Methods for measuring eye pressure
Intraocular pressure is usually measured during a comprehensive ophthalmologic examination. Palpation is used to roughly determine the IOP level. When the patient looks down with the eyelids closed, light pressure with a finger on the upper eyelids can determine whether the pressure is low or high. The differences between the right and left eyes are then compared. Palpation is used when it is not possible to use a measuring device (for example, after corneal transplantation).
Various devices based on different measurement principles are used to measure intraocular pressure. Today, there are 2 main types of tonometers used - contact and non-contact.
Non-contact tonometry
Most often, a patient sees an ophthalmologist using the applanation non-contact method, in which a special air tonometer releases a stream of air to the eye. This pressure flattens the cornea and, according to the measured parameters, determines the IOP values. For the patient, the examination is not burdensome, it is very quick, and is carried out in a sitting position, without contact with the eyes. The method is painless.
Contact tonometry
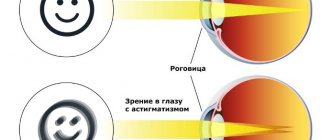
When using contact applanation tonometers, intraocular pressure is measured by touching the eye (after corneal anesthesia). The device applies pressure to a given area of the cornea necessary to straighten it, directly proportional to the IOP. But measurement results using these types of instruments may not be entirely accurate. They are affected by the shape of the eye, the thickness of the cornea, diseases, and previous surgeries.
Measuring eye pressure through the eyelids
Tonometers that measure IOP through the eyelids are more suitable for screening examinations. Since it is not possible to provide daily intraocular pressure measurements as part of an ophthalmologic examination, devices have been developed to measure IOP even at home. When using this method, there is no direct contact with the eye, no anesthesia is required, and there is no risk of infection. In some serious cases where classical methods cannot be used, transpalpebral tonometry is the best choice.
Contraindications to the use of other tonometers include:
- corneal edema;
- corneal erosion;
- corneal transplantation.
But the accuracy of these devices is lower compared to other tonometers.
Causes of changes in intraocular pressure
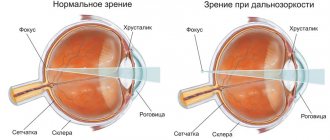
Normal intraocular pressure (10-21 mmHg) is important for the proper functioning of the eye and maintaining good vision.
IOP levels are influenced by various factors, including the following:
- Age
. Pressure in the eyes increases with age. - Floor
. Some studies show that women are more likely to suffer from ocular hypertension. - Genetics
. Inheritance has some influence, but the extent of its role has not yet been clearly demonstrated. - Corneal thickness
. Ocular pressure values can be strongly influenced by central corneal thickness. A thinner cornea helps to reduce IOP, while a thicker one helps to increase it. - Changing body position
. When changing from a sitting position to a lying position, the pressure in the eyes increases by approximately 1-6 mmHg. In people with glaucoma, these changes are more significant. - Influence of eyelids and eye movements
. Winking, strong squeezing of the eyelids, or, conversely, opening them wide can increase IOP. - Anesthesia
. During general anesthesia, intraocular pressure decreases. - Change during the day
. IOP values fluctuate throughout the day. It is important to monitor the size of these changes. The greater the change, the greater the likelihood of developing optic nerve damage. Deviations of no more than 8 mmHg are considered normal changes in values. The highest values are observed in the morning. This is due to hormone fluctuations. In patients with glaucoma, on the contrary, the highest rates are recorded in the daytime and evening. Therefore, it is necessary to measure the so-called. daily curve of values (at least 12 measurements are taken during the day). - Change during the year
. IOP increases slightly in winter due to atmospheric pressure and other factors such as light. - Cardiovascular factors
. After many years of research, a correlation has been determined between intraocular pressure and blood pressure. When blood pressure rises, there is a slight increase in pressure inside the eyes. - Sports
, physical overexertion. Strenuous exercise can temporarily reduce eye pressure. This is due to acidosis and changes in osmolarity. - Life style
. An increase in IOP can cause an increase in body mass index, cigarette smoking, and stress. - Medicines and food
. Various substances can also affect the amount of pressure in the eyes. For example, anesthetics and alcohol slightly reduce performance due to a decrease in the amount of intraocular fluid and even mild dehydration. Caffeine, ketamine, and corticosteroids, on the contrary, increase the values.
Causes of IOP violation
If intraocular pressure readings deviate from the norm, then the causes of this pathological phenomenon may be different. Increased ophthalmotonus (ocular hypertension) is a common phenomenon that is mainly observed in elderly people suffering from the following diseases:
- chemical poisoning;
- VSD;
- thyroid dysfunction;;
- traumatic brain injuries;
- hypertensive crisis;
- heart defects, heart failure;
- ophthalmological diseases;
- obesity.
The following factors can provoke a decrease in eye pressure:
- diabetes;
- liver failure;
- pathologies of an infectious nature;
- inflammation of the eyeball;
- retinal detachment;
- low blood pressure;
- damage to the eyeball.
Ocular hypotension can develop due to complications after surgery on the organs of vision. If a deviation from the norm has been identified, then the first step is to determine the cause of this pathological phenomenon, and then select treatment.
Normal eye pressure in women
Intraocular pressure is determined by the relationship between the formation of intraocular fluid and its drainage. The norm for eye pressure in women is within the range of 10-21 mmHg, and the differences in values between the sexes are insignificant. In youth, IOP may be less than 10 mmHg, but this value increases with age. Values greater than 21 mmHg are the reason for examining the optic nerve, which may be affected by changes caused by glaucoma.
At a young age, the average values are (mmHg):
- 20-29 years old – 17.6;
- 30-39 years old – 15.5.
Fluctuations in IOP can be influenced by hormonal changes such as pregnancy and the menstrual cycle. At older ages, IOP increases, mainly due to hormonal imbalance mediated by menopause. At this time, values can be around 17.4 mmHg. (40-49 years old). Then sometimes a slight or significant decrease or, conversely, an increase in indicators (mmHg) is recorded:
- 50-59 years old – 16.3;
- 60+ years – 17-26.
Normal eye pressure in children
Intraocular pressure increases with age, so normal eye pressure levels differ between adults and children. In infants it is 8-11 mmHg, and at the age of about 4 years – 14 mmHg. Similar to adults, children also show fluctuations in values. IOP in adolescents is comparable to that of adults.
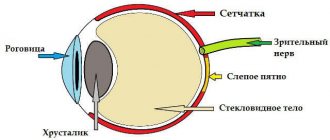
Before age 3, increased pressure in the eyes usually results in an enlarged eyeball (hydrophthalmos). Without treatment, severe, irreversible damage to the nerve fibers of the retina and optic nerve occurs, followed by a decrease in visual function. Early surgical and medical treatment in a specialized clinic can optimally maintain near-normal vision, but the prognosis is usually uncertain.
{banner_horizontalnyy3}
Acute increase in IOP
Typically, intraocular pressure during glaucoma rises gradually, and no sharp deterioration in vision is observed. But in the acute form of the pathology, a sharp jump in indicators is possible, which can be caused by the following factors:
- oxygen deficiency of the optic nerve;
- drinking excessive amounts of water;
- ocular circulatory disorders;
- severe stressful situation;
- long, identical work with the head tilted;
- excessive physical or psycho-emotional stress;
- being in the dark for a long time, when you have to strain your eyes, trying to see something.
A sudden jump in IOP can occur during surgery, accompanied by an increase in pupil size. In advanced forms of glaucoma, these factors can provoke an acute increase in pressure, accompanied by severe pain and loss of vision. The critical level is 60 mmHg. Art.
Read in a separate article: Open-angle glaucoma of 1 and 2 degrees: causes, symptoms, treatment and prevention
Normal eye pressure for glaucoma
Glaucoma is caused by increased intraocular pressure due to obstruction or dysfunction of absorption. An increase in IOP causes a decrease in vascular perfusion pressure in the optic nerve papilla. This leads to dysfunction and death of retinal ganglion cells.
Clinical manifestations and pressure indicators in the eyes depend on the degree of the disease:
- I degree. As a rule, the patient is bothered by a headache (increase in readings up to 30 mmHg).
- II degree. Irrigation occurs: the patient sees rainbow circles around the light (pressure above 30 mmHg causes corneal edema, and Newton's rings form around point light sources).
- III degree. Deterioration and blurred vision occurs (pressure of about 50 mmHg reduces retinal perfusion and, consequently, its function).
- IV degree. There is a critical increase in IOP (up to 70 mmHg), leading to blindness.
If your doctor talks about the risk of developing glaucoma due to increased pressure in the eyes, this is not a reason to panic. With a slight excess of 21 mmHg. or a thick cornea in the absence of signs of damage to the optic nerve, we are not talking about glaucoma.
Many people suffer from ocular hypertension without harming their vision. However, regular monitoring is required, preferably by repeat imaging of the optic nerve.
Diagnostics
A specialist can determine the cause of the feeling of pressure on the eyes. The doctor finds out complaints and the presence of chronic diseases. If there is pressure on a person’s eyes at the time of consultation, the doctor measures what the person’s blood pressure is at the moment.
Then the ophthalmologist examines the visual organ, measures IOP, and assesses the condition of the fundus using biomicroscopy and ophthalmoscopy. If space-occupying formations are suspected, the doctor may prescribe an ultrasound of the eyeballs, MRI, or CT of the eye orbits.
The combination of pressure on the eyes from the inside and dizziness, headache, confusion, nausea indicates the presence of diseases of other organs.
An ophthalmologist will help you determine which specialist you need:
- neurologist;
- endocrinologist;
- therapist;
- cardiologist;
- oncologist;
- neurosurgeon.
How to reduce eye pressure
Glaucoma is a virtually incurable disease. Therefore, it is better to promptly reduce increased intraocular pressure, thereby minimizing associated problems, such as pain in the head and eyes.
Methods for reducing IOP include:
- Eye drops. When diagnosing high pressure in the eyes, the doctor prescribes drops, the purpose of which is to reduce the amount of eye fluid or improve its outflow.
- General treatment. If the drops do not work or are poorly tolerated, there is an alternative in the form of tablets. But the medications may have side effects such as frequent urination, tingling, nausea or kidney stones.
- Surgical intervention. The final way to achieve better drainage of the fluid is by surgical or laser treatment of the drainage area.
Lifestyle change
You can influence the amount of intraocular pressure by changing some habits:
- Physical exercise. Cardio training improves blood circulation throughout the body, including the retina and optic nerve.
- Healthy eating. Include more leafy vegetables, foods rich in omega-3, vitamins C, E and A in your diet.
- Elevated head position during sleep. Sleeping on a high pillow at an angle of about 20 degrees can also help lower IOP.
- Herbal mixtures. Blueberries or ginkgo biloba are plants that can lower intraocular pressure. But it should be remembered that they do not replace medications prescribed by an ophthalmologist.
- Relaxation. Stress is one of the factors that causes increased IOP, so spend a few minutes every day doing meditation, yoga, or other relaxation techniques.
- Caffeine. Reducing the amount of caffeine in your diet is generally beneficial. One of the reasons for increased pressure in the eyes is excessive caffeine consumption.
Because the increase in intraocular pressure is not apparent at first, it is difficult to recognize. Therefore, undergo regular preventive examinations; If you experience problems with your vision, consult an ophthalmologist outside of routine examinations.