decided individually.
As a rule, before surgery, allergy tests are prescribed to determine individual sensitivity to the materials used.
Cost of the operation
The cost of scleroplasty averages 8-15 thousand rubles for surgery on one eye. The final price will depend on the clinic, the doctor, the material used for strengthening, and the surgical technique.
It is recommended to perform the operation only in certified and reliable institutions. In general, most patients after scleroplasty are satisfied with the result.
Any eye surgery is a risk. However, sometimes the benefits of scleroplasty outweigh the possibility of complications. Despite the fact that throughout the world such an operation for the treatment of myopia is rarely used, in the CIS countries it has allowed many people to see.
Sources used:
- Belyaev, V.S. Operations on the cornea and sclera / V.S. Belyaev. - M.: Medicine, 1984.
- Brovkina, A.F. Orbital diseases / A.F. Brovkina. - M.: Medical Information Agency, 2008.
- Kanski, Jack Clinical Ophthalmology. Systematized approach. Chapter 13. Glaucoma / Jack Kanski. - M.: Logosphere, 2010.
- https://niigb.ru/