Main visual impairments in multiple sclerosis
With multiple sclerosis, patients often consult a doctor about visual disturbances. Their appearance is associated with the structural features of the optic nerve. The process is usually one-way. The doctor pays special attention to visual impairments, because this point is the most important in making a diagnosis and choosing the optimal treatment method.
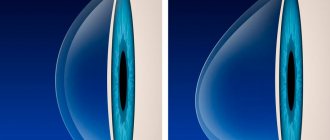
Rapid decrease in visual acuity
It can be insignificant (fogging of the visual field or changing the contours of objects) to complete loss, when the patient does not distinguish light. A person does not notice this kind of disorder for a long time precisely because of the one-sided nature of the lesion.
The process of reducing visual acuity varies over time.
Feeling pain
This is a fairly common complaint. Painful sensations occur mainly during movement of the eyeballs. Unpleasant sensations have no connection with physical stress and do not depend on the time of day. The patient may feel discomfort at night, and then his sleep worsens.
In rare cases, eye pain is combined with unpleasant sensations in the head of varying degrees of severity and intensity.
Change in visual field
Sometimes the patient sees spots, clouds and other objects in front of him. There is a persistent desire to get rid of them. Sometimes a person cannot see the image through the blur.
A person notices that his vision noticeably deteriorates in bright lighting conditions. Due to high sensitivity to light, glare appears and the perception of color changes. In some cases, patients note the presence of flickering, “fireworks”. Sometimes it happens that a person cannot determine the volume of an object because he sees it in a plane.
With physical activity, these symptoms intensify. This also occurs as a result of taking a bath, visiting a bathhouse or sauna. Even a short run can worsen your eye condition.
First symptoms of the disease
PC is not a homogeneous disease. Most patients at the time of diagnosis suffer from a relapsing-remitting form. They experience worsening symptoms followed by improvement. At this time, immune cells attack the myelin. This may take several days, weeks, months, and may be mild or very acute. During the period of remission of the disease, symptoms decrease or may almost completely disappear. It should be noted that the symptoms are gradual; with each new exacerbation, as a rule, new symptoms appear, along with the old ones, while the old ones are usually more pronounced with each exacerbation.
However, after several disappearances, permanent myelin damage and disability often occur. In most patients, the relapsing-remitting form turns into a secondary progressive form. Then the ailments are almost constant and gradually intensify. The rarest form of primary multiple sclerosis is primary progressive. Typically, this form of the disease occurs in people who become ill at a late age (35 years and older), and more often occurs in men. The course of the disease occurs without clear intervals and quickly leads to disability.
Frequent patient complaints
People suffering from multiple sclerosis are more likely to have the following complaints:
- the appearance of fog before the eyes;
- pain;
- inability to correctly determine the distance to an object;
- presence of foreign objects in the field of view;
- significant deterioration in condition after taking a hot bath;
- loss of a portion of the visual field;
- “kaleidoscopic” vision;
- uncontrolled eye movements - nystagmus;
- doubling of objects;
- sensation of constant presence of a foreign body.
Multiple sclerosis (MS) is a disease with multifocal damage to the central nervous system (CNS). As is known, the classic manifestations of MS are signs of damage to the pyramidal, sensory and cerebellar systems, involvement of the cranial nerves and also pelvic disorders [1-3]. These clinical symptoms occur in various combinations, reflecting the localization of demyelination foci in the brain and spinal cord. Nevertheless, there are “typical” and “atypical” symptoms for MS [3]. If typical symptoms help a clinician diagnose MS, then atypical ones force them to look for other causes of their occurrence, and MS becomes a diagnosis of “exception”. One of the “atypical” manifestations of MS is extrapyramidal movement disorders. In the literature there are rare descriptions of spastic torticollis [4, 5], chorea, dystonia [6], and tremulous hyperkinesis in MS [7]. A few articles are devoted to myoclonus [8-12]. In our clinical practice, we encountered such an unusual manifestation of MS as spinal myoclonus. Because this is a very unusual manifestation of MS, it may be of interest to specialists.
Patient A.
, 33 years old, works as an engineer, left-handed. From the life history: the patient’s heredity is not burdened. At the age of 10, he noted the development of weakness and a feeling of numbness in the left extremities, for which he was hospitalized in the neurological department of a children's hospital with a diagnosis of “Acute cerebrospinal circulatory disorder.” As a result of the treatment, the symptoms completely regressed within six months, after which nothing bothered the patient.
About 3 years ago, at the age of 30, the patient noticed periodic “twitching” in the left hand, forearm and shoulder. Such twitchings were observed 2-3 times a week, with purposeful movements, were spontaneous and became more frequent with excitement. The patient was unable to restrain or reduce these violent movements by any means or effort of will. Bright lights and loud sounds also had no effect on the twitching. Since the severity of violent movements, according to the patient, was not significant, he did not seek medical help. Over time, twitching in the left hand began to occur more often, sometimes regardless of active movements; they already bothered the patient at rest and persisted during sleep. The increase in the amplitude of violent movements forced the patient to leave work and seek medical help. Twitching increased during emotional stress and decreased after drinking alcohol. Other external factors did not influence them. The patients had no attacks with loss of consciousness.
When examining the patient's somatic status, no pathology was found. During a neurological examination, a slight disturbance of the associated movements of the eyeballs without double vision and nystagmus was recorded, and a slight smoothing of the right nasolabial fold was observed. Hyperesthesia of the feet on both sides from the level of the ankle joints, hypoesthesia of the left little finger of the hand and the lower third of the inner surface of the left forearm were detected, and the patient did not make active complaints about changes in sensitivity. Vibration and muscle-joint sensation was intact, muscle strength was sufficient. Tendon reflexes from the upper extremities were normal, with a vague predominance on the left; the knee and Achilles reflexes were brisk. Plantar reflexes were of the flexion type; abdominal reflexes were absent. The patient performed the finger-nose test on the left with kinetic tremor, without an intention component. Tandem walking was not impaired. Dysdiadochokinesis, Babinski asynergia and pelvic disorders were not detected.
Violent movements were recorded in the shoulder girdle on the left and left arm - jerky twitching in the form of a sharp alternating contraction of the muscles of the shoulder, forearm, wrist extensors and finger flexors, which led to the periodic occurrence of either moderate (20-25°) extension in the shoulder, or flexion in the elbow (10-15°), then to simultaneous extension in the wrist joints and flexion of the fingers. Hyperkinesis manifested itself especially clearly when stretching the arms forward and holding them in this position, with a frequency of up to 10 per minute. At rest, rare hyperkinesis of the above-described nature, but of significantly lower amplitude, was detected. Hyperkinesis prevented the patient from making precise movements; he was unable to write his last name. Sharp noise (clapping hands), tapping (on muscles, tendons) and light did not cause an increase in myoclonus.
Laboratory tests of blood and urine were normal. According to the results of magnetic resonance imaging (MRI) of the brain and spinal cord, multiple foci of demyelination measuring 3-7 mm, hyperintense on T2-weighted images (T2-WI) and hypointense on T1-weighted images (T1-WI), localized in white matter of the cerebral hemispheres, periventricular and subcortical regions, corpus callosum. A similar single lesion was observed in the right hemisphere of the cerebellum (Fig. 1)
.
Figure 1. MRI of the brain.
Multiple foci of demyelination, hyperintense on T2-weighted images. a - localized in the white matter of the cerebral hemispheres, periventricular and subcortical regions; b - a similar single focus is recorded in the right hemisphere of the cerebellum; c — lesions periventricular and in the corpus callosum; d — MRI after 3 months, compared with previous results, the appearance of new foci of demyelination was revealed; the focus at the posterior horn of the right lateral ventricle accumulates contrast agent. At the level of the C2 segment, 2 intramedullary lesions without clear contours were identified, slightly hyperintense on T2-weighted images and isointense on T1-weighted images, measuring 4x6 and 4x7 mm. The presence of a similar lesion at the level of segments C4-C5 and C5-C6 of the cervical spinal cord could not be excluded (Fig. 2)
.
Figure 2. MRI of the spinal cord.
At the level of the C2 segment, 2 intramedullary lesions are identified without clear contours, slightly hyperintense on T2-weighted images; the presence of similar lesions at the level of segments C4-C5 and C5-C6 of the cervical spinal cord cannot be excluded (indicated by arrows). Electroencephalography revealed no pathology. During involuntary contractions of the muscles of the left arm, no pathological changes were recorded on the EEG. Needle electromyogram (EMG) revealed discharges from several motor units of the m. extensor dig. com.
on the left (segment C7), discharge duration 70 ms and amplitude 1400 μV.
When conducting research in other muscles innervated by other segments, no answers were obtained (Fig. 3)
.
Figure 3. Needle EMG. Discharge with m.
extensor dig. com. lasting 70 ms and amplitude 1400 μV (responses were not obtained in other muscles from other segments). Stimulation EMG revealed a disturbance in the conduction of the motor fibers of the left arm at the elbow level (tunnel syndrome); no changes were found in the nerves of the left arm.
Thus, the patient was examined during an episode of deterioration in neurological status. This episode occurred in a young man (33 years old) with no previous or concomitant infection/fever. The detection of 2 or more signs of multifocal damage to the central nervous system during examination and the identification of lesions typical for MS on neuroimaging (subcortical, periventricular, infratentorial and in the spinal cord) [13] allowed us to settle on the diagnosis of “probable multiple sclerosis”. An episode that occurred in childhood (weakness and numbness on the left side) may have been the first attack of MS (although it is not documented). If this is so, then we are dealing with the onset of MS in childhood. The patient received standard pulse therapy with glucocorticosteroids and on the 3rd day of treatment noted a decrease in the frequency of twitching. Objectively, myoclonic hyperkinesis was recorded in the left hand, which was more postural in nature and appeared with a frequency of 8-10 per minute; twitching was not detected at rest. After 1 month, myoclonus stopped completely.
To verify the dissemination of the pathological process over time and establish a reliable diagnosis of MS, the patient underwent a repeat MRI examination of the brain after 3 months. Compared with previous MRI results, new foci of demyelination were noted on the left in the periventricular region and at the posterior horn of the right lateral ventricle; when contrast was administered, the last lesion accumulated contrast agent (omniscan) (see Fig. 1)
. According to the McDonald criteria [13], the patient was diagnosed with relapsing-remitting MS. After 3 months, no hyperkinesis was detected in the hand.
Considering the presented observation, it should be noted once again that spinal myoclonus (SM) is a rather rare form of hyperkinesis. They can be divided into segmental and propriospinal [14-19]. This division is based on the segmental structure of the spinal cord and the connections of the segments through the propriospinal tract. Spinal segmental myoclonus (SSM) is an involuntary movement involving hyperkinesis of muscles innervated by one or more adjacent segments of the spinal cord [17, 20–22].
In the above observation, myoclonus was localized in one arm. If we analyze the entire kinetics of the existing hyperkinesis, then the movements that constituted the hyperkinesis, namely shoulder extension (m. deltoideus, m. supraspinatus)
;
flexion at the elbow joint ( m. biceps brachii, m. brachialis, m. brachiradialis
);
extension of the hand ( m. extensor carpi radialis longus, m. extensor carpi radialis brevis, m. extensor dig. com.
);
flexion of the fingers ( m. flexor digitorum superficialis
) was provided by muscles innervated by several adjacent segments C5-C7 [23]. Accordingly, the patient had SSM.
In most cases, SSM are symptomatic, and they are based on lesions in the spinal cord caused by some primary disease - infection [24-26], tumor [27], arteriovenous malformation [28], syringomyelia [16], acute disseminated encephalomyelitis [29], vertebral pathology [28], iatrogenesis [125], etc. [10, 30-35]. Let us recall that the observed patient had foci of demyelination at the level of segments C2, C4, C5, C6 of the cervical spinal cord, and it was these foci that could cause the occurrence of myoclonic twitching of a segmental nature (see Fig. 2)
.
Clinically, SMS are most often irregular or can be rhythmic with a frequency of 0.2-8 Hz and an intensity of 1-600 per minute [10, 16, 22, 30, 32, 36]. The amplitude is also varied - from barely noticeable contractions of individual muscles or groups of muscles to intense movements in the joints [8]. The topic of segmental myoclonus in MS is very poorly covered in the literature due to the rarity of this condition. J. Jankovic and R. Pardo [10] describe 5 patients with MS who exhibited segmental hyperkinesis of stem origin in the form of palatal myoclonus. Myoclonic hyperkinesis in a patient with MS in the case we observed was periodic, non-rhythmic, with an intensity of up to 10 times per minute and led to visual violent movement in the joints of the left hand.
Propriospinal myoclonus (PSM) is the second type of SM, which differs from SSM by the involvement of a larger number of muscle groups in hyperkinesis; along with the limbs, twitching is also observed in the trunk [15-19, 32]. This occurs due to the spread of pathological impulses along the propriospinal tract, and many segments of the spinal cord are successively involved in hyperkinesis [14, 19]. Unlike SCM, propriospinal twitches often do not have a specific etiology. Some authors [17] associate their occurrence with neck trauma, tumor, viral myelitis and psychogenic factors. The literature describes a case of Lyme borreliosis, which manifested itself clinically in the form of PSM [37]. With PSM, rhythmic or nonrhythmic axial flexion movements are observed, involving the neck, body, and limbs in hyperkinesis, with a frequency of about 1-6 Hz. Hyperkinesis usually occurs spontaneously, in a horizontal position on the back and can be provoked by cutaneous stimulation of the abdominal area or by inducing tendon reflexes [17, 19]. In the described patient, only one arm was involved in hyperkinesis, the trunk and lower limbs remained intact, which rather indicates the segmental nature of the lesion, without massive involvement of the propriospinal tract.
There is a single description of PSM in MS [11]. A patient with MS periodically, after previous sensitive sensations in the neck (tingling), developed spontaneous irregular twitching in the right shoulder and arm. Violent twitching spread to the trunk and hip flexors on the right side. On MRI, the authors identified lesions in the cervical segments C2, C3, C4. The authors explained the development of PSM by the fact that lesions in the white matter could lead to disinhibition of spinal activity, but they assumed that the cause could also be the hyperexcitability of the demyelinated axon, which in such a damaged state is capable of spontaneously or reflexively generating impulses of pathological muscle activity.
Both types of MS are characterized by the persistence of hyperkinesis during sleep and relative resistance to external stimuli - they do not increase under the influence of auditory, visual, tactile stimuli or motor activity [10, 14, 16, 27, 30], although there are descriptions of cases in the literature SSM with disappearance during sleep and sensitivity to external stimuli [22, 31, 32]. It is believed that as the disease progresses, a reaction to external influences may appear [15]. For SM, the postural component is more pathognomonic—increased hyperkinesis in a certain position, as well as worsening twitching during fatigue and emotional stress [31, 32]. The SMS observed in the patient under study persisted during sleep, were not dependent on auditory and visual stimuli, but increased due to emotional stress and fatigue, and decreased with alcohol intake.
The next important distinguishing feature of SM is the absence of pathological activity on the EEG. Joint EEG-EMG should exclude the presence of cortical hyperexcitability preceding muscle contraction [10, 16, 30]. In the case under consideration, the EEG did not show any foci of hyperexcitability, which made it possible with a high probability to exclude the cortical nature of hyperkinesis.
Surface EMG in SM reveals rhythmic or semirhythmic discharges that are usually synchronous with a stereotypical duration and frequency. EMG studies of SMS demonstrate discharges lasting more than 100 ms (up to 1000 ms) and limited to one or two adjacent myotomes. With SCI, myoclonic discharges can last from 50 ms to 4 s, they are formed from the abdominal and cervical segments and spread slowly rostrally and caudally, while the cranial muscles remain intact. PSM is characterized by a delay between discharges and their sequential propagation, which is due to the slow conduction of the impulse along the propriospinal tract [17, 30]. In the case we are describing, the duration of the discharge was 70 ms, which does not really correspond to the description of segmental myoclonus presented in the literature, but is more characteristic of propriospinal ones. However, neither clinically nor neurophysiologically we observed the spread of forced muscle contractions, which most likely excludes the propriospinal nature of myoclonus.
The observation we described demonstrates a clear picture of SSM in MS. The absence of epileptic activity on the EEG, the presence of discharges in the muscles of the left arm (segment C7), the involvement in hyperkinesis of the muscles of the left upper limb, the innervation of which is provided by 3-4 adjacent segments, and, finally, registration of foci of demyelination in the spinal cord, namely at the level of the segments C2, C4, C5, C6 of the cervical spine - all this confirms the spinal segmental nature of myoclonus. The cause of SSM most likely was foci of demyelination in the spinal cord. The disappearance of hyperkinesis after hormone therapy strengthens our hypothesis about the genesis of violent movements.
There are various hypotheses for the mechanism of development of SM [8, 21, 26, 31, 32, 38-40]. Considering that myoclonic hyperkinesis in the observed patient appeared occasionally at rest and manifested itself most clearly when maintaining a posture, the most likely variant of the development mechanism is based on the rupture of intersegmental connections by foci of demyelination in the spinal cord [18]. This could lead to local dysregulation of the gamma motor neuron loop with the subsequent emergence of spontaneous neuronal impulses in the spinal cord segments and the formation of myoclonic hyperkinesis. The location of the lesions relative to the gray matter of the spinal cord may have been important.
Thus, the main reference points for diagnosing SSM in the above observation can be: 1) involvement in hyperkinesis of a limited group of muscles innervated by several neighboring segments of the spinal cord; 2) the absence of influence of external stimuli (auditory, visual, tactile) and active movements on the severity of hyperkinesis; 3) preservation of hyperkinesis during sleep, their intensification under the influence of fatigue and emotions, the appearance of myoclonus in a certain position; 4) absence of hyperexcitability on the EEG; 5) pathological EMG activity of muscles in limited myotomes with an intensity of 70 ms.
Treatment of SSM, in particular in MS, involves treatment of the underlying disease - stopping the exacerbation with the use of glucocorticosteroids. If there is no effect, clonazepam is considered the drug of choice at a dose of up to 6 mg per day [10, 17, 18, 22, 30]. Baclofen therapy may improve nocturnal myoclonus in the legs [10]. The literature contains mention of the effectiveness of topiramate and levetiracetam in SM. Tetrabenazine is used when there is no effect from other drugs [10, 30]. It is possible to use drugs in combination, such as tizanidine, clonazepam and baclofen [38]. There are descriptions in the literature of the positive effect of botulinum therapy for SM [17, 18, 30].
In conclusion, we note that the above observation demonstrates SSM as one of the rarest manifestations of MS. The basis of this “atypical” symptom of MS was a focus of demyelination located in the spinal cord of the cervical region.
Medical therapy
Medicines play a significant role in the treatment of multiple sclerosis. The preferred intake of methylprednisolone drugs is Metipred, Urbazon, Medrol. These drugs are administered intravenously and by drip. From the beginning of treatment, the doctor selects high doses, and then slowly reduces the dosage of the drug until it is completely discontinued. In case of acute development of pathology, Dexamethasone is administered retrobulbarly.
For about 20 days, the ophthalmologist prescribes Dicinon - first retrobulbar, then intramuscularly or orally. In parallel, drugs with antioxidant effects are used - Emoxipin, Essentiale,
To eliminate edema, Dazix, Diacarb, and ethacrynic acid are prescribed. Anti-inflammatory drugs are prescribed internally. In order to improve blood circulation processes in the lesion, Dalargin is used intramuscularly.
After the inflammatory phenomena subside, Cerebrolysin, Nootropil, Cavinton, Stugeron, Complapin are prescribed. Therapeutic measures are carried out jointly with a neurologist.
Anti-inflammatory drugs are used to treat nystagmus. Additionally, the doctor uses special lenses and bandages.
With adequate treatment, the symptoms of visual impairment gradually disappear. With a favorable course of the disease, complete remission can be achieved. Patients require constant monitoring by a neurologist and ophthalmologist. Treatment of optic nerve atrophy is extremely complex and lengthy.
Author's rating
Author of the article
Alexandrova O.M.
Articles written
2029
about the author
Was the article helpful?
Rate the material on a five-point scale!
If you have any questions or want to share your opinion or experience, write a comment below.
Most common signs and symptoms
Each of the PC signs has its own characteristics. In this case, we can only identify groups of symptoms that are most characteristic of multiple sclerosis. The initial symptoms, the rate of progression, the severity and combination of different groups of symptoms are presented differently in each person. The following groups of symptoms should be distinguished:
- Are common. These include fatigue, fatigue, and decreased performance. Patients claim that at the moment of weakness they feel as if someone had suddenly “pulled the plug from the power supply.” General fatigue appears without warning and also disappears unexpectedly. In some people, at the moment of fatigue, for example, the limbs (arms, legs) become so heavy that they cannot make the slightest movement. Often fatigue is associated with changes in weather, temperature (overheating) in the apartment or physical exercise. It can occur with infections associated with fever;
- Visual disorders. They are one of the early symptoms of PC, although not all patients have them. The most common disease is optic nerve dystrophy. Visual impairment is usually transient. During the day, double vision, decreased visual acuity, loss of visual fields and other various signs may develop. As a rule, in the period between exacerbations, vision is completely restored;
- Pain. May be acute or chronic. Neuropathic pain occurs as a result of damage to the nerve fibers of the brain and spinal cord. The patient feels tingling, numbness, trembling in the limbs, burning, “flies crawling under the skin,” as if a sudden electric shock. Daily stress and stress on the body contribute to musculoskeletal pain. There is a loss of muscle strength and function, stiffness and cramps. The patient has difficulty moving his hips and spine. They have problems with changing posture, walking, coordination of movement, everyday activities (dressing, washing);
- Pelvic disorders. In MS, the transmission of signals along the nerve pathways to the bladder is disrupted. The patient has difficulty maintaining urine or emptying the bladder. It happens that when the nerve tracts of the spinal cord are damaged, the bladder contracts even with a small amount of urine (the so-called instability of displacement), causing constant urge. Often there is an inability to hold urine. In the second type of trouble, the bladder sphincter does not relax while the muscles contract. This causes a weak, intermittent flow of urine and an inability to completely empty the bladder. It happens that the patient loses control of the rectal sphincter;
- Psychological symptoms. This group of symptoms is an awareness of the severity of the condition, often the presence of pelvic functions and vision problems. However, it should be noted that there is sometimes the presence of the so-called “euphoria of multiple sclerosis.” At the same time, the patient is not critical of the disease, makes rosy plans for the future, and often refuses treatment.